STEMIs in Disguise
/The 2013 ACC/AHA STEMI guidelines outline, with specific age and gender-related cutoffs for ST segment elevation in certain leads. While these are clinically important, there are several STEMI equivalents or EKG patterns that do not meet these criteria but should point the practitioner to consult with an interventional cardiologist. These STEMI equivalents are found in 10-25% of cases of coronary occlusion, making it imperative that emergency personnel be familiar with these patterns. The equivalents included on the 2013 ACC/AHA guidelines include:
Wellens
De Winter Waves
LMCA occlusion
Hyperacute T waves
Posterior MI
For the purposes of this post, we will focus on LMCA Occlusion, Posterior MI, Wellens, and De Winters Waves. For additional reading, follow some of the links throughout the post and take at look a previous TamingtheSRU post done by Robert Whitford, MD
LMCA occlusion taken from Life in the Fast Lane. Note that ST elevation in aVR>V1, with widespread ST depression. https://litfl.com/lmca-occlusion-st-elevation-in-avr/
ST elevation in aVR with diffuse ST depression
What Could this Represent?
Left main coronary artery critical stenosis
A recent study investigating the incidence of this ST elevation with diffuse ST depression found that complete occlusion occurred in only 10% of patients (Harshas 2019). This makes sense given that complete occlusion would cause quick cardiogenic shock. Instead, main culprit behind the ECG findings was sub-occlusive disease (multivessel in this particular study) along with other medical causes (PE, sepsis, dissection).
Left proximal LAD disease
Triple vessel disease
Subendocardial ischemia (taken in setting of something like severe tachycardia or sepsis)
aVR is reflective of the basal septum. This means that aVR is either a reciprocal change to the global perfusion, or it represents direct ischemia to the basal septum
Patterns to Look For
ST elevation in aVR: the degree of elevation varies with amount of myocardium involved and is an independent predictor of mortality.
>0.5mM: 81% sensitivity and 80% specificity for determining LMCA occlusions (Yamaji, 2001).
>1.0 mM: may be more specific to LMCA. For a more detailed discussion, see this Rebel EM Post for some more in-depth discussion
aVR > V1: can differentiate an LMCA from an LAD lesion (Rostoff, 2005)
Diffuse ST depression
Typically see in the lateral and precordial leads
No consensus on exact degree of deviation or which leads ST depression needs to be present. One study found that the mean number of leads with ST depression to be about 7 (Harhash, 2019).
Proximal LAD occlusion from Life in the Fast Lane. Note that the elevation in aVR and V1 are of similar magnitude. https://litfl.com/lmca-occlusion-st-elevation-in-avr/
Is this really a STEMI equivalent?
Yes. While a cutoff of about 0.5mm is thought to be a bit nonspecific, there is a fair amount of data suggesting that aVR elevation, particularly as it gets bigger, has some predictive role in determining significant coronary disease. In fact, mortality is directly correlated with the degree of elevation.
ST Elevation in aVR tends to occur more often and greater magnitude in LMCA lesions than in LAD occlusions.
In anterior STEMI patients, an elevation of aVR had a 43% sensitivity and 95% specificity for proximal LAD occlusion
What Should the Management Be?
Emergent vs urgent PCI? Probably neither, because you may be looking at a CABG. aVR elevation with ST depression is still located on the STEMI equivalent guidelines and while these may not necessarily indicate a full blown occlusion, there’s probably a good chance of significant sub-occlusive disease being present. Complete occlusion versus stenosis is not well defined in many of studies about this EKG pattern. That being said, there is still a fairly strong body of evidence that suggests a high sensitivity for elevations in aVR for significant occlusion (defined as at least 75% occlusion in the left main and at least 90%in proximal , with some studies showing sensitivities as high as 80% and specificity as high as 98% (Kosuge, 2011). Most of these patients, whether LMCA or triple vessel disease, will require CABG, so consider discussing dual anti-platelet therapy with your interventionalist prior to administration.
