Grand Rounds Recap 10.5.2016
/R4 Simulation with Drs. Derks, McKean, and Mudd
The Case: "Drunk and disorderly" female patient in her 30s brought in by EMS for clearance before going to jail. She was found wandering in the street by police. The patient refuses to allow providers to take a history or vital signs
- Physical Exam: Agitated, difficult to redirect. Multiple skin lesions/sores but nothing infected appearing. She is diaphoretic. Otherwise unrevealing
- Vitals: HR 133, BP 121/60, Sat 98% on RA, RR 23, Febrile
- PMH: EMR reveals history of thyroid disease and possible bipolar disorder
- Labs: CBC - normal, Renal - normal, TSH: 0.03, Free T4: 5.54, CSF: tube 1 - 9 WBCs, 51% lymphs, gram stain negative
Differential Diagnosis: Thyroid storm, substance abuse, alcohol withdrawal, NMS, meningitis, bacteremia, sepsis
Diagnosis - Thyrotoxicosis
- Most cases are caused by Graves disease, usually presenting between age 20-40
- Above age 40 consider toxic multi nodular goiter
- Treatment:
- Beta-blockers: propranolol (classic answer, esmolol can be used as well)
- Inhibition of new thyroid hormone synthesis
- PTU - oral/rectal, blocks release and conversion of thyroid hormones (safer in pregnancy)
- methimazole - oral/rectal
- Blocking thyroid hormone release (should occur 1-2 hours after PTU or methimazole)
- Lugol solution
- Potassium iodide
- Ipodate
- Lithium carbonate
Oral Boards
Case 1: Elderly male at rehab after recent stroke coming in with respiratory distress. He is on prednisone chronically but hasn't been getting it at the nursing home. Exam reveals course breath sounds, wheezing, and mild tachypnea. Vitals: febrile, tachycardic, tachypneic, hypotensive 72/46. CXR shows bilateral infiltrates.
Diagnosis: HCAP with sepsis, adrenal insufficiency
Critical Actions: obtain CXR, diagnose PNA, administer steroids, give antibiotics, give fluids before giving pressors, disposition to appropriate level of care (step-down, ICU)
Case 2: 19 y/o M with SOB, syncope and fatigue from home. Reportedly 'passed out' today with intermittent palpitations and fatigue x1 week coalescing in syncope today for several minutes w/o post-ictal phase. Vitals: borderline tachycardia, otherwise unremarkable. EKG: Bradycardia with complete heart block. While in ED patient becomes symptomatic again with bradycardia and hypotension. Skin exam shows ring-like lesion around what appears to be insect bite. Neuro exam is unremarkable.
Diagnosis: Complete heart block 2/2 suspected Lyme disease.
Critical Actions: obtain EKG, begin transcutaneous pacing, administer pain meds/sedation for pacing, full skin exam to identify etiology of heart block, begin Lyme treatment with IV ceftriaxone or penicillin G, discuss with cardiology and admit to CCU/EP Lab.
Case 3A: 50 yo M with snake bite to foot. Patient's friend states that it looked like a Copperhead. Vitals: tachycardia, otherwise unremarkable. Exam: Tachycardia, left foot 1 + pitting edema with two puncture wounds, 2+ pulses.
Treatment: Antivenin is recommended for upper extremity wounds to reduce disability, laboratory abnormalities, rapidly worsening swelling or wounds can also benefit. Stable mild swelling can be observed. Be sure to check tetanus status. Antibiotics are not indicated empirically but watch for secondary infection. Watch for compartment syndrome.
Case 3B: 35 yo F with bilateral hand pain and anxiety. + Tobacco use. Vitals: HR 101, otherwise normal. Exam: Distal fingers are pale and cool bilaterally with no capillary refill.
Diagnosis: Raynaud's Phenomenon
Treatment: Place hands in warm water
Case 3C: 45 yo M with rash. Rash is pruritic, started on legs, and spread up to trunk. Recently went on vacation and spent a lot of time in a hot tub, no other outdoor exposures. Exam: Hypertensive, afebrile, otherwise normal vitals. Rash is noted from well demarcated line on his mid chest down throughout his lower extremities.
Diagnosis: "Hot tube" folliculitis which is usually caused by pseudomonas.
Treatment: otherwise healthy patients can be treated with a fluoroquinolone, consider bactrim/keflex if there appears to be a secondary infection like abscess or cellulitis
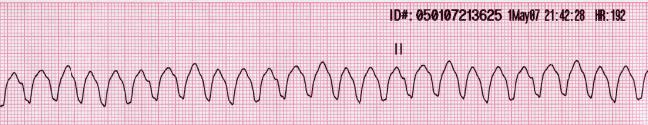
Vtach Case Follow UP: Master's Class with Dr. Jeff HILl
Setting the scene: Dr. Hill is an R3 and gets a telemetry call about a hypotensive, tachycardic patient is lethargic but awake with pre-hospital 12 lead EKG showing Vtach. EMS attempts cardioversion but is unsuccessful. The patient arrives, still in ventricular tachycardia.
