Grand Rounds Recap 5.24.2017
/Morbidity and Mortality with Dr. Dan Axelson
Case #1
Pt is a young woman with ESRD and HTN who presents with HA + vomiting and photophobia, first visit gets HTN control and sent home then returns <24h later and diagnosed with a spontaneous SDH, likely secondary to uremia and platelet dysfunction.
Learning Point #1: New HTN definitions
- JNC 8: Does not use "hypertensive urgency"
- JNC 7: "Unfortunately the term urgency has led to overly aggressive management of many patients with severe, uncomplicated hypertension"
- ACEP policy: "Asymptomatic markedly elevated blood pressure" 160/100
Learning Point #2: Does headache count as "end organ damage"?
- By itself, no
- Headache + ______ then yes
- nausea/vomiting
- blurry vision
- neuro deficits
Learning Point #3: What clinically qualifies as "end organ damage"?
- Lethargy/confusion/seizures- HTN encephalopathy
- Papilledema/cotton wool spots
- Chest pain/nausaea/diaphoresis relieved nitro
- Aortic dissection
- JVD, rales, S3
Learning Point #4: When do I worry about and how do I treat uremic platelet dysfunction?
- We don't know a specific number
- Treatment recommendations:
- dDAVP @ 0.3mcg/kg IV/SQ or 3mcg/kg IN
- Dialysis
- Cryoprecipitate
Learning Point #5: Why didn't we attribute the SDH to her HTN?
- Location is everything, most HTN bleeds are perforated arteries and happen deep in the white matter
Case #2
Sick asthmatic who gets all the things for asthma thrown at her, ends up intubated and in the ICU. pH of 7.01 CO2 of 95
Learning Point #1: Who gets Mag?
- NNT of 3 in "Severe" asthmatics to prevent admission
- Define severe as Peak Expiratory Flow Rate (PEFR) of <200L/min that did not double after 2-3 albuterol tx
Learning Point #2: What are steroids buying me in asthma?
- NNT 8 for saving hospital admission (5 in severe)
- NNT 10 for preventing relapse
- The later the steroids are given, the less helpful the steroids are at preventing admission
- For every 30 min delay from triage the OR of admission is 1.19
- Prednisone v Dexamethasone
- Prednisone x 5d v Dexamethasone in the ED and 1 dose 24h later
- Return to normal activity better in dexamethasone group
- Hospital admit, ED visit, and PCP visit all the same
- Return to normal activity better in dexamethasone group
