Grand Rounds Recap 3.29.2017
/Morbidity and Mortality Conference with Dr. Riley Grosso
Case 1: Calcium Channel Blocker and Beta Blocker Overdose
Check out this Tox Short from OHSU about bradycardia!
Physiology of Ca-Channel Blocker Overdose
L-type calcium channels allow calcium influx into myocardium and smooth muscle cells activating the sarcoplasmic reticulum to release more calcium to allow for muscle contraction. This also controls automaticity in the SA node.
Endocrine effect of Calcium Channel Antagonists (CCAs)
- In the shock state: the myocardium preferentially uses glucose for fuel
- The liver responds with gluconeogensesis to increase circulating glucose
- Calcium-channel blockers also block insulin release from the pancreas
- All of this results in hyperglycemia and a diabetic-like state in the tissues
Physiology of Beta Blocker Overdose
When activated, the beta-1 receptor increases cAMP in the cell which then phosphorylates the L-type calcium channel allowing for calcium influx into the cell through the channel. In overdose, it thusly behaves similarly to Ca-channel overdose.
Treatment of Ca-Channel Blocker or Beta-blocker Overdose
GI decontamination (gastric lavage/activated charcoal)
- Not routinely recommended.
- If the patient presents within the first one to two hours after overdose and is asymptomatic it may be useful.
- If the patient is symptomatic it's not likely to be helpful and more likely to harm given concern for aspiration/airway compromise.
Calcium:
- Mechanism: increasing extracellular calcium may overcome competitive antagonism of calcium and force Ca through unblocked channels. Indicated for both Ca-channel and Beta blocker overdose.
- Dose: Aim for a 2-3 fold increase in serum Ca
- Bolus over 5-10 min of 0.6mL/kg of 10% CaGluc (0.2 mL/kg of 10% CaCl)
- Followed by gtt @ 0.6-1.5 mL ml/kg/hr of 10% Calu (4-10 gm/hr)
Glucagon
- Mechanism: increases circulating glucose (for this reason it is less likely to be effective on Ca-channel blocker overdose); direct myocardial action via stimulation of myocardium via cAMP (similar to catecholamines) through a separate receptor
- Dose:
- 50-150 mcg/kg (3-10 mg in 70kg patient)
- Peak response in 5-7 min, lasts for 10 min
- Can repeat in 3-5 min
- If responsive consider gtt at the effective bolus dose
- No maximum - if you haven't had a response by 12 mg, you may be unlikely to get one
- Nausea and vomiting are common and are dose related
- 50-150 mcg/kg (3-10 mg in 70kg patient)
Insulin
- Level 1D recommendation (if myocardial depression is present)
- Mechanism: inotropic properties possibly due to its role in carbohydrate metabolism and myocardial utilization of glucose "metabolic rescue"
- In Beta-blocker overdose: the patient will also need glucose.
- In Ca-channel overdose: remember to check the glucose regularly - the patient will eventually become euglycemic.
- + Inotropic effects, no chronotropic effects
- Dose:
- 1U/kg regular insulin bolus followed by gtt at 0.5-1 U/kg/hr
- Blood pressure and contractility increase within 15-60 min
- Potassium shifts, pay attention to the need for supplementation (generally patients are not total body potassium deplete but will have shifts)
- 1U/kg regular insulin bolus followed by gtt at 0.5-1 U/kg/hr
Catecholamines:
- Mechanism: adrenergic receptor antagonists
- Norepinephrine - first line to treat blood pressure to improve vascular tone
- Epinephrine - to increase cardiac output and heart rate
- Dobutamine - recommended if cardiogenic shock is prominent for + inotropic effects with the caveat that vascular tone is likely to decrease
- Larger doses than normal may be needed
Intralipid:
- Mechanism: "Lipid sink"
- Dose 1.5 ml/kg bolus followed by a drip of 0.25ml/kg/min for 30-60min
Methylene Blue
- Mechanism: inhibits NO-cGMP pathway which decreases vasodilation and increases responsiveness to vasopressors
- Evidence is not great, but anecdotal evidence and case reviews suggests that it may be helpful.
Other treatments to consider:
- ECMO
- Balloon pump
- Pacemaker
Case 2: Resuscitation in Trauma
What are the indications for massive transfusion?