Treatment strategies for refractory ventricular fibrillation or ventricular tachycardia
Dual Defibrillation:
- Retrospective chart review of double sequential external defibrillation including 12 patients
- 3 of the 12 got ROSC and survived to hospital discharge
- Ultimately there's not good data, but it may be worth trying
Ischemia leads to dysrhythmia:
- Can patients undergo cardiac catheterization while undergoing CPR using a mechanical device? Retrospective review of 43 patients showed that it is possible to have successful PCI while undergoing CPR
- What about thrombolytics?
- Small case series showed successful ROSC after VT/VF arrest with good neurologic outcome with use of tPA in 3 patients
What about beta blockers?
- Retrospective pre-post study of esmolol to treat patients with refractory Vfib
- Small study including 25 patients, 6 received esmolol (500 mcg/kg bolus followed by a drip)
- How would beta blockade be helpful?
- Epinephrine can increase coronary perfusion pressure but also increases myocardial oxygen demand
- Beta blockade may reduce myocardial oxygen demand (primarily a beta effect)
- Animal studies have showed decrease number of shocks and decreased ischemia using beta blockers with epi
- Survival to hospital discharge and survival with good neurologic outcome were improved with the use of esmolol
Outcome for this patient:
- Dual defibrillation several times
- Multiple rounds of CPR
- Ultimately sustained ROSC was never achieved
troponinemia Case Follow up with Dr. Collins harrison
The Case: 54 yo F presents with multiple complaints: lightheadedness, fatigue, dry cough, headache, paresthesias and decreased grip strength in bilateral upper extremities, abdominal pain, left shoulder pain, right calf pain, heel pain. Troponin obtained with triage labs was elevated at 14. Vitals are normal. Exam: well-appearing, normal cardiac/lung exam, benign abdomen, past-pointing with bilateral upper extremities. Labs show: equivocal UA with RBCs and WBCs, elevated CK, elevated troponin which is trending upwards. Initial and repeat EKGs are normal.
Differential Diagnosis of an Elevated Troponin
- Ischemic
- ACS: STEMI vs NSTEMI (plaque rupture)
- Non-ACS
- Coronary
- Non-coronary: hypoxia, global ischemia, hypo perfusion, recent CT surger
- Non-ischemic
- Myocarditis (infection, cardiotoxic, systemic/AI, hypersensitivity) - 50% progress to dilated cardiomyopathy!
- Pericarditis
- Takotsubo cardiomyopathy
- Etiology: stress (physiologic or emotional) catecholamine toxicity, coronary spasm, microvascular dysfunction
- Diagnosis: LV dysfunction - focal apical ballooning on echo, no CAD + new EKG changes or elevated troponin
- Stroke
Case, continued:
- CT head obtained shows multiple infarcts in multiple territories suggestive of embolic source, also seen on MRI
- Cardiology also consulted but deferred management after the CT scan results returned
- Left heart catheterization was eventually obtained and was normal as was a trans thoracic echo without evidence of vegetation.
- LE duplex shows DVT and CTPA shows multiple PEs
- TEE obtained shows a mitral valve vegetation raising concern for culture negative endocarditis, she is treated empirically
- Finally, CT abdomen and pelvis is obtained which demonstrated primary ovarian and uterine malignancies
- Mitral valve vegetations were determined to be likely secondary to severe hyper coagulable state in the setting of advanced malignancy, no infectious source was identified
Clinical soapbox with Dr. brent boyer
The Heroin Epidemic
History:
- Cecily Saunders RN, MD - Founder of palliative medicine; first to pioneer morphine for suffering at St. Christopher's Hospice.
- Jan Stjernsward, MD and Vittoria Ventafridda, MD - WHO Pain Ladder created for the treatment of palliation and pain management in patients with cancer including the use of opiates for moderate to severe pain
- 1980s Changing thoughts: If you screen patients for substance abuse first, you can use opiates safely for non-cancer pain
- Letter to the Editor in the NEJM in 1980 by Dr. Hershel Jick: "Addiction rare in patients treated with narcotics."
