Mastering Minor Care: Hand Injuries
/You look at the track board and see that a 36-year-old male has been roomed with hand pain. You may be thinking “Easy, I’ll get x-ray and this guy will be out of here in 30 minutes.” Or, you may be thinking “Oh no. There are like a million things that can go wrong with a hand. Please tell me hand surgery is in house!” While there is no way to cover everything that can go wrong with the hand, this post will cover some of the most common hand injuries and how to recognize and manage them in the emergency department.
Hand Exam
It is important to develop a quick and comprehensive hand exam when patients present with hand pain or injuries. This can be broken down into several key components:
Inspection: Look at that hand for any gross deformities or other abnormalities.
Assess for scissoring fingers when patient makes a fist as this can be indicative of an MCP or carpal fracture.
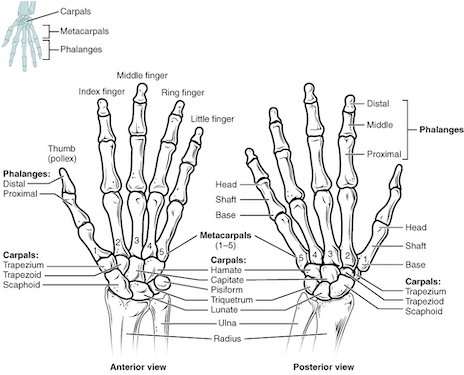
Palpation: Palpate all bones and joints to assess for tenderness, deformities, and crepitus (image 2).
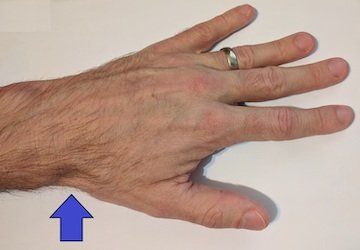
Check for anatomic snuffbox tenderness (image 1) to assess for occult scaphoid fractures
Circulation: Check for radial and ulnar pulses as well as capillary refill.
Complete Allen’s test to assess for collateral blood flow:
Have the patient make a tight fist with their hand while you occlude the radial artery
When the patient’s fist is released, the hand should turn pink with collateral blood flow from the ulnar artery
If it does not, the patient doesn’t not have adequate collateral circulation. This can also be used to assess radial collateral while occluding the ulnar artery. This is especially important if there is any concern for vascular injury.
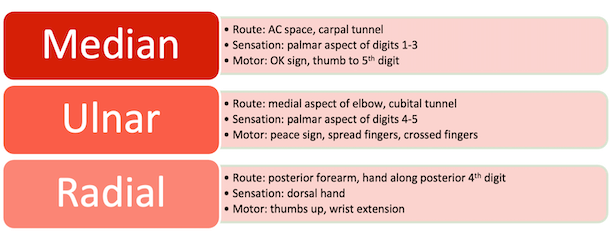
Nerve assessment: Each of these distributions should be tested to ensure that there is no underlying nerve injury.
Tendon assessment: Each tendon should be separately assessed in isolation.
Flexor digitorum profundus: have the patient flex the DIP against resistance
Flexor digitorum superficialis: the patient should flex the PIP against resistance
Extensor tendons: have the patient lay their hand flat on the surface and lift their fingers
Common Injuries
PIP Dislocations
The proximal interphalangeal (PIP) joint is located between the first and second phalanx of the fingers. It is comprised of multiple collateral ligaments that insert into various locations on the phalanx. The PIP joint can be dislocated in a dorsal, volar, or lateral direction. Dislocations are most commonly dorsal due to PIP hyperextension such as a ball striking a patient’s fingertip.
Exam findings: Deformity +/- skin puckering at PIP
There may be lateral laxity of the joint if tested in extension
Perform Elson’s test: have the patient extend the finger against resistance
It is abnormal and concerning for PIP dislocation if this results in DIP hyperextension.
Diagnosis: X-ray may show obvious dislocation. It may also show more subtle dorsal joint widening due to subluxation (“V” sign).
Management: Patient should undergo closed reduction of the joint in the emergency department followed by buddy taping for 3-6 weeks. Dislocations can lead to swan neck deformities or boutonniere deformities long term
MCP (Boxer’s) Fracture
The metacarpals are located between the carpal bones and phalanges. While any MCP can be fractured, a boxer’s fracture is a fracture of the fourth or fifth metacarpal (MCP) joint. This is usually due to an axial load on the fist such as punching a wall.
