Hepatitis Panel Interpretation
/Viral hepatitis is a commonly encountered and increasing problem thanks in part to the rise in injection drug use. Here I review the screening recommendations and interpretation of hepatitis B and C serology. Screening recommendations are based on CDC and US Preventative Task Force guidelines. Prevalence of viral hepatitis is much higher in the ED setting and may warrant expanded screening. This is an active area of research and there are as of yet no formal professional recommendations regarding expanded screening.
Hepatitis B
HBV Screening: Based on country of origin and personal risk factors.
Country of Origin: Screen all individuals from countries w/ high endemic rates (almost everywhere excluding US, Canada, northern Europe, Australia)
Personal Risk Factors: Screen patients with history of IVDU, MSM, HIV/Immunosuppression, elevated transaminase of unknown origin, current pregnancy, maternal infection, and hemodialysis.
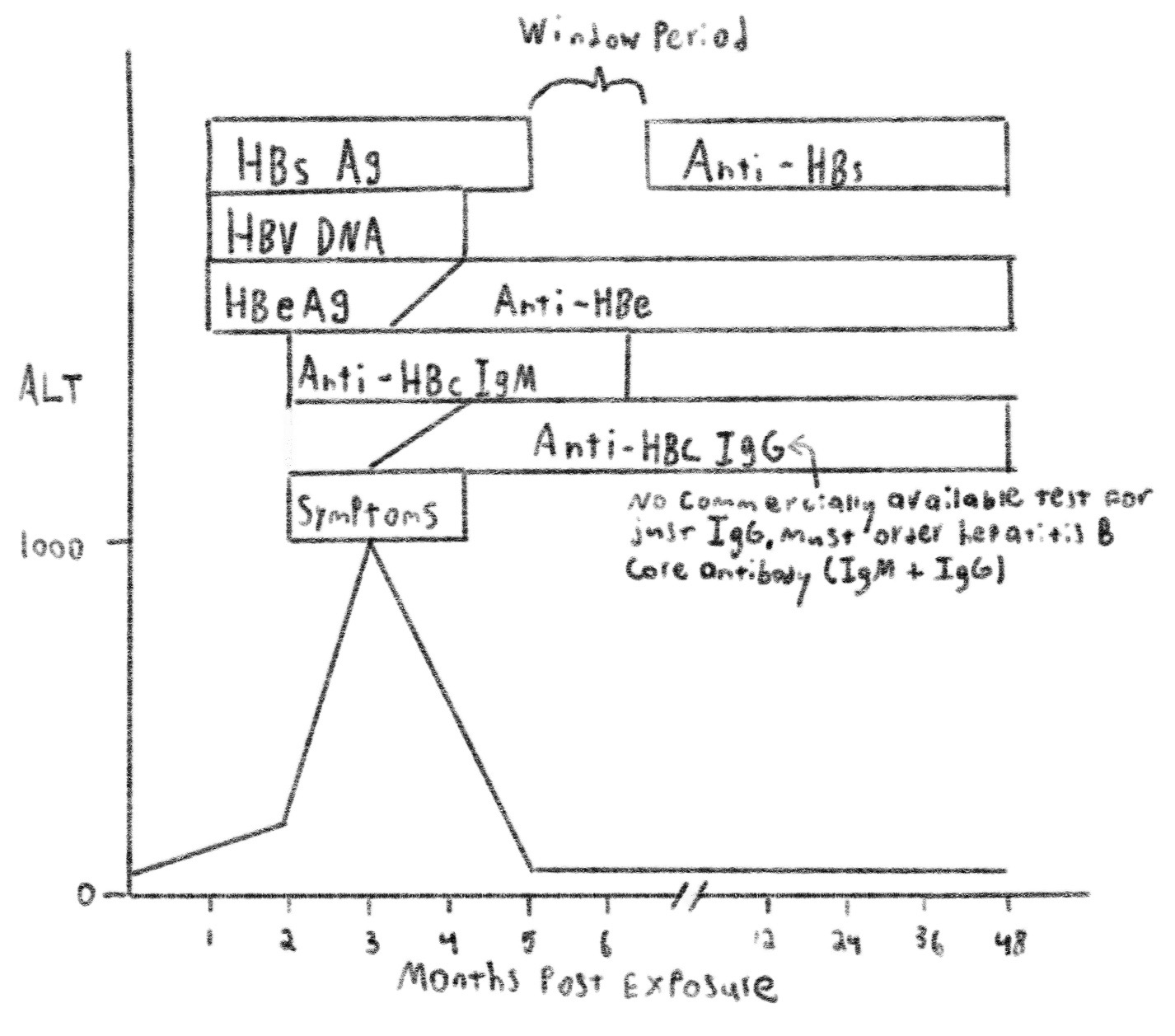
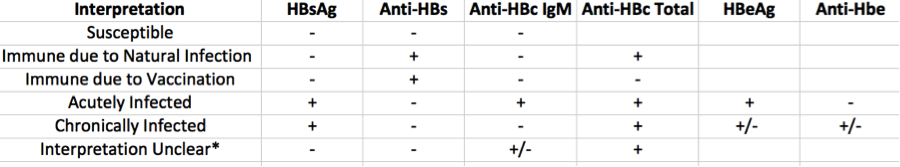
HBV Serologic Interpretation: Interpretation is complex but an understanding of the natural disease course makes interpreting serology much simpler. Below you will find the relevant antigens/antibodies tested for in hepatitis B and the timeframe in which each appears. Note that these timeframes can vary by several months and that the graph below is skewed somewhat towards time of earliest expected appearance.