- 1990s Changing actions: American Pain Society states pain is a "vital sign" and must be treated appropriately
- 2001: Joint Commission implements pain standards for healthcare organizations
- Press-Gainey joins in and includes pain management in post-visit surveys
- State legislatures institute intractable pain laws stating that patient's have a right to adequate pain control, including narcotics
- Oxycontin is approved in 1995, touted as less addictive due to time release formulation. Purdue pharmaceutical did not have hard data to back up claims that it was less addictive. It wasn't clear to doctors and the FDA at the time that crushing or dissolving the tablet could lead to a direct high
- Reimbursement schemes for pain clinics shifted away from multi-modal pain control to narcotic use
Ohio's Story:
- Portsmouth, Ohio: Industrial town that suffered an economic decline in the 1980s when Detroit Steel left the area
- Dr. David Procter arrived to Portsmouth and opened the "South Shore Clinic," a family medicine clinic that transitioned to a pain clinic. Charged $120/patient for a visit for narcotic prescriptions. Considered the "Godfather of Pill Mills." He hired and trained a number of physicians that went on to start their own clinics throughout Ohio
- Dr. Procter was ultimately convicted of manslaughter after several of his patients overdosed. Many of the doctors he trained were indicted
- Pill mill reform occurred, multiple licenses were revoked, pill-crush resistant formulations are created, and ultimately it gets harder to get prescription opiates
What happens when you cannot get prescriptions opiates? Enter heroin.
- Black tar heroin from South America enters circulation
- Many addicts transitioned from prescription narcotics to heroin.
Recommended Reading: Dreamland by Sam Quinones
What now?
- AMA drops pain as a vital sign
- Pill mill doctors
- Consider prescribing narcan to these patients
lithium toxicity Cpc: Dr. Murphy vs Dr. Lafollette
The Case: Elderly patient with schizophrenia, bipolar, dementia, HTN, HLD, DM who presents for AMS. Vitals are normal. Exam shows agitated patient screaming incoherently. Non-focal neurologic examination with the exception of dilated but symmetric pupils and occasional uncontrolled limb jerking movements. Labs, UA, CXR are unremarkable and unrevealing. Negative CT Head
Test of choice:
Lithium level 2.3
Lithium Toxicity
Lithium is remarkably similar to sodium from an atomic standpoint, therefore the body treats them almost interchangeably.
- Rapidly absorbed
- Narrow therapeutic index
- Slow equilibration into the CSF
- Almost exclusive renal excretion
Acute Toxicity
- High serum concentrations
- Mild or absent neurologic symptoms in the acute phase (lithium takes time to the cross the blood-brain barrier)
- GI symptoms are prominent; nausea/vomiting/diarrhea
- May see EKG changes
- The most accurate lithium level should be obtained 6 hours post-ingestion (early levels in asymptomatic patients may be artificially high due to the way the drug distributes).
Acute on Chronic Toxicity
Chronic Toxicity
- Usually due to changes either in absorption or elimination
- Higher dose of the medication
- Decrease in GFR
- Meds: NSAIDs, diuretics, ACE-inhibitors
- Dehydration
- Renal injury
- Neurologic symptoms are the hallmark: agitation, delirium, seizures, coma
- Diabetes Insipidus
- Hyperthyroidism
SILENT: Syndrome of Irreversible Lithium Effectuated NeuroToxicity
- "Neurologic dysfunction, especially cerebellar symptoms, persisting for at least 2 months without further lithium exposure."
- Symptoms lasting longer than 6 months are likely permanent
- This is a clinical diagnosis
Management:
- GI decontamination is not recommended
- Supportive care: rehydration and renal support to increase elimination, dialysis if symptomatic or high serum level - in conjunction with a toxicologist near you
Clinical Diagnostics with Dr. Josh Gauger
Overview:
- CRP is produced during the inflammatory cascade
- ESR is the rate at which red blood cells settle in a test tube. This takes longer if there is more fibrinogen, IgG etc within the blood. This can occur as a result of many types of inflammation.
- Pro-calcitonin: this is unregulated in bacterial infections and down regulated in viral infections
Case 1: Native Vertebral Osteomyelitis
- IDSA Guidelines: Obtain bacterial cultures, baseline ESR/CRP, spine MRI
- 40% will have a normal WBC, 55% afebrile
- ESR and CRP elevation 94-100% sensitive, trend can guide treatment
- MRI 97% sensitive and 93% specific (but only after three weeks of infection)
Case 2: Septic Arthritis
- ESR/CRP 94-98% sensitive but they are not specific
- Joint aspirate and clinical exam should guide therapy
- ESR and CRP should be used more to adjust your pretest probability, not used post-test
Case 3: Cellulitis
- LRINEC: scoring system for necrotizing soft tissue infection using CRP
- Criticism of LRINEC:
- Not an ED-only population
- CRP cutoff binary
- Retrospective observational study
- Recent studies call sensitivity into question
Case 4: Febrile 7 week old
- Procalcitonin is probably the most accurate test for serious bacterial infection and invasive bacterial infection in young children (above elevated WBC count, ESR, and CRP).