Statistically significant correlation with need for massive transfusion:
- INR greater than 1.5
- SBP less than 90 mmHg
- Hemoglobin less than 11 g/dL
- Base deficit greater than or equal to 6
- dFAST (+)
- HR greater than or equal to 120
Strongest likelihood of requiring massive transfusion in 24 hours:
- INR > 1.5 (OR 3.4)
Post-intubation Hypotension (PIH)
Why we care about this:
The frequency and significance of postintubation hypotension during emergency airway management.
- Patients with PIH had significantly higher in-hospital mortality (33% vs 21%)
- Among survivors, PIH correlated with increased mean ICU and hospital LOS
Which patients are at risk of PIH?
- Pre-intubation shock index > 0.8, odds ratio 55 of developing PIH, even if normotensive
- Shock index = HR/SBP
Take away points: if your shock index is > 0.8 or the patient is hypotensive, consider resuscitating before you intubate. Or, if intubation can't wait, have push-dose pressors ready.
Case 3: Neurologic Catastrophes that Cause Cardiac Arrest
A minority of out-of-hospital cardiac arrests are preceded by neurologic injury 4-10%.
When to suspect a neurologic cause of OHCA?
- Initial rhythm is not VF
- Complaints of headache prior to arrest
In 244 OHCA patients - all received a head CT whether ROSC was obtained or not: 6% had SAH but 15% of those that had ROSC had aSAH.
ECG Findings of ICH in OHCA
- ST segment elevation can be seen in as many as 78% of patients, especially in aVR and V1
- ST segment elevation in two contiguous leads is exceedingly rare
- ST segment depression is nearly universal and T wave inversions are common
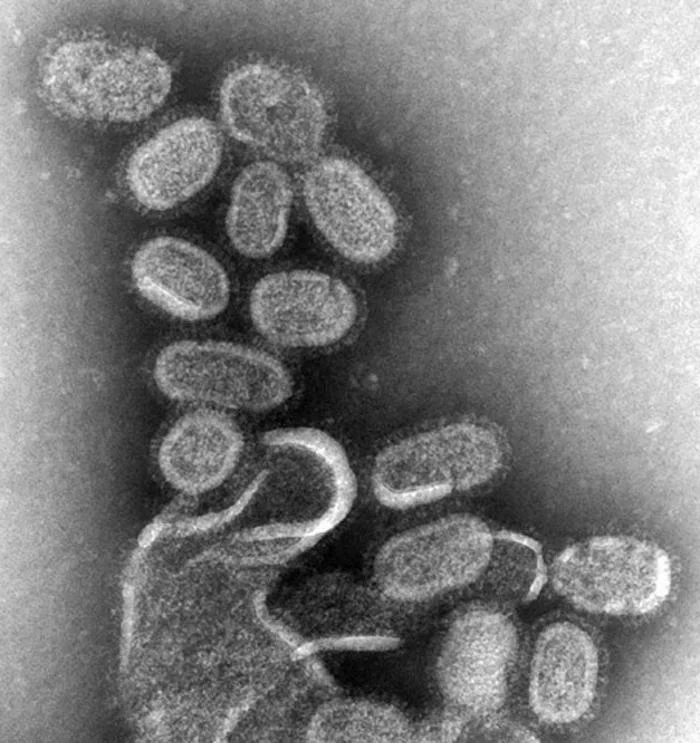
Case 4: Influenza
- Flu is peaking about a month later than it did last year.
- Three different types
- Influenza A
- Categorized by H&N glycoproteins: H1N1 and H3N2 are the current human strains
- Most prevalent, more severe morbidity
- Frequently causes seasonal outbreaks and epidemics (this is the only one that can cause pandemics)
- Influenza B
- Less prevalent
- Less often the cause of seasonal outbreaks
- Influenza C
- Least prevalent
- Causes only sporadic cases or minor outbreaks
- Can cause severe respiratory infections in children under the age of 6
- Influenza A
- Humans can develop relative immunity to influenza B and C (but typically not A) after having the infection as a child which may be why these infections are less severe than influenza A.
- Infectious patterns
- Transfer of respiratory secretions
- Incubation period: 18-72 hrs depending on inoculum dose
- Viral shedding:
- Begins 24 hrs prior to start of symptoms
- Peaks 1-2 days after start of symptoms
- Continues to shed up to 10-14 days
- Clinical Presentation:
- Respiratory symptoms +/- fevers, chills, headache, body aches
- Usually sudden in onset - patients can often tell you specifically when their symptoms began
- Pediatrics: GI symptoms predominate and fevers higher than adults
CDC recommends testing only when it will impact treatment.