Exam findings: Swelling and tenderness present at MCP
Volar angulation of the MCP joint which will look like a missing 4th or 5th knuckle
Assess for scissoring of the fingers
Look for any associated abrasions or lacerations that may be consistent with a fight bite or open fracture
Diagnosis: Obtain AP and lateral views to assess for degree of angulation
Management: Closed reduction should be considered if the fracture meets the criteria as listed in the table below.
Most specialists recommend placement of an ulnar gutter splint however new research has shown that buddy taping has similar long-term outcomes to plaster casts with earlier return to work and a shorter ED stay. These patients should be referred to hand surgery as many need outpatient surgeries.
Lunate and Perilunate Dislocations
Image 5: lunate dislocation.
Lunate and perilunate bones are carpal bones. They are located next to each other in the proximal hand. These injuries are often associated with a high mechanism where the patient’s wrist was forcibly extended and deviated towards the ulnar aspect. Often these are missed on initial presentation but can have serious long-term consequences.
Exam findings: Tenderness throughout carpal bones, especially over lunate and perilunate. Assess median nerve function as this can be injured as a result of the injury.
Diagnosis: Up to 25% of these injuries are missed on AP x-rays so a lateral x-ray is key to diagnosis. X-ray findings include Gilula’s arc, piece of pie sign, and spilled teacup sign.
Management: Hand surgery should be consulted if possible as many need urgent surgical intervention and all need close follow up.
Distal Radius Fractures
Distal radius fractures are the most common orthopedic injury seen in the emergency department. There is a bimodal distribution of patients presenting with this injury including young persons with high energy mechanisms and elderly patients who often sustain fractures due to a fall on an outstretched hand. One should maintain a high index of suspicion for possible associated ligamentous injuries.
Exam findings: Tenderness at the distal radius with swelling and often deformity present at the wrist.
Diagnosis: AP and lateral x-rays should always be obtained. If there is concern for intraarticular involvement on x-ray, CT should also be obtained. If there is any clinical concern for ligamentous involvement the patient may also require outpatient MRI.
Colles’ fracture: dorsally displaced and extraarticular. Most common type of distal radius fracture. Usually elderly patient with FOOSH injury.
Smith’s fracture: volarly displaced and extraarticular. Due to a fall onto a flexed wrist or a blow to the back of hand.
Die-Punch: Depressed fracture of lunate fossa of distal radius due to an axial loading injury.
Barton’s fracture: Dorsal intraarticular fracture which is often associated with dislocation at the radiocarpal joint.
Chauffer’s fracture: Fracture of the radial styloid. This is usually due to a blow to the volar aspect of the wrist. These often have associated scaphoid or ligamentous injuries.
Management: Closed reduction and splinting should be completed in the emergency department. There are multiple ways to approach the anesthesia and reduction as listed below.
Anesthesia: Providers can give IV procedural sedation or attempt a hematoma block. Hematoma blocks are effective and do not increase risk of infection. To preform a hematoma block, enter the skin directly over the fracture and advance until hitting bone. Aspirate blood to confirm location in the hematoma before administering lidocaine. Ultrasound guidance may improve anesthesia.
Reduction: There are multiple methods of reduction including manual traction, finger trap traction, and active traction/counter traction. One 2018 meta-analysis showed that finger trap method is most effective for radial shortening with better pain control and fewer complications. Manual traction appears to be more effective for patients with dorsal tilt. Unfortunately, if first attempt at reduction fails it is unlikely to have successful reduction on the second attempt with only 5% of people requiring two attempts having acceptable final alignment on x-ray.
Splinting: After reduction patient should be placed in a sugar tong splint.
While many of these patients do well with closed reduction and splinting, there is also a subset of the population that with require surgical intervention that have significant % inclination of the radius, change in height of the radius or volar tilt. Hand surgery or orthopedics should be considered in these cases.
High Pressure Injuries
High pressure injuries are most common in young males, especially those in the pain, automotive, and diesel industries. Patient most often sustains the injury to their non-dominant hand. Initial injury will gradually lead to chemical irritation and inflammation, ultimately creating a nidus for secondary infection. The injury can also result in dissection along the neurovascular bundles, leading to vascular occlusion and soft tissue necrosis. High pressure hand injuries have a poor prognosis with up to half of patients requiring surgery including amputation. Poor prognostic factors include time to treatment, force of injury, volume injected, and composition of material.