De Winter T waves
This is from an anterior STEMI with classic de Winter T waves from Life in the Fast Lane https://litfl.com/de-winter-t-wave-ecg-library/
De Winter T waves are found in only about 2% of proximal LAD lesions (Verouden, 2009). But when present, they have a PPV of 95.2-100% of signficant stenosis of LAD, 70% stenosis or greater (Morris, 2017). Patient’s with these EKG findings typically present with substantial, acute chest pain and tend to be younger with a history of dyslipidemia (Verouden, 2009)
Patterns to Look For
Upsloping T waves in precordial leads, V1-V6 (1-3mm)
Static, whereas Hyperacute T waves evolve → get serial EKG’s
ST depression at the J point, >1mm
Mild ST elevation in aVR (0.5-1mm)
ST elevation in aVL sometimes also seen
The most prominent ST depression and highest T waves noted in V3
Management - PCI within 2 hours of presentation
Wellens Syndrome
Here is an example of Wellens with Type A waves from LIFTL (https://litfl.com/wellens-syndrome-ecg-library/)
These EKG changes typically represent critical LAD stenosis (either plaque or spasm). Patients may present with chronic chest pain or history of recent chest pain that is usually typical, anginal pain. Notably, the classic T wave patterns are seen only during chest pain-free episodes, not during active chest pain. Troponin levels are usually either normal or minimally elevated (only 12% reported to have abnormal troponin vales in 1 study)
What Patterns to Look For?
T wave morphology, typically in precordial leads, particularly V2 and V3
Type A: initial positive deflection (~25%)
Type B: deep, symmetric T wave inversions
Note: Type A can evolve into Type B if stenosis persists
Type A: biphasic with initial positive deflection https://litfl.com/wellens-syndrome-ecg-library/
Type B: negative inverted T waves, symmetric https://litfl.com/wellens-syndrome-ecg-library/
Isoelectric or slight (<1mm) ST elevation in precordial leads
Abnormal R wave progression
Absence of Q waves in precordial leads
Pseudonormalization
T waves flip and can even become hyperacute during periods of chest pain. This should be terrifying rather than reassuring, as it can indicate complete occlusion of the affected artery. Dr. Smith’s ECG blog shows a great example of this “stuttering” pattern of occlusion/reperfusion cycle in a patient with Wellen’s Syndrome.
Wellens Mimics
There are both cardiac and non-cardiac causes of T wave inversions. PE is one of the most common ECG patterns that can look like anterior ischemia. Also found a variety of case studies outlining cases of “pseudo-Wellens” related to toxicologic sources including marijuana, PCP, or cocaine use. There are also cases of intermittent LBBB and acute cholecystitis being associated with a pseudo-Wellens phenomenon. Takotsubo cardiomyopathy is another Wellens mimic thought to be related to myocardial edema (Miner, 2019). LVH and HTN are also noted to be causes of pseudo-Wellens, so just be aware and take into account the likelihood that the patient is presenting with ACS.
Wellens in the setting of LBBB? It is possible for the Wellens morphology to be seen in the setting of LBBB. A published case report from 2017 (Meyers, 2017) describes the presentation of a 65 yo male with PMH of SCC of head and neck, with 1 hour history of chest pain and dyspnea. The initial EKG, done while the patient was having active chest pain demonstrated a LBBB that did not meet Sgarbossa criteria. On a repeat EKG done after chest pain resolved, the Wellens morphology of the t-waves are clearly visible.
Management Considerations
PCI definitive, but this is pre-infarct state rather than a complete occlusion. You would likely either see pseudonormalization or progressive to ST elevation if the vessel completely occludes as discussed in pseudonormalization section.
Why is urgent PCI important?