Diagnosis:
- Rapid antigen detection (RAD): 40-80% sensitive
- How good is clinician gestalt? Probably similar to the rapid test or clinical decision rules.
- If clinical suspicion is high but the RAD is negative and the answer will change management: consider getting a PCR or treating empirically.
What about neuraminidase inhibitors? Do they help?
Cochrane Review: Neuraminidase Inhibitors
- Time to first symptom alleviation:
- Adults: symptom relief 16.8 hr faster
- Children: no effect in asthmatic children (but treatment is recommended), symptom relief 29 hr faster in other children
- Hospitalizations: no significant effect
- Serious complications: no significant effect
- Pneumonia: NNT 100 to prevent "self-reported" pneumonia (but not clinically or radiographically confirmed pneumonia)
- Harms of treatment: nausea and vomiting (NNH 28 and 22 respectively)
- Preventing transmission:
- NNT 33 to reduce risk of symptomatic influenza in one person
- NNT 7 to reduce risk of symptomatic influenza in one person in the same household as the confirmed case
CDC recommends treatment for patients:
- at high risk for complications (see link above for details)
- who are hospitalized
- with laboratory-confirmed or highly suspected influenza who have severe symptoms
Case 5: Beware Abdominal Pain in the Elderly
15% of ED visits in patients over 65 yo are for abdominal pain (3rd most common behind chest pain and shortness of breath)
- Admission rates up to 60%
- 20% of admitted patients will have an invasive procedure while admitted
- 17% mortality of those undergoing a procedure
More difficult in the elderly:
- 20-30% have a blunted fever response
- Worse immune function
- Altered mental status
- Poor access to care
R3 Taming the SRU with Dr. O'Brien
The Case: Elderly male with history of NASH cirrhosis and DM II, presenting for HA and neck pain upon awakening, facial numbness and droop and subdural hematoma on CT. INR 2.6.
He arrives as a transfer from an OSH with worsened neurologic deficit: flaccid paralysis of LUE and 3/5 strength in LLE. Taken for repeat head CT with a large R parenchymal with concern for active bleed.
Coagulation Changes in Liver Disease
- Because the liver is responsible for both pro and anti-hemostatic factors a relative balance remains in liver failure
- INR is a marker of disease severity
- TEG
- Allows for guided factor replacement
- Successful use in liver transplant patients
- May predict bleeding risk more accurately than INR
DIC
- Consider in sepsis, severe trauma
- Treat the underlying cause
- Monitor platelets, fibrinogen
Febrile Seizures with Dr. Andrew GOlden
Diagnostic criteria:
- Seizure
- Simple: Lasts < 15 minutes, generalized, only once in 24 hours
- Complex: Lasts > 15 minutes, focal component, or more than one in 24 hours
- 6 - 60 months of age
- Temp > 38 C
- Absence of CNS infection or metabolic imbalance
- Absence of history of prior afebrile seizures
Risk factors:
- Height of fever
- Viral illness
- Genetic susceptibility (of patients presenting to the ED for febrile seizures, 10-20% will have a first degree relative with a history of febrile seizures)
- Atopy
- Recent immunization
AAP Recommendations for Simple Febrile Seizures:
- routine blood testing is not recommended
- any patient with seizure and fever with signs or symptoms concerning for meningitis should get an LP
- for patients between 6-12 months of age who are deficient in H. flu or S. pneumo vaccinations - consider LP
- for patients pretreated with antibiotics who have seizure + fever - consider LP as antibiotics may mask meningitis symptoms
- EEG not routinely recommended
- Neuro imaging is not routinely recommended
Acute treatment:
- Benzodiazepines
- lorazepam 0.05-0.1 mg/kg IV
- diazepam 0.1-0.2 mg/kg IV
- midazolam 0.2 mg/kg buccal or IM, max 10 mg
- Disposition: home with education
How to counsel parents:
- Recurrence
- < 12 months of age: about 50%
- > 12 months of age: about 70% will have no recurrence
- Likelihood of epilepsy
- General population 0.5%
- Simple febrile seizures 1.1%
- Multiple simple febrile seizures, age < 12 months, family history: 2.4%
- Complex febrile seizures: 9.2%
- Anticonvulsants: not recommended due to significant risk from side effects
- Antipyretics: treat fever but don't reduce recurrence
Complex Febrile Seizures
- Increased risk of having complex febrile seizure:
- Younger age at first seizure
- Developmental delay
- Treatment:
- ABCs
- Benzos
