Grand Rounds Recap 6.28.2017
/Mortality and Morbidity with Dr. Betham
Case #1: Male in his 60s with chest pain, significant family history of CAD, normal vitals. EKG: RBBB, initial trop negative. Repeat EKG shows a posterior STEMI, pt taken to the cath lab.
RBBB
- Diagnostic Criteria
- Wide QRS > 120ms
- RSR' in V1-V3 ("rabbit ears")
- Wide, slurred S wave in lateral leads I, aVL, V5-V6
- In BBB, the T wave is opposite the direction of the QRS slurring
Posterior MI (check out Annals of B-pod March 2016 EKG Corner)
- Accounts for 15-20% of STEMI
- Usually with lateral or inferior infarct as well
- 3-11% isolated posterior
- Frequently missed due to positioning of the EKG
- Consider getting a posterior EKG with V7-9
- Often L circumflex disease
- Can be RCA if right dominant
Case #2: Male in his 60s with history of coronary disease with stent placement 1 year ago who presents with chest pain. EKG: ST depression V3-V6, I & aVL, and ST elevation in aVR. Cath lab activated and ends up with lesion in circumflex.
aVR
- Mirror of the lateral leads
- Reflects changes in the R upper portion of the heart
- Useful in its own right
- PR elevation in pericarditis
- R' in TCA overdose
- ST elevation in AV nodal re-entrant tachycardia
- How is ST elevation in aVR used in MI
- Reciprocal change from ST depression in the lateral leads
- Often indicates severe disease
- Prognosticate in the hospital
- ST elevation in aVR associated with older age, increased number of risk factors,
- OR if in-hospital mortality with aVR elevation
- Minor OR 4
- Major OR 6
- A single culprit lesion is often not found
- Isolated ST elevation in aVR is not a STEMI
- Recommend emergent consultation of the interventional cardiology
- Treat as NSTEMI
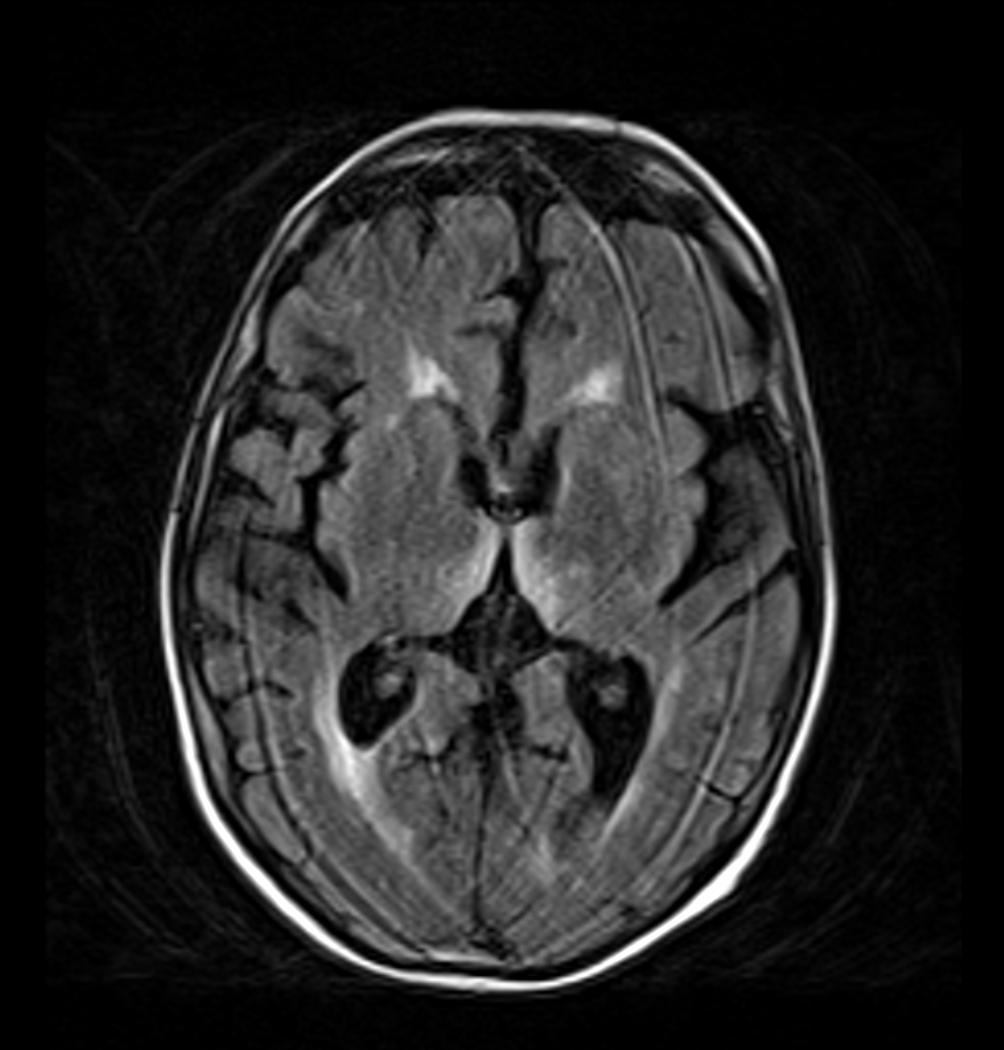
Case #3: Female in her 30s who presents with weakness and inability to perform ADLs who fasted earlier for religious reasons. LE>UE weakness, vertical & horizontal nystagmus, doesn't follow commands, sleepy, temporal wasting. MRI shows abnormal signal in mammillary bodies, thiamine deficiency, diagnosis of Wernicke's Encephalopathy
Wernicke's Encephalopathy
- Results from critical vitamin B1 deficiency
- Alcoholism
- Bariatric surgery
- 4-12 weeks post-op
- Hyperemesis
- Chronic illnesses
- Anorexia
- Fasting/unbalanced diet
- Staple diet of polished rice
- Develops in 2-3 weeks
- Prevalence in the US 0-2.2%
- Estimated mortality 17%
- Men > Women
- Triad of symptoms
- Ophthalmoparesis
- Nystagmus
- Horizontal & vertical
- Evoked by gaze
- Lateral rectus weakness
- Loss of conjugate gaze
- Nystagmus
- Ataxia
- Altered Mental status
- apathy and confusion
- progresses to coma and death in weeks if untreated