- Prednisone x 5d v Dexamethasone in the ED and 1 dose 24h later
- Oral = IV = IM
- Prednisone 40mg = 50mg = 60mg
Learning Point #3: When and how should I give Epi?
- When inhaled medications are rendered useless
- Too much constriction and edema
- Delirium/coma
- Respiratory arrest
- O2 sats are compromised
- How does it work?
- B2 agonism gives bronchodilation
- alpha 1 agonsim yields microvascular constriction, decreasing edema
- Whats the best route?
- Thigh > Arm
- IM > SC
Case #3
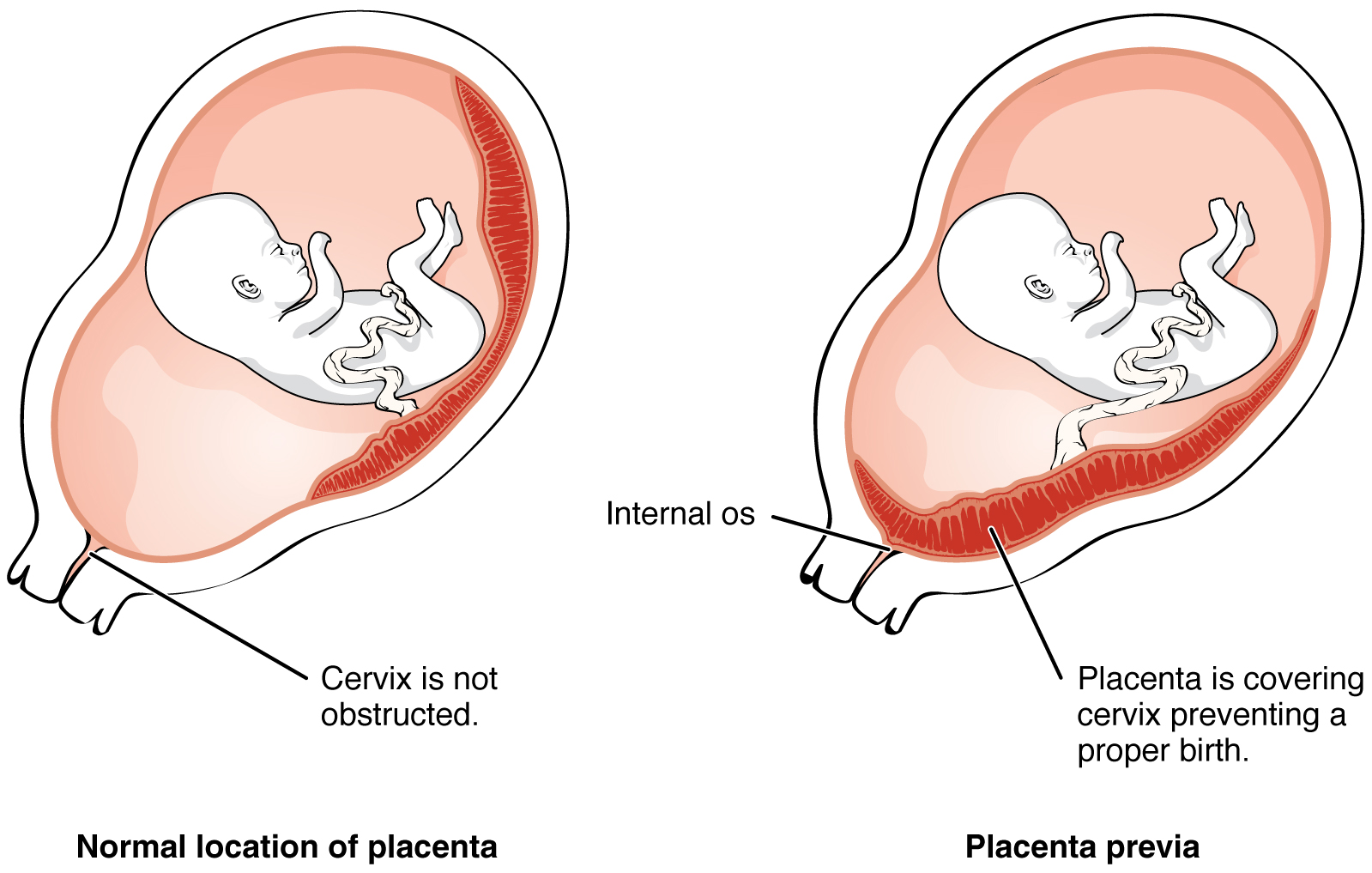
G8 P6 at 16wks by LMP who presents with vaginal bleeding, found to have placenta previa on US.
Learning Point #1: Vaginal bleeding by trimester
- 1st Trimester:
- Ectopic pregnancy
- Abortion
- Threatened
- Inevitable
- Incomplete
- Missed
- Vaginal/Cervical Cause
- 2nd/3rd Trimester:
- Placenta Previa
- 10% of patients <20 wks, most resolve by delivery
- Placental Abruption
- Uterine Rupture
- Vasa Previa
- Vaginal/Cervical
- Placenta Previa
Learning Point #2: Placenta Previa/Increta
Learning Point #3: Digital Exams at 20+ weeks
- Two problems:
- Placenta previa: risk of bleeding
- PPROM: risk of bacterial translocation, risk of precipitating labor
Case #4
11mo with bronchiolitis who was sent home initially, returns on day of illness 3 and ends up on high flow NC and admitted to the PICU.
Learning Point #1: What is the course of bronchiolitis?
- Cough + Coryza + Fever (<39)
- Sx peak day 3-5, cough can last 2-3 wks
- First episode of wheezing <12mo, almost always <24mo
- RSV 50-80%, a neg RSV swab does not rule out bronchiolitis
Learning Point # 2: Who can go home with bronchiolitis?
- Age >2mo
- RR normal for age
- Only mild retractions
- Initial O2 sat >94%
- Adequate oral intake
Learning Point # 2.5: What about Oxygen?
- Routine use of supplemental oxygen is NOT recommended if SpO2 is >90%
- Routine use of continuous pulse oximetry NOT recommended if not on supplemental oxygen (increases admissions and LOS in the hospital)
Learning Point #3: Are there any Prospective, Multicenter Bronchiolitis Studies Predicting ICU admission?
- Age <2months (OR 4.14)
- ED visit in the past week (OR 2.15)
- Severe retractions (OR 2.56)
- Inadequate Oral intake
Learning Point #4: Who needs High Flow NC in bronchiolitis?