- Second line therapies are your typical AEDs: fosphenytoin, depakote, keppra
- Work-up:
- Blood work
- Indications for neuro imaging:
- large head circumference
- persistently abnormal exam
- signs on exam of increased ICP
- EEG if prolonged seizure or concern for status
Febrile Status Epilepticus
- 25% of all Status Epilepticus in children
- Continuous seizure activity for 30 minutes or longer ***
- 78% of patients required more than 1 AED
- 48% required respiratory support and 85% of those required intubation
CPQE: Ventilator Management In obstructive lung disease with Dr. Gerad Colmer and Dr. Courtney McKee
Mortality Data
- Asthma: ~40,000 deaths/year nationwide
- Admission < 1%
- Intubated: 7-10%
- COPD: ~147,000 deaths/year
- Admission: 2.5%
- If intubated: 22-38%
Pathophysiology
- Asthma
- Larger proximal airway structures have increased resistance to flow due to decreased diameter (mucus, inflammation, mucosal edema)
- Generally healthy alveoli and distal airways
- COPD
- Destruction of distal lung tissue and alveoli
- Collapse of small airways trapping air in alveoli
Non-Invasive Positive Pressure Ventilation (NIPPV)
- Contraindicated for patients who can't tolerate the mask or can't remove the mask if needed.
- Cochrane Review 2012 of NIPPV in Asthma
- Increased number of patients appropriate for discharge
- Improved tachypnea and work of breathing
- No mortality benefit shown
- COPD
- Predicting failure of NIPPV
- GCS < 13 at the time of arrival
- After 1 hour of bipap: ABG pH < 7.35 and/or RR > 20
- Sensitivity of RR > 20 in predicting failure 85%
- Other studies showed similar pattern: poor mental status, severe acidosis on arrival or persistent acidosis after 1-2 hours of NIPPV, tachypnea
Mechanical Ventilation of Patients with Asthma
Vent mode: no great studies - use what you are comfortable with or start with assist control - volume.
Risk factors for morbidity in mechanically ventilated patients with acute severe asthma.
- Major complications: barotrauma from dynamic hyperinflation and hypotension
- Air trapping from incomplete exhalation causes intrathoracic pressure to rise (high end-inspiratory pressure)
- Increased intrathoracic pressure decreases preload resulting in hypotension
- Air trapping can cause direct damage to alveoli due to over distention
Key components of initial vent settings in acute asthma exacerbation:
- Recommended breath rate: 8-10 bpm (to allow for adequate exhalation)
- Tidal volume: 6-8 mL/kg recommended
- PEEP recommendation: 5 cmH2O (or 75% of the patient's plateau pressure as measured at end of an inspiration)
Mechanical Ventilation in COPD Patients
Initial vent mode: no great studies - use what you are comfortable with or start with assist control - volume.
Again the goal is to ventilate while minimizing barotrauma and air trapping or dynamic hyperinflation.
Initial Vent Settings:
Tidal Volume: 6-8 mL/kg of ideal body weight
Rate: 10-12 breaths per minute
PEEP: 5 cm H2O (or 75% of what you measure to be the patient's intrinsic PEEP during an end expiratory hold)
Troubleshooting
- Dislodgment of the tube: reconfirm placement
- Obstruction of the tube: suction
- Pneumothorax: bedside ultrasound, decompress the chest, CXR
- Equipment: check your vent
- Stacked breaths: disconnect the circuit and allow total exhalation
If the patient is still hypoxic:
- Increase FiO2 with a goal saturation of 90-94%
- Consider placing an arterial line for serial ABG assessments
- Increase PEEP (to a point) by slow increments
If the patient is still tachypneic - and breath stacking:
- Ensure appropriate sedation to improve synchrony with the vent
- Consider chemical paralysis if patient is refractory to increased sedation or increased sedation is contraindicated
If the patient is air trapping:
- The patient doesn't have enough time to exhale
- Decrease respiratory rate
- Increased exhalation time
If the patient is acidotic:
- Increase your ventilation (but beware of air trapping) - RR then TV
- Be sure to check plateau pressure with increases (ideally less than < 30 cm H2O)
- Consider arterial line again to check serial blood gases
- Some permissive hypercapnea may be allowed if lung mechanics will not permit adequate ventilation: to pH of 7.2
If the patient has elevated plateau pressure:
- Decrease tidal volume (lower limit is 4-5 cc/kg of ideal body weight)
- Consider transitioning to pressure control mode
If the patient is hypotensive:
- Volume status?
