Necrotizing Fasciitis and the Spectrum of Soft Tissue Infections
/Soft tissue infections are common, and every emergency doctor will see many, many, many cases of cellulitis and superficial abscesses. The trick is to recognize and respond to the rare but life-threatening necrotizing soft tissue infections, in particular necrotizing fasciitis.
Table 1: Classification of Necrotizing Fasciitis (1)
Necrotizing fasciitis is a rapidly progressive bacterial infection that tracks along the fascia and is associated with severe sepsis and a deadly prognosis. The diagnosis is rare compared to cellulitis and abscesses, though it may initially present very similarly, making recognition a challenge. Several types of necrotizing fasciitis exist, and differ by microbiology and typical affected population (See Table 1.)
The clinical picture of necrotizing fasciitis is variable and dependent on time course. The classic presentation is a patient with an erythematous skin lesion (72%) with edema (75%) and pain outside of the erythematous margin, as well as pain out of proportion 72% to their examination. (1,2)
Late findings at the site of infection include hemorrhagic bullae, crepitus, superficial necrosis, violaceous or ecchymotic discoloration, and “wood hard” lesions (Figure 1). Anesthesia of the affected area may result from infarction of superficial nerves. It should be noted that visible signs of this infection may be late appearing, as it is deeper structures that are initially involved. Systemic findings of necrotizing fasciitis include fever, hypotension, and altered mental status, due to sepsis. (3,4) Air on radiologic imaging is diagnostic, if seen. (4)
Figure 1 - Skin Findings of Advanced Necrotizing Fasciitis. (By Piotr Smuszkiewicz, Iwona Trojanowska and Hanna Tomczak [CC BY 2.0 (https://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons)
Necrotizing fasciitis requires an entirely more aggressive approach than the more familiar soft tissue infections to avoid morbidity and mortality. Timely surgical consultation is the key to reducing mortality, which is between 20% and 30%. (5) Gold-standard diagnosis happens in the OR by fascial visualization, and is followed by extensive debridement. Initiation of broad-spectrum antibiotics (vancomycin + piperacillin/tazobactam + clindamycin is standard) is also indicated, and cardiovascular support is often necessary for these very sick patients. (2)
So, necrotizing fasciitis is deadly, rare, and easy to confuse with something more benign. Is there a clinical decision tool that might help us identify necrotizing fasciitis? Read on for the underwhelming answer.
The LRINEC Score
Table 2 - LRINEC Scoring System (6)
The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) is a scoring system described by Wong et al. in Critical Care Medicinein 2004. (6) The study describing the score was a retrospective observational study (read “chart review”) that looked at 89 admitted patients diagnosed with necrotizing fasciitis and 225 patients admitted with severe cellulitis or abscess over 5.5 years at a teaching hospital in Singapore.
The researchers utilized logistic regression to identify laboratory values that predicted whether a patient was likely to have necrotizing fasciitis rather than one of the other diagnoses. Laboratory values that were found to be independent predictors of necrotizing fasciitis were then assigned integer values based on their regression coefficients to create a scoring system with a max score of 13 and a cutoff of ≥6 (Table 2). Testing of this decision rule by the authors in a validation cohort showed a negative predictive value of 96.0% and a positive predictive value of 92%.
So does this mean that you can send some labs on that weird cellulitis and feel good sending them home with cefazolin and TMP-SMX if they don’t score ≥6 on the LRINEC?
Not really.
Critique
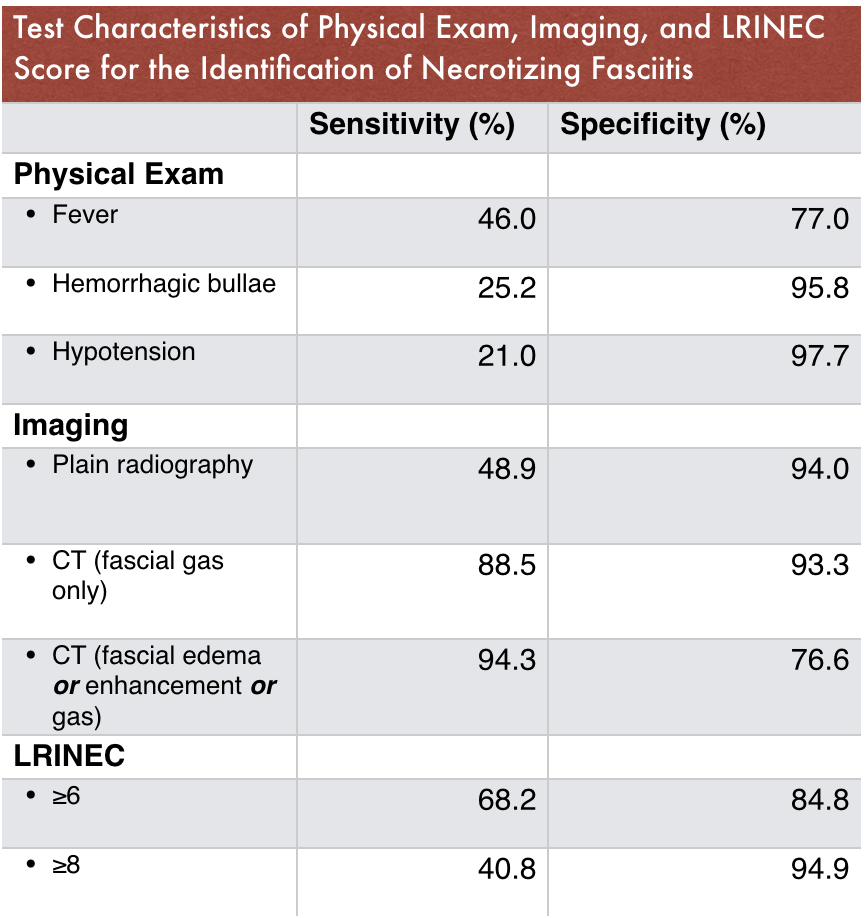
Table 3 - Test Characteristics of the LRINEC Score (10)
To start, the score has not really held up well when applied to new populations. Subsequent studies have found the sensitivity to be 80% or below for the suggested cutoff score. (7,8) In addition, a case of necrotizing fasciitis with a LRINEC score of 0 in the ED has been described. (9)
A decision rule for a deadly disease should have exceptional sensitivity. A recent meta-analysis looking at the test characteristics of physical exam findings, imaging tests, and the LRINEC score demonstrates poor sensitivity of the scoring system. Certain physical exam characteristics and CT scan performed better than LRINEC, but no single test or finding was sufficient for ruling out the diagnosis (Table 3).