- Retrospective analysis of all infants admitted to the PICU and tx with HFNC in Australia
- 2005- 37% intubated (HFNC comes onto the scene)
- 2009- 7% intubated
- Retrospective chart review of kids admitted to the PICU before and after HFNC in New Jersey
- NNT 7
- CCHMC attending recommendations:
- Clinical or laboratory respiratory distress/failure
- Apnea/mental status
- PICU
- Hypoxia despite standard oxygen therapy
- Warmed, humidified O2 so higher flows very well delivered
- It does likely give some variable degree of PEEP
- Start 1-2L/Kg/Min
Case #5 - Case Series on UTI treatment in the ED
Learning Point #1: What actually is a "complicated" UTI?
- UTI associated with an underlying condition that increases risk of failing therapy
- Uncontrolled DM
- Pregnancy
- AKI/CKD
- Indwelling catheter/stent/nephrostomy tube
- Functional/anatomical abnormalities of the urinary tract
- Renal transplant
- Male Gender
Learning Point #2: Are all male UTIs complicated by definition?
- In treatment, yes
- Treat for 7 days
- Avoid macrobid and B lactam (poor prostate penetration)
- In work-up, no
- Not all men under 50yo need work up for the cause of their UTI
Learning Point #3: What are formal tx recommendations for cystitis?
- IDSA
- Nitrofurantion 100mg BID x 5 days
- Bactrim 160/800mg BID x 3 days
- Fosfomycin 3gm oral single dose
- Fluoroquinolones (high resistance)
- B-lactam 4th, lower efficacy
- UCEM
- Keflex 500mg BID x 3-7 days (E coli 96%)
- Omnicef 300mg BID x 3-7 days (E coli 98%)
- Macrobid 100 BID x 5 days (E coli 91%)
- Fluoroquinolones x 3-5 days (E coli 87%)
- Bactrim x 3 days (E coli 85%)
Learning Point #4: What are the formal tx recommendations for pyelonephritis?
- IDSA
- Ciprofloxacin 500mg BID x 7d
- Levofloxacin 750mg qD x 7d
- Bactrim 160/100mg BID x14d
- UCEM
- Cephalosporins (Keflex, Omnicef) x 10-14d
- Bactrim 160/100mg BID x 14d
Learning Point #5: What are formal tx recommendations for treatment of complicated cystitis?
- Treatment should be guided by recent antimicrobial use and recent culutre data.
- Cystitis: at least 7 days
- Pyelonephritis (including pregnancy) 10-14d
Learning Point #6: One dose IV antibiotics and d/c on oral antibiotics for pyelonephritis?
- Non-inferiority study showed no difference in outcomes v admission to the hospital for IV antibiotics
Case #6
Young male who presents initially with a rash consistent with VZV, comes back with acute cerebellar ataxia.
Learning Point #1: Acute Cerebellar Ataxia (ACA) is a thing
- Thought to be mostly an autoimmune phenomenon with most of this happening post-viral
- Most common in <3yo (>50% of acute ataxia in children)
- Diagnosis is made clinically in this age group
- ~20% of varicella infections result in ACA
- Also consider EBV, cocksackie, HSV, parvo B19, others
- 1/10 of ACA patients have residual symptoms
Learning Point #2: Can I trust orthostatic VS for volume assessment
- Looked at patients without evidence of blood loss or hypovolemia on presentation, many were orthostatic based on vitals
- 40% Sn and 70% Sp for volume depletion
Learning Point #3: How does Romberg test work again?
- Romberg- described in 1836 in tabes dorsalis patients who had trouble walking in the dark
- Cerebellum process:
- Vision
- Proprioception
- Vestibular sense
- Romberg test is a of the posterior column, not a cerebellar test
- Midline cerebellar signs
- Truncal ataxia
- Wide based gait
- Nystagmus
- Dysmetria on heel-to-shin
- Lateral cerebellar signs
- Ipsilateral UE weakness
Case Follow-up: Jazz for Airway Masters with Dr. Charlie Kircher
“All the technique doesn’t matter...only if the feeling is right.” - John Coltrane
EMS Call: Elderly F with “some kind of airway infection” with difficulty breathing.
VS 110, BP 160/90, 85% NRB, RR 40
Exam: Agonal respirations and respiratory failure, morbidly obese, tachypneic with poor inspiratory effort in the bases bilaterally
Bag valve mask during preparation to bring up oxygen saturations. Using the glidescope on the first attempt showed a great view of the cords but unable to pass even a 6.0 tube through. Second attempt with a bougie with the 6.0 tube with some additional force was successful. Post-intubation CXR shows a tracheal stent which was the likely source of the obstruction to intubation.