75% found to go on to have anterior wall STEMI per original study from 1982, at a mean of 8.5 days from admission (de Zwaan, 1982)
In a follow up study, found that all patients with Wellens T wave morphology had at least 50% occlusion of the LAD (de Zwaan, 1989)
Do not stress test these patients for theoretic risk of inciting AMI (although this risk is based primarily on case studies)
Posterior STEMI
This typically represents a left circumflex or RCA occlusion. It is often seen in the setting of inferior STEMI (15-20%) and isolated posterior STEMI is less likely (~8% of infarcts)
What Patterns to Look For
ST depression in V1-V3 (at least 1mm)
Tall broad R waves
Upright T waves
Dominant R/S ratio >1 in V2 (think of this as the Q wave equivalent, so can be absent in early infarctions)
Note: The inferior and lateral with posterior extension (seen in the first 2 EKGs in the slideshow below) are more worrisome given the larger infarct area. Duration of the STD in the right precordial leads is also suggestive of worse outcome
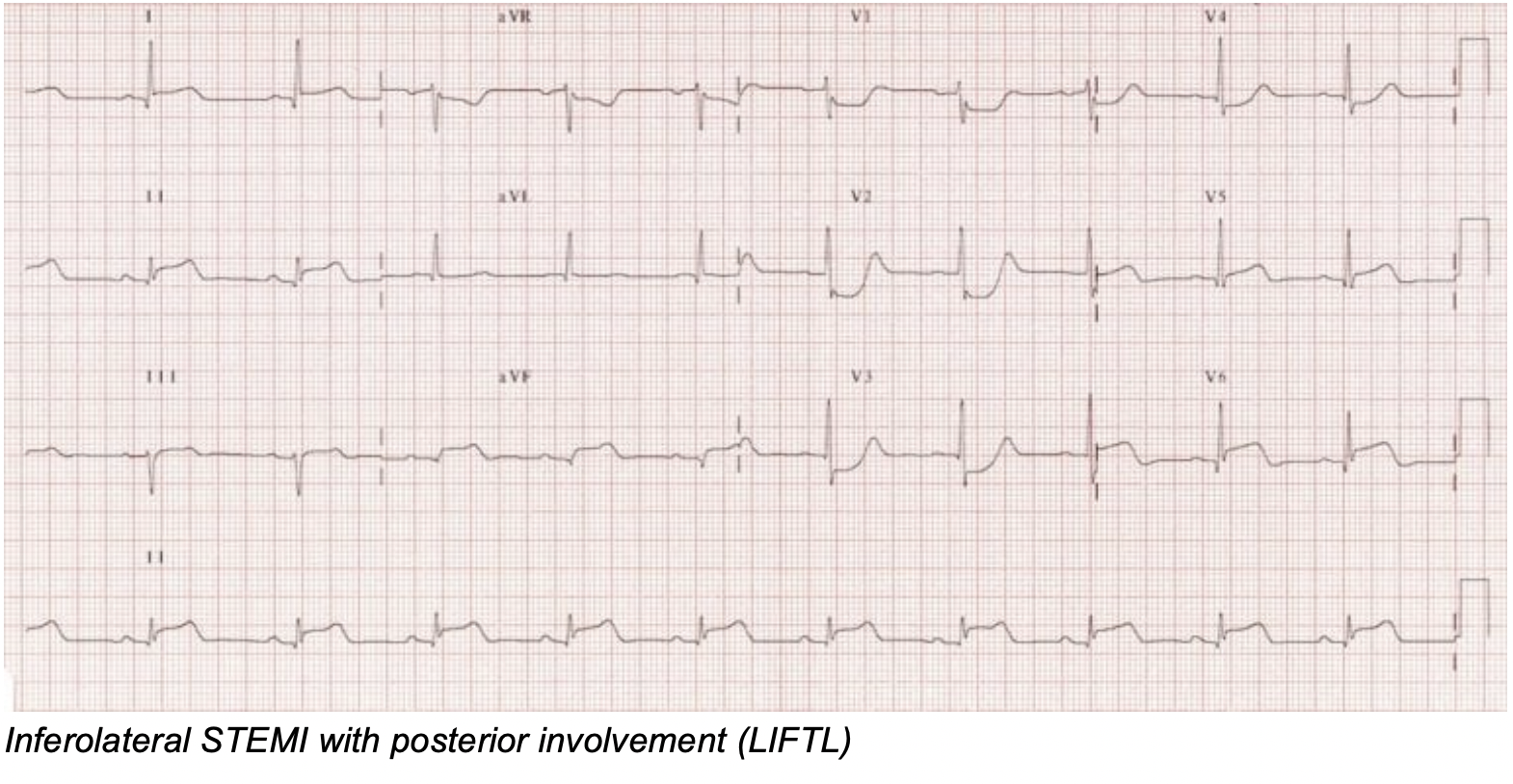
