Therapeutics: Platelet Coagulopathy Fixes with ITP, TTP and DIC
/A CBC is one of the most common ED lab studies obtained, and while this “basic lab” is something that is often ordered reflexively, perhaps to check for anemia or leukocytosis, the sometimes-forgotten third major component of this test is the platelet level. In this post, we’re going to discuss three important platelet disorders, all hallmarked by thrombocytopenia, that the ED provider should be familiar with – Immune Thrombocytopenia (ITP), Thrombotic Thrombocytopenic Purpura (TTP), and Disseminated Intravascular Coagulation (DIC).
+ Why Do we Care about Platelets?
Vasoconstriction
- Vascular injury exposes endothelial cells, which release endothelin, causing smooth muscle contraction and vasoconstriction
Adhesion
- Von Willebrand Factor binds exposed subendothelial collagen to GP1b receptor on platelets, linking platelets to the stie of injury
Activation
- Binding of vWF to GP1b activates the platelet, causing a conformational change that exposes the GPIIb/IIIA receptor and causes platelets to degranulate and release coagulation factors
Aggregation
- Newly exposed GPIIb/IIIA receptor then binds fibrinogen, which “glues” multiple platelets together and forms a weak platelet plug
This weak platelet plug later gets strengthened via the generation of thrombin by the coagulation cascade. 1
+ What exam findings should clue you in to a potential platelet disorder?
Recall that a thorough skin exam is important for patients reporting bleeding symptoms or with suspected platelet disorders. [2]
Petechiae
- Result from bleeding into the skin from broken capillaries
- Red, flat, and discrete
- Non-blanching (blood is already in the extracellular space, can’t “push” it around with pressure)
- < 2 mm in size
- Often occur in dependent areas, but can occur anywhere, including the mucosal surfaces
Purpura
- Coalesced petechiae
- 2-10 mm in size
- Usually non-palpable and dependent in thrombocytopenia, but can be palpable in vasculitis due to capillary inflammation
- Skin purpura = “dry” purpura; Mucosal purpura = “wet” purpura
Ecchymosis
- Subcutaneous accumulation of extravasated blood
- Non-palpable, skin is flat
- Measure >1 cm in size
- Ecchymoses of varying ages helps indicate an ongoing process rather than an acute traumatic event
Hematoma
- Extravascular collection of blood
- If subcutaneous, may raise the skin profile and be palpable
- Can occur within the deep tissues, e.g. muscle, retroperitoneal space, and joints
| Pathophysiology | Examples | Description |
|---|---|---|
| Decreased Platelet Production | Bone marrow disorders (viral infection, cancers, nutrient deficiencies, etc.) | Improperly functioning marrow → Platelets unable to be produced from megakaryocytes |
| Liver disease (cirrhosis, hepatitis, etc.) | Impaired liver synthetic function → decreased TPO production → marrow is not stimulated to produce platelets | |
| Peripheral platelet destruction | Autoimmune destruction (ITP, Evans Syndrome, etc.) | Anti-platelet antibodies may be formed idiopathically or in response to another autoimmune condition, leading to platelet destruction |
| Drug-induced | Certain medications (e.g. quinine) can induce the production of anti-platelet antibodies | |
| Platelet consumption in thrombi | TTP, DIC, HUS | In certain conditions, widespread thrombosis causes consumption of all available platelets |
| Dilution | Massive transfusion or massive fluid resuscitation | If giving a large amount of fluid or blood, it is important to proportionately transfuse platelets to avoid dilutional thrombocytopenia |
| Sequestration | Splenomegaly, splenic congestion, portal hypertension | In healthy individuals, the spleen carries approximately one-third of the platelet mass within the body. If the spleen is larger than usual or has congestion due to portal hypertension or vascular disease, the circulating peripheral platelet count is decreased even if total body platelet mass is normal |
Idiopathic Thombocytopenic Purpura (ITP)
Pathophysiology
Defined as an acquired thrombocytopenia with a platelet count <100 caused by immune destruction of platelets [4]
Disease of platelet quantity – the remaining platelets function normally, there are just not enough of them
Up to 60-70% of patients with ITP will have IgG antibodies that are platelet-specific, usually against glycoproteins on the platelet surface such as GPIIb/IIIa or GPib/IX/V4
Primary ITP (80%)
Platelets are destroyed by pathologic anti-platelet antibodies, impaired megakaryocyte production, and/or T-cell mediated destruction of platelets [4]
No apparent triggering mechanism or underlying condition
Secondary ITP (20%)
ITP that arises after an inciting event that appears to predispose to antibody-mediated platelet destruction
Causes of secondary ITP are numerus, but include:
Autoimmune conditions (SLE, rheumatoid arthritis, antiphospholipid syndrome, CVID, etc.)