Further chart review: tracheal histoplasmosis s/p serial tracheal stents. Granulation tissue had developed near the top of the stent causing significant narrowing.
Can you perform a cricothyroidotomy through a stent? Probably but it's likely to be more difficult and there may be complications.
Tracheal/Airway Stents: Indications
- Malignant tracheobronchial obstruction
- Subglottic stenosis
- Benign tracheal or bronchial stenosis
- Localized severe expiratory central airway collapse
- Anastomotic structure or dehiscence following lung transplant
Recommendations for airway management of patients with tracheobronchial stents
- Trach/Cric - high risk of complications
- LMA is safest option
- If tracheal intubation necessary - awake fiber optic technique
- Emergency - awake fiberoptic with bougie for ETT
Pediatric Head Trauma with Dr. Aaron Murphy-Crews
Anatomical Differences in Pediatric Patients
- Larger surface area more prone to bleeding
- Cranium is thinner and more predisposed to fracture
- Higher center of gravity and poorer balance leads to increased frequency of head trauma
Epidemiology
- 600,000 ED visits annual
- 60,000 admissions
- 7,400 deaths
- < 2 yo, NAT is the leading cause of death from head trauma
- About 50% of these patients get a head CT
Characterizing Trauma
- Severity based on GCS:
- Mild 14-15
- Moderate 9-13
- Severe < 9
- Clinically Important TBI is the presence of intracranial injury (SDH, EDH, cerebral contusion) AND at least one of the following:
- Neurosurgical intervention
- Intubation
- Hospitalization
- Death
For NON-minor trauma: (GCS < 13 about 20% have clinically important TBI)
- Get a head CT
- Avoid hypoxia
- Elevate HOB
- Avoid fever
- Hypertonic saline
Minor head trauma: About 50% get CT Head but there is a very low incidence of clinically important TBI
What's so bad about that CT scan of the head?
- Estimated 1 new brain cancer and 1 new leukemia per 10,000 head CT at modern dosing
- Other estimates range from 1:1000-5000 scans to cause one cancer
PECARN
Particularly useful because it was designed to tell us who we don't need to scan.
Separates < 2 and 2 and older children.
Large, prospective and validated.
Excellent sensitivity for predicting clinically important TBI and helpful to avoid unnecessary radiation.
How does it compare to similar studies: CHALICE and CATCH?
Sensitivity of CATCH and CHALICE were much lower than PECARN for detecting clinically important TBI.
What about vomiting?
If vomiting is the ONLY sign after head injury, clinically important TBI is unlikely.
Alternatives to Head CT
- Point of care ultrasound can be used to look for skull fracture
- However, 50% of injuries have no associated skull fracture
Visual Diagnosis with Dr. Hoehn
HSP
- Immunoglobulin A vascuilitis
- Most common vasculitis in children
- Ages 3-15, peak 4-6
- 1/2 cases proceeded by URI
- Diagnosis
- Purpura or petechiae (usualy palpable)
- LE predominant
- w/o thrombocytopenia or coagulopathy
- Arthritis or arthralgia
- Abdominal Pain
- Intussusception
- Renal involvement
- UA
- HTN
- Purpura or petechiae (usualy palpable)
Kawasaki's
- One of the most common vasculitides in children
- Etiology-> ?
- Typically self-limited but certain complications (CA aneurysm, depressed myocardial contractility, HF) lead to significant morbidity/mortality
- 80-90% of cases in kids <5
- Diagnosis
- Fever x5 days without other explanation and 4/5 of the following:
- Bilateral bulbar conjunctival injection
- Oral mucous membrane changes
- Peripheral extremity changes
- Polymorphous rash
- Cervical LAD
- Fever x5 days without other explanation and 4/5 of the following:
Measles
Highly contagious
Fever, malaise, cough, coryza, conjunctivitis followed by a rash
- Several day prodrome: fever, malaise, anorexia, conjunctivitis, coryza, cough
- Klopik spots --> pathognomonic
- Exanthem 2-4 days after fever
- Starts on face and spreads cephalocaudally
Rocky Mountain Spotted Fever
- Tick-borne disease
- Rickettsia rickettsia
- Most cases spring/summer
- Highest incidence <10 years of age & 40-64yo
- Risk factors exposure to dogs, residing near wooded areas
- Mortality --> 3%
- Incubation period--> symptoms present 2-14 days after being bitten by infected tick
- Clinical manifestations
- Early --> nonspecific symptoms
- Rash
- 90% of patients
- blanching erythematous with macules that become petechial
- Starts on ankles and wrists and spreads to the trunk
- Palms and soles