Exam findings: Entry wound may look benign or have surrounding edema or pallor. If patient is seen later in symptom course, they may present with diffuse swelling or signs of necrosis.
Diagnosis: This is a clinical diagnosis. X-ray should be obtained to identify any radiopaque foreign bodies if present.
Management: Patient will require broad spectrum antibiotics, tetanus shot, and limb elevation in the ED. Hand surgery should be consulted emergently as most require surgical debridement and possible amputation.
Post by Bailee Stark, MD
Dr. Stark is a PGY-3 in Emergency Medicine at the University of Cincinnati
Editing by Bronwyn Finney, MD and james Li, MD
Dr. Finney is a PGY-3 in Emergency Medicine at the University of Cincinnati.
Dr. Li is an Assistant Professor in the Department of Emergency Medicine at Washington University of St. Louis
References
Grohmann A, Kaveman E, Gottlieb M, et al. Boxer’s Fracture. WikEM.
Handoll HH, Madhok R. Closed reduction methods for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003;(1). doi:10.1002/14651858.CD003763
Søsborg-Würtz H, Corap Gellert S, Ladeby Erichsen J, Viberg B. Closed reduction of distal radius fractures: a systematic review and meta-analysis. EFORT Open Rev. 2018;3(4):114-120. doi:10.1302/2058-5241.3.170063
Hofmeister EP, Kim J, Shin AY. Comparison of 2 methods of immobilization of fifth metacarpal neck fractures: a prospective randomized study. J Hand Surg. 2008;33(8):1362-1368. doi:10.1016/j.jhsa.2008.04.010
Pellatt R, Fomin I, Pienaar C, et al. Is Buddy Taping as Effective as Plaster Immobilization for Adults With an Uncomplicated Neck of Fifth Metacarpal Fracture? A Randomized Controlled Trial. Ann Emerg Med. 2019;74(1):88-97. doi:10.1016/j.annemergmed.2019.01.032
Karadsheh M. Lunate Dislocation (Perilunate dissociation). OrthoBullets.
Schermann H, Kadar A, Dolkart O, Atlan F, Rosenblatt Y, Pritsch T. Repeated closed reduction attempts of distal radius fractures in the emergency department. Arch Orthop Trauma Surg. 2018;138(4):591-596. doi:10.1007/s00402-018-2904-2
Ahn L, Vitale M, Franko O. Distal Radius Fractures. OrthoBullets. Published January 9, 2021. https://www.orthobullets.com/trauma/1027/distal-radius-fractures
Johnson D. High-Pressure Injection Injuries. OrthoBullets.
Collesfracture.jpg (1568×1732). Accessed June 25, 2022. https://upload.wikimedia.org/wikipedia/commons/e/e3/Collesfracture.jpg
College O. English: Anatomy & Physiology, Connexions Web Site. Http://Cnx.Org/Content/Col11496/1.6/, Jun 19, 2013.; 2013. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:806_Hand_and_Wrist.jpg
MD JH. English: Anatomical Snuff Box.; 2017. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:Snuffbox2017.jpg
Hellerhoff. English: Joint Dislocation in PIP of D4. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:Finger_luxation_D4_PIP.png
Galindo RJ. English: PA Left Hand x-Ray Showing Fracture at the Neck of Fifth Metacarpal Bone, Commonly Refered to as Boxer’s Fracture. Maracay, Venezuela; Same Patient as File:Boxers Fracture-Lateral Xray.JPG.; 2010. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:Boxers_fracture.JPG
MD JH. English: A Lunate Dislocation.; 2011. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:LunatedislocationL.jpg
Barton’s fracture. Lateral Projectional Radiography of the Right Wrist of a 33 Year Old Man, Showing a Palmar Barton’s Fracture.; 2017. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:Radiograph_of_Barton%27s_fracture.jpg
Hellerhoff. Deutsch: Chauffeur-Fraktur Und Möglicherweise Älterer Abriss Proc. Styloideus Ulnae. Ulnavorschub Mit Zeichen Der Impaktation Am Lunatum.; 2021. Accessed June 25, 2022. https://commons.wikimedia.org/wiki/File:Chauffeur-Fraktur_und_PSU_bei_Ulnavorschub_mit_Impaktation_83W_-_CR_ap_-_001.jpg