Infections (MMR vaccination, H. pylori infection, HIV, Hepatitis C, CMV, VZV, COVID-19, and others)
Medications [4,5]
Clinical Presentation
The most common presenting symptom is mucocutaneous bleeding
Ex: nose bleeds and gum bleeding, may also manifest as heavy menstrual bleeding in females [6]
Petechiae and purpura are more commonly seen in the dependent extremities, can wax and wane over days [6]
Rarely can present with severe bleeding or intracranial hemorrhage [6]
Diagnosis
ITP is a diagnosis of exclusion [6]
Initial work-up should include [7]:
CBC to rule out additional causes (thrombocytopenia should be isolated in ITP without anemia or pancytopenia)
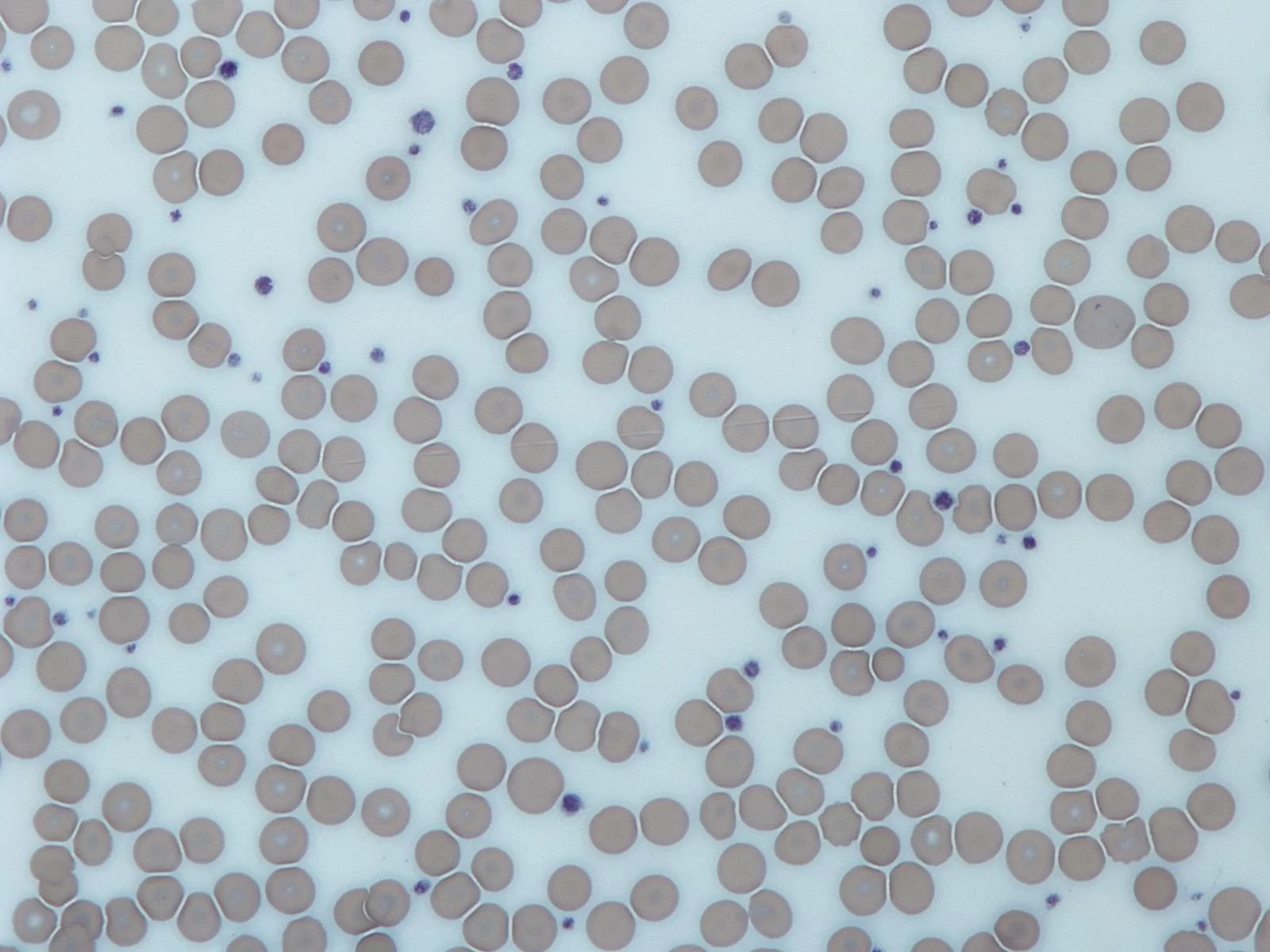
Peripheral blood smear to rule out additional causes, i.e. schistocytes indicating a hemolytic process, platelet agglutination causing pseudothrombocytopenia, etc.