- Sedation meds?
- Pneumothorax?
- Air trapping with increased intrathoracic pressure? (disconnect from the vent, allow to exhale, and bag)
CPC with Dr. Liebman vs Dr. Powell
The Case: Young, adult male presents with chest pain, it is substernal, 10/10 and has been present for three weeks. Subjective fevers. Worse with deep inspiration and movement, radiates to the throat, back and shoulder pain. Also with right sided pain along his ribs. No history of trauma. Self-medicating with IV heroin and is also taking methadone. Last use of heroin was 2-3 days ago.
PMH: Scheuermann's disease, OCD, schizophrenia, bipolar disorder
PSH: multiple orthopedic surgeries for various fractures
Social Hx: IVDU, tobacco, occasional EtOH
Meds: methadone, gabapentin, propranolol
Vitals: normal, afebrile
Physical exam: slightly uncomfortable
- HEENT: normal
- Neck: track marks, no lymphadenopathy
- Chest: normal with exception of pain with palpation of the sternum
- Pulm: normal
- Abd: normal
- Neuro: normal
- MSK/Skin: track marks and ulcerations on extremities
EKG: Sinus rhythm, no ST segment changes
CBC - WBC 12.0, normal diff and otherwise normal/Renal - normal
Troponin negative x 2
A diagnostic test was ordered...
Dr. Powell works through the case:
Summarizing the case:
- Young male with a history of IVDU and chest pain
- Possibly some fullness in the anterior mediastinum on CXR per Dr. Powell's read
- Leukocytosis (mild 12.0)
- Elevated bicarb and tachypneic on arrival
- Possible evidence of right heart strain on EKG
- Painless nodules with necrotic centers on both legs
Is this IVDU related or non-IVDU related?
Building the differential using the VINDICATE Me pneumonic.
What fits from the long list?
- Infectious/Inflammatory
- Neoplastic
- Drugs/Deficiency
- Idiopathic/Iatrogenic/Intoxication
Dr. Powell's test of choice: CT Chest with IV Contrast
Dr. Powell's diagnosis: Osteomyelitis or Septic Joint
The actual diagnostic test: CT Chest with IV Contrast!
The actual diagnosis: Sternal osteomyelitis with costochondritis of the adjacent first rib
Osteomyelitis
- Mechanism of infection: hematogenous spread, contiguous spread +/- vascular insufficiency, or direct inoculation (trauma, iatrogenic)
- Acute (days to weeks) or Chronic (months to years - refractory to antibiotics)
- Most common cause of osteo in all comers is S. aureus
Sternal Osteomyelitis
- Primary: no adjacent focus of infection
- 0.3% of all cases of osteo in the literature, most cases are described in IVDU
- Caused by hematogenous spread of organism (usually S. aureus or P. aeruginosa)
- Most patients benefit from antibiotics
- Few patients become septic
- Mortality low: approaching 0% in the age of antibiotics
- Presentation is subtle: insidious onset of sternal pain, some may have skin findings (erythema, tenderness, indurated mass)
- Early detection is important
- labs may show: leukocytosis, ESR elevations
- radiology studies negative in the early stages
- soft tissue swelling is first sign
- cortical irregularity occurs later
- Beware septic arthritis of the sternoclavicular joint
- Secondary: complication of median sternotomy or trauma
- Complication of CABG: 1-2 %
- Risk factors: length of time on bypass, excessive post-op hemorrhage particularly with re-exploration, use of internal mammary bypass graft, CPR
- Typically S. aureus, K. pneumonia, C. albicans
Clinical Course: Admitted to medicine. TTE negative for endocarditis. ID consult recommended bone biopsy prior to antibiotics. Blood cultures grew out GPC in clusters. Taken to the operating room and found to have severe osteomyelitis of the first rib and manubrium sternum and first rib. Discharged to SNF on antibiotic therapy.
How long should these patients be on antibiotics?
- Typically at least 6 weeks from most recent debridement
- Trending ESR/CRP can be helpful
- New studies suggesting that oral antibiotics may be effective in chronic osteomyelitis