Acute Hepatitis B Infection
Chronic Hepatitis B Infection
HBsAg: Hepatitis B surface antigen, a protein on the surface of HBV. The presence of HBsAg indicates that the patient is infectious.
Anti-HBs: Hepatitis B surface antibody. The presence of Anti-HBs indicates immunity from HBV.
Anti-HBc: Hepatitis B core antibody. Generated against core antigen, a protein found in infected hepatocytes that is not generally tested for. Anti-HBc IgM is generated early in infection and replaced by Anti-HBc IgG. Presence of IgM indicates recent infection (<6m).
HBeAg: Hepatitis B envelope antigen. Presence of HBeAg is indicative of active viral replication.
Anti-HBe: Hepatitis B envelope antibody. Its presence has prognostic and treatment implications in chronic infection.
*There are 4 possible interpretations. Most commonly this represents distant infection in which Anti-HBs is no longer detectable but Anti-HBc is. Also possible is that testing was obtained during the “window” period in which Anti-HBs is being generated but is bound entirely to HBsAg and is thus undetectable. Another interpretation is that this represents a low level chronic infection in which HBsAg is simply too low to be detectable. Finally, this could be a false positive Anti-HBc. At any rate this serology warrants re-testing at a later date.
Big Picture
The point of testing in the ED is to identify infection. This can be accomplished through HBsAg and anti-HBc IgM alone, and in fact this is what is tested for in the acute hepatitis panel at our institution. By adding Anti-HBs it is possible to determine immune status. However, HBV vaccination is a 3 dose series that is unlikely to be initiated in the ED, and therefore testing for immune status may be of lesser importance in the ED setting. The remaining tests should be ordered if viral infection is present, but need not be included in initial screening tests.
Hepatitis C
HCV Screening: Based on age and personal risk factors.
Age: Screen all adults born between 1945 and 1965 due to high prevalence in this age cohort.
Personal Risk Factors: Screen patients with history of IVDU, HIV/Immunosuppression, elevated transaminase of unknown origin, hemodialysis, STI or multiple sexual partners, clotting factor concentrate administration prior to 1987, organ transplants or transfusion prior to 1992, incarceration, intranasal drug use, maternal infection, and unregulated tattoos.
HCV Serologic Interpretation: This is decidedly less complex than HBV testing. Most laboratories simply test for total Anti-HCV (IgM + IgG). However, some institutions will do separate IgM testing as well. Positive antibody testing warrants further quantitative RNA testing. Positive RNA testing indicates active HCV infection. Negative testing indicates exposure that did not progress to chronic HCV. 15-25% of patients exposed to HCV will not develop chronic infection.
A quantitative RNA test result with high viral load (>800,000 IU/mL) is suggestive of acute infection. However, many patients with acute infection will not have high viral loads, and many patients with chronic HCV exhibit high viral loads (especially those with HIV co-infection). Viral load does have important treatment implications and is worth obtaining in order to assist our ID/GI colleagues.
Written by: David Habib, MD
Peer Review: Jeffery Hill, MD MEd