- Ophthalmoparesis
- Diagnosis
- MRI shows abnormal enhancement
- Vitamin B1 levels
- Treatment
- Admit
- Vitamin B1 IV then home on PO
Case #4: Young man with inability to use his bilateral upper extremities, septic, multisystem organ failure, + rhabdomyolysis with compartment syndrome of his BUE. Lost use of bilateral hands.
Compartment syndrome
- Increased pressure within a muscular compartment resulting in compromised perfusion, tissue necrosis
- Causes
- External compression
- Hemorrhage into a compartment
- Reperfusion injury
- Five "P"s
- Most sensitive: pain with passive flexion/extension
- Other early findings: parasthesias and loss of 2-point discrimination
- Paralysis is a late finding
- Frequently irreversible (~13% recover function)
- Pallor/Pulselessness? Unlikely
- Clinical exam pitfalls:
- Depressed GCS
- Simultaneous nerve injury
- Sensitivity of palpation of the compartment is about 50%
- Whats an abnormal pressure? (Check out our video on how to use an a-line set-up to check compartment pressures)
- Normal is less than 10 mmHg
- Greater than 30mmHg is generally diagnostic
- Delta pressure= DBP - compartment pressure
- 20-30mmHg or less is diagnostic
- Sometimes felt to be better than absolute pressure in decision-making for fasciotomy
Case #5: Male in his 40s with DM who presents with penile swelling, septic shock, EKG with STEMI, sent to cath lab with clean coronaries. EF 20-25% thought to be secondary to his sepsis. EF recovers before discharge.
Cardiomyopathy in Sepsis
- Global LV hypokinesis in ~60% of septic shock patients
- Increasingly recognized as Takotsubo phenomenon
- ST segment elevation common
- Normal LHC
- Recovers at 10-14 days with appropriate treatment
- Likely multifactorial
- Catecholamines (endogenous and exogenous)
- Inflammatory cytokines
- ?perfusion mismatch in the myocardium
Case #6: Young woman with rectal prolapse and incarcerated, prolapsed, internal hemorrhoids which required operative intervention.
Hemorrhoids
- Incidence unreported: 4-40%
- Most common cause of rectal bleeding
- Vascular cushions that become enlarged and displaced distally
- Pregnancy
- Portal HTN
- Constipation or straining
- Internal or External
- Internal Hemorrhoids
- First Degree: No prolapse
- Warm baths
- 2nd Degree: Spontaneous prolapse and reduction
- Manual reduction with TID warm baths and after every bowel movement
- 3rd degree: digital reduction
- 4th degree: unable to reduce
- First Degree: No prolapse
- Consult surgery
- Severe bleeding
- Severe pain
- Incarcerated or strangulated internal hemorrhoids
- Topical Agents
- Preparation H
- 1.5% topical lidocaine
- 0.3% topical nifedipine
- Excision of the clot?