HIV and HCV testing, as thrombocytopenia is a common presenting sign of these illnesses
Initial Treatment
The goal of initial treatment is to prevent significant bleeding, not to normalize the platelet count. Based on the 2019 International Consensus Report on ITP, treatment is stratified based on the patient’s bleeding severity and their risk of bleeding, not the platelet level: [7]
Critical bleeding (e.g. threat to life, limb, or sight)
Bleeding into a critical anatomic site or bleeding causing hemodynamic instability or respiratory compromise
Can include intracranial, intraspinal, intraocular, retroperitoneal, pericardial, or intramuscular bleeding with compartment syndrome
Platelet count usually < 10,000
Platelet transfusions
Typical dose is 4-6 units of pooled platelets at a time, repeated as needed, because platelets may be consumed by the ITP-related destruction
IVIG
1 g/kg x1-2 days
Glucocorticoids
Dexamethasone 40 mg IV x4 days or methylprednisolone 1 g IV x3 days
Severe bleeding
Bleeding that results in a drop in hemoglobin of 2 g/dL or requires >1 unit pRBCs
Platelet count usually < 20,000
Glucocorticoids (preferred) or IVIG at the doses above, but both are not required
Minor bleeding
Skin or mucosal bleeding that does not meet criteria for critical or severe bleeding
Platelet count usually < 50,000
Glucocorticoids
Dexamethasone 40 mg PO or IV x4 days, or prednisone 1 mg/kg daily x1-2 weeks + gradual taper
Asymptomatic severe thrombocytopenia
Patients with a platelet count of < 20,000 but who are asymptomatic should be treated, as they are at high risk of bleeding
Based on risk-benefit analysis of the patient’s other comorbidities and bleeding propensity and shared decision making with the patient
A higher threshold, such as a platelet count of 30,000-50,000, may be used in patients > 60 years old or on anticoagulants
Can be treated with PO glucocorticoids at the doses above, similar to patients with minor bleeding
Disposition
Patients with critical or severe bleeding require admission, usually to an ICU setting
New ITP with platelets <10,000 generally requires admission
New ITP without significant bleeding with platelets >30,000 can be discharged with close hematology follow-up
New ITP with platelets 10,000 – 30,000 requires shared decision making to determine discharge with close hematology follow-up vs. admission
Based on the patient’s bleeding risk, comorbidities, and social support/ability to follow-up
Known ITP without bleeding can be discharged with close follow-up if the platelet level is >10,000
Thrombotic Thombocytopenic Purpura (TTP)
Pathophysiology
TTP results from a deficiency in an enzyme known as ADAMTS-13 [6]
ADAMTS-13 normally cleaves multimers of von Willebrand factor (vWF) into smaller monomers
When ADAMTS-13 is deficient, vWF accumulates on the endothelial surface and binds up platelets, causing widespread microthrombi accumulation in the microvasculature, leading to end-organ ischemia
In 95% of cases, TTP is caused by acquired inhibitory autoantibodies against ADAMTS-13, but it can rarely be genetic due to inherited mutations [9]
Like most autoimmune conditions, the underlying etiology is unclear on how TTP develops. Most cases are idiopathic with no identifiable inciting cause [6,9]
Clinical Presentation
The “classic” pentad of fever, hemolytic anemia, thrombocytopenia, renal dysfunction, and neurologic symptoms (“FAT RN”) rarely occurs and is unreliable [8]
The presenting symptoms vary widely based on the affected organ system(s), and can range from sequela of thrombocytopenia (fatigue, petechiae, bleeding) and hemolytic anemia (jaundice, dark urine) to evidence of end-organ ischemia [6]
Diagnosis
TTP is a clinical diagnosis, based on clinical features and laboratory testing [6,9]
A presumptive diagnosis of TTP can be made with findings of microangiopathic hemolytic anemia + thrombocytopenia without other obvious cause
All patients with suspected TTP need a CBC + peripheral smear [6,9]
Anemia is generally mild
Thrombocytopenia is usually severe, in the range of 20,000 – 50,000
Schistocytes on peripheral smear are required for diagnosis
Hemolysis labs are helpful to prove presence of a hemolytic anemia
Elevated reticulocyte count
Elevated LDH
Elevated indirect bilirubin
Decreased haptoglobin
Direct Coombs test to rule out autoimmune hemolytic anemia
Coags and type + screen
Other laboratory testing is aimed at finding evidence of end-organ damage
Creatinine/basic metabolic panel to look for renal dysfunction
UA
LFTs
Troponin (elevations seen in roughly 50% of patients with TTP)