So, why might it be that the LRINEC score has not proven to be a robust and reliable indicator of necrotizing fasciitis?
First, it is important to recognize what the components of LRINEC are really indicating – systemic derangement. These laboratory criteria are signatures of critical illness and severe sepsis. Early cases of necrotizing fasciitis may not yet demonstrate significant laboratory abnormalities, as patients’ disease has not yet progressed to that stage.
Looking back to the cohort in the original paper, the studied patients were admitted and the first blood tests on admission were used for the analysis. This tells us as ED providers that this isn’t our patient population, and it isn’t the timeframe of disease during which we will necessarily see it. We are likely to see earlier manifestations of necrotizing fasciitis, and certainly hope to catch the diagnosis then.
Also, this score was designed to help separate necrotizing fasciitis from severe abscess and cellulitis (all patients fell into one of these two groups), but it wasn’t designed to help differentiate between necrotizing fasciitis and other things that might be on your differential. The ED, home of the undifferentiated patient, may not be the place to apply a decision rule separating just two diagnoses. So what else is on the differential (Table 4)?
Table 4 - Differential Diagnosis for Extremity Pain/Swelling/Erythema
Bottom line
The LRINEC score is not recommended to bear much weight in the decision making surrounding suspected necrotizing fasciitis. As the LRINEC authors themselves state, “it should be emphasized that the diagnosis of necrotizing soft tissue infections is a clinical diagnosis, and this diagnosis or even suspicion of it warrants immediate operative debridement.” Good advice.
Mentioning that someone’s LRINEC score is 10 is not a bad way to let your surgery friend know that you are highly concerned and it’s time to trot to the ED, but a LRINEC score of 2 won’t prevent the same urgent consult in someone with dodgy blood pressure, an excruciatingly painful leg with violaceous coloring, and a history of diabetes. Clinical suspicion is the cornerstone of this diagnosis.
So, if your patient with a soft tissue infection has any of…
- Pain out of proportion to their examination
- Pain or edema outside of the area of erythema
- Systemic illness (tachypnea, hypotension, tachycardia, altered mentation)
- Bullous, necrotic, or ecchymotic lesions
- A rapidly progressing course (3,4)
…then it’s likely time to consider advanced imaging and surgical consultation to move the patient toward life-saving treatment.
References
- Kelly EW, Magilner D. Necrotizing Soft Tissue Infections. In: Tintinalli JE, Stapcyznski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine, 8th edn. New York: McGraw-Hill, 2016: 1034–6.
- Stevens DL, Baddour LM. Necrotizing soft tissue infections. UpToDate.com. 2018. https://www.uptodate.com/contents/necrotizing-soft-tissue-infections?search=necrotizing fasciitis&source=search_result&selectedTitle=1~117&usage_type=default&display_rank=1 (accessed Aug 26, 2018).
- Stevens DL, Bisno AL, Chambers HF, et al.Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America. Clin Infect Dis2014; 59: e10–52.
- Pallin DJ. Necrotizing Skin and Soft Tissue Infections. In: Walls RM, Hockberger RS, Gausche-Hill M, et al., eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 9th edn. Philadephia, USA: Elsevier, 2018: 1718–9.
- McHenry CR, Piotrowski JJ, Petrinic D, Malangoni MA. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg1995; 221: 558–65.
- Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med2004; 32: 1535–41.
- Burner E, Henderson S, Burke G, Nakashioya J, Hoffman J. Inadequate Sensitivity of Laboratory Risk Indicator to Rule Out Necrotizing Fasciitis in the Emergency Department. West J Emerg Med2016; 17: 333–6.
- Holland MJ. Application of the Laboratory Risk Indicator in Necrotising Fasciitis (LRINEC) score to patients in a tropical tertiary referral centre. Anaesth Intensive Care2009; 37: 588–92.
- Wilson MP, Schneir AB. A case of necrotizing fasciitis with a LRINEC score of zero: Clinical suspicion should trump scoring systems. J Emerg Med2013; 44: 928–31.
- Fernando SM, Tran A, Cheng W, et al.Necrotizing Soft Tissue Infection: Diagnostic Accuracy of Physical Examination, Imaging, and LRINEC Score: A Systematic Review and Meta-Analysis. Ann Surg2018; XX: 1.
Authorship
Written by - Brandon Berger, MD
Editing and Posting - Jeffery Hill, MD MEd

![Figure 1 - Skin Findings of Advanced Necrotizing Fasciitis. (By Piotr Smuszkiewicz, Iwona Trojanowska and Hanna Tomczak [CC BY 2.0 (https://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons)](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1535807945056-JUTABA1RK4YTHDZN6BF6/Necrotizing_fasciitis_left_leg.JPEG)