- Thrombosis >48h, then likely unhelpful
Updates in Global Health with Dr. Deborah Gerdes MD, MSc, DTH&H
Malaria
- 3.2 billion people are at risk of infection globally
- Since 2000 great progress in reducing mortality related to infection- 66% in WHO Africa region and 60% worldwide
- In 2015 still 438,000 malaria deaths -- 90% in Africa
- Majority of deaths are in children under 5
- High burden of disease in Africa
- High prevelance
- Caused by infection with parasites of the genus Plasmodium
- P falciparum (most deadly and common)
- Parasite & Life Cycle
- Clinical course varies with different host factors- age, prior exposure/immunity, pregnancy
- Severe disease is most common in children and travelers
- Milder symptoms: fevers, malaise, headaches
- Severe Malaria: cerebral malaria, severe anemia, acidosis, hypoglycemia, AKI, ARDS, bleeding, and shock
- Cerebral malaria and severe anemia are more common in African children
- Organ failure more common in adults without prior exposure
- Accurate and rapid diagnosis is essential
- WHO recommends rapid diagnostic testing (RDT) for anyone suspected of malaria before beginning treatment
- From 2005 to 2014 use of RDTs increased in WHO Africa from 36% to 6%%
- Some limitations-- including underlying parasitemia in highly malaria-endemic areas
- Thick and thin blood films are also still available and the test of choice in the US
- WHO Principles: early diagnosis, effective treatment, treat only confirmed cases
- Treatment:
- 3 days of artemisinin combination therapy (ACT) for P falciparum
- ACT use increased from 11 million to 2005 to 337 million in 2014
- Severe disease: IV artesunate in Africa; quinine + ?artesunate in US
- First true concerns about ACT resistance noted in Thailand in 2003- along Cambodian border
- Studies in Cambodia during the same time period found reduction in parasitological response
- In 2007, parasite clearance times were found to be significanly longer in Palin than in Wang Pha and decrease in ART susceptibility from Bangladesh through Thailand
- WHO and international community working together to contain resistance
- Increasing resistance to partner drugs-- leading to full treatment failur
- Other areas of focus
- Vector control
- Vaccines
- Malaria Examination
Traveler's Diarrhea
- Most common illness to travelers to lower income
- Represents 1/3 of returning travelers
- Risk highest in 1 k week of travel then declines
Strongyloidiasis hyperinfection
- Strongyloides stercoralis- nematode (roundworm)
- Widespread in tropics and subtropics also reported in more temperate climates
- Larva currens (creeping eruption)
- Caused by migrating larvae during autoinfection
- Hyperinfection
- Complication of the chronic form of the disease
- when host immune system is abruptly reduced-- steroids, DKA, malignancy-- leukemia/lymphoma, immunosuppressive tx
- Steroid use is most common
- Likely under recognized
- Symptoms:
- Severe bloody diarrhea
- Bowel inflammation with microperforations
- Peritonitis
- GN sepsis
- Pulmonary infiltrates, hemopytsis, pleural effusion
- Severe bloody diarrhea
- Diagnosis:
- Stool microscopy
- Duodenal biopsy
- microscopy of duodenal juice
- Serologic tests-- ELISA
- Stool culture
- Hairy string test.
- Much easier to diagnose in hyperinfection
Taming the SRU with Dr. Titone
The Case: Older male found down outside on a hot August day, temp was 105.9 and tachycardic, actively seizing on arrival. Final Diagnosis: Heat Stroke
Fever v Hyperthermia
- Fever
- Elevation in temp that occurs with an increase in the hypothalamic set point
- Vasoconstriction commences
- Body is hot and it likes it
- Hyperthermia
- Something external is heating the body
- Compensatory mechanisms overwhelmed
- Body is hot and can't fix it
Regulatory Mechanisms in Hyperthermia
- Evaporation
- Radiation
- Conduction
- Convection
Hyperthermia Spectrum
- Heat Edema
- Mild Swelling
- Cutaneous vasodilation
- Increased ADH
- Heat Syncope
- Volume depletion and low vasomotor tone
- Decreased venous return
- Postural hypotension
- Heat Cramps
- Salt depletion
- spasm of voluntary muscles
- fasciculations
- salt tabs
- Heat Exhaustion
- Regulation and CNS function is intact
- <105 F
- Can be hypo or hypernatremia, or eunatremic
- Heat Stroke
- Loss of consciousness
- Cardiovascular collapse
- Severe dehydration --> vasoconstriction to maintain mAP--> cessation of heat loss
- Classic:
- Older patient who is out in a heat wave
- mild lactatic acidosis, mild CK elevation, normoglycemia
- Exertional
- Younger patient who is running a marathon
- High lactic acidosis
- Classic:
- "End Stage" Heat Stroke
- Above 107.6F
- Enzymes become non-functional
- Above 107.6F
Resuscitation of Heat Stroke
- Check a glucose
- Think about taking airway early
- Rectal vs bladder continuous monitor
- Ativan (primarily renally cleared) works for shivering and seizures
- Pressor of choice is dobutamine
- Avoid vasoconstriction because the patients are trying to get rid of heat
- Fluids: Classic be judicious, Exertional types should get a lot of fluid
- Cooling Techniques
- Ice packing
- Least effective
- .05 F per min
- Convection Air Cooling
- .07F per min
- Radiation
- 32F surroundings --> .07F per min
- 0F surroundings --> 1F per min
- Evaporative Cooling
- .09F-.015F per min
- Ice Water Immersion
- Most efficient
- Logistically difficult
- .27F-.63F per min
- Ice packing
A quick line of respect for our chief residents Drs Dan Axelson (@axelsontweets), Brittany Betham (@BethamMD), Riley Grosso (@grossoriley), and Jon McKean for a phenomenal year summarizing, addending and connecting our Grand Rounds via these Recaps and engaging our online community - thank you immensely and good luck next year!