EKG
CT head or MRI brain
Serum or urine HCG to determine pregnancy status
ADAMTS-13 activity testing can be sent from the Emergency Department, but this is often a send-out test and should not be relied upon for diagnosis
The PLASMIC score can be used to predict the likelihood of TTP in patients with already known thrombotic microangiopathy, although this was studied and validated in hospitalized patients, not in an ED setting, and has not been validated to rule out TTP9,10
1 pt each for:
Platelet count < 30,000
Hemolysis
Not treated for active cancer in the past year
No history of solid organ or stem-cell transplant
MCV < 90
INR < 1.5
Creatinine < 2
0-4 points = Low risk of severe ADAMTS-13 deficiency
5 points = Intermediate risk
6-7 points = High risk
Initial Treatment
Hematology should be involved once TTP is suspected
The primary treatment of TTP is plasma exchange therapy, also known as plasmapheresis [6,11]
Exchange therapy both removes the causative autoantibody and replaces deficient ADAMTS-13
Usually 1-2 plasma volume exchanges are performed per day
Reduction in all cause mortality compared to plasma infusions alone [6]
Fresh frozen plasma can be transfused if plasma exchange is not readily available [6]
Must be cautious to avoid volume overload in patients with renal or heart failure
Not as effective as plasma exchange because the causative antibodies remain
Despite the presence of severe thrombocytopenia, platelet transfusions are contraindicated, because they may actually worsen disease by contributing to additional microthrombi formation [6]
Additional treatment may be indicated as guided by hematology, but this generally will not occur in the ED setting [11]
Glucocorticoids and/or rituximab may be used as immunosuppressive agents to suppress autoantibody production
Caplacizumab is a monoclonal anti-vWF antibody that binds vWF and prevents its binding to platelets; it is reserved for especially severe or refractory cases of TTP, and may also be used for patient’s who decline blood products for religious or personal reasons
Disposition
Patients with TTP require admission to an intensive care unit for plasma exchange therapy or emergent transfer to a capable center
Disseminated Intravascular Coagulation (DIC)
Pathophysiology
DIC is hallmarked by a “consumptive coagulopathy” where the coagulation system is massively activated everywhere in the body, instead of locally at sites of tissue injury, such that coagulation factors ultimately get depleted, leading to simultaneous bleeding and clotting [12,13]
An initial insult exposes blood to large amounts of procoagulants, such as:
Lipopolysaccharides in gram negative bacteria
Trauma resulting in vascular endothelial damage that exposes the blood to procoagulant substances
Placental damage from trauma associated with pregnancy or retained products of conception, resulting in massive tissue factor (TF) generation
Cancer cells producing tissue factor (TF)
Severe intravascular hemolysis resulting in release of procoagulants from lysed cells
The coagulation cascade gets massively activated, leading to the formation of thrombi from platelets and fibrin
Fibrinolysis is activated at sites of thrombi, resulting in the generation of fibrin degradation products (FDP)
Platelets and coagulation factors get used up due to massive activation, and FDPs further interfere with clot formation and platelet aggregation, predisposing to bleeding
This process ultimately leads to a combination of thrombosis, bleeding, and end organ damage
It is important to recognize that DIC is not a specific disease, it is a manifestation of another underlying pathologic process [13]
Clinical Presentation
An appropriate clinical context, such as recent trauma, sepsis, or malignancy is important to make the diagnosis of DIC12,13
No clinical sign or symptom is highly specific for DIC, but acute DIC should be suspected in the appropriate clinical context if there is bleeding from 3 or more unrelated sites [12]
Bleeding may manifest as:
Oozing from sites of catheters or drains
Accumulation of blood in serous cavities post-operatively
Petechiae, purpura, and ecchymoses
DIC may also present with a variety of symptoms related to underlying organ dysfunction, including:
AKI/renal failure
Liver dysfunction
Neurologic dysfunction
Diagnosis
| Lab | Value | Points |
|---|---|---|
| Platelets | >100,000 | 0 |
| 50,000-100,000 | 1 | |
| <50,000 | 2 | |
| Fibrin marker (D-dimer) | Normal | 0 |
| Moderate Increase | 2 | |
| Severe Increase | 3 | |
| PT | <3s | 0 |
| 3-6s | 1 | |
| >6s | 2 | |
| Fibrinogen | >100 mg/dL | 0 |
| <100 mg/dL | 1 | |
Like the other thrombotic microangiopathies, there is no single test that can rule in or rule out DIC
Patients with suspected DIC should receive the following initial work-up:
CBC with peripheral smear should demonstrate anemia, thrombocytopenia, and schistocytes
PT/INR and aPTT will be prolonged due to the consumption of clotting factors
Fibrinogen is typically low in acute DIC, as it gets consumed to make thrombi. However, fibrinogen is also an acute phase reactant and may be massive elevated in states of sepsis or malignancy. Therefore, a fibrinogen in normal range may still represent massive consumption
D-dimer is typically elevated
Hemolysis labs will suggest a microangiopathic hemolytic anemia
Similar to cases of suspected TTP, patients with suspected DIC should undergo evaluation for associated end-organ damage
The International Society on Thrombosis and Haemostasis (ISTH) has developed a scoring system to aid in the diagnosis of DIC: [13,14]
This scoring system must only be used in patients with an underlying disorder known to be associated with DIC
A score of 5 or more suggests acute DIC
Initial Treatment
The only treatment for DIC is to reverse the underlying cause to remove the stimulus driving coagulation cascade activation
Additional supportive measures include:[12,13]
RBC transfusions for severe bleeding
Platelet transfusions should be used to maintain platelet count > 50,000 if there is active bleeding or > 20,000 without bleeding
Fresh frozen plasma or cryoprecipitate can be transfused to replete coagulation factors if serious bleeding is present and PT/aPTT are prolonged
Hemodynamic and respiratory support as needed
Despite the increased risk of thrombosis in patients with DIC, prophylactic anticoagulation is not typically recommended [12]
If venous thromboembolism is present, it should be treated accordingly
Disposition
DIC has a very poor prognosis with mortality upwards of 50%; patients with DIC or suspected DIC require admission to an intensive care unit for close monitoring and treatment
Summary of Lab Tests in Platelet Dysfunction
| Lab | ITP | TTP | DIC |
|---|---|---|---|
| Platelets | Decreased | Decreased | Decreased |
| Hemoglobin | Normal | Decreased | Decreased |
| Peripheral Smear | Low Plt otherwise normal | Schistocytes | Schistocytes |
| LDH | Normal | Elevated | Elevated |
| PT/PTT | Normal | Normal | Often Elevated |
| D-Dimer | Normal | Normal | Elevated |
| Fibrinogen | Normal | Normal | Decreased |
Post by Sarah Moulds, MD
Dr. Moulds is a PGY-1 in Emergency Medicine at the University of Cincinnati
Editing and Graphics by Allie Hunt, MD and Ryan LaFollette, MD
Dr. Hunt is a PGY-4 in Emergency Medicine at the University of Cincinnati. Dr. LaFollette is an Associate Professor of Emergency Medicine at co-editor of TamingtheSRU.com
References
Sattar, HA. Fundamentals of pathology. Pathoma, LLC. 2019
Ma, A. Approach to the adult with a suspected bleeding disorder. In: UpToDate. February 2021
Arnold DM and Cuker A. Diagnostic approach to the adult with unexplained thrombocytopenia. In: UpToDate. May 2021
Lambert ML, Gernsheimer TB. Clinical updates in adult immune thrombocytopenia. Blood 2017;129(21); 2829-2835
Arnold DM and Cuker A. Immune thrombocytopenia (ITP) in adults: Clinical manifestations and diagnosis. In: UpToDate. July 2021
Kappler S, Ronan-Bentle S, and Graham A. Thrombotic Microangiopathies. Emer Med Clin 2014;32(3); 649-671
Provan D, Arnold DM, Bussel JB, et al. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv. 2019;3(22):3780-3817
Page EE, Kremer Hovinga JA, Terrell DR, et al. Thrombotic thrombocytopenic purpura: Diagnostic criteria, clinical features, and long-term outcomes from 1995 through 2015. Blood Adv. 2017;1(10):590-600.
George JN and Cuker A. Pathophysiology of TTP and other primary thrombotic microangiopathies (TMAs). In: UpToDate. October 2021.
Bendapudi PK, Hurwitz S, Fry A, et al. Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: A cohort study. Lancet Haematology. 2017;4(4):157-164.
George JN and Cuker A. Immune ITP: Initial treatment. In: UpToDate. October 2021.
Leung LLK. Evaluation and management of disseminated intravascular coagulation (DIC) in adults. In: UpToDate. December 2021.
Boral BM, Williams DJ, Boral LI. Disseminated intravascular coagulation. Amer Jour Clin Path. 2016;146(6):670-680.
Toh CH, Hoots WK; SSC on Disseminated Intravascular Coagulation of the ISTH. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost. 2007 Mar;5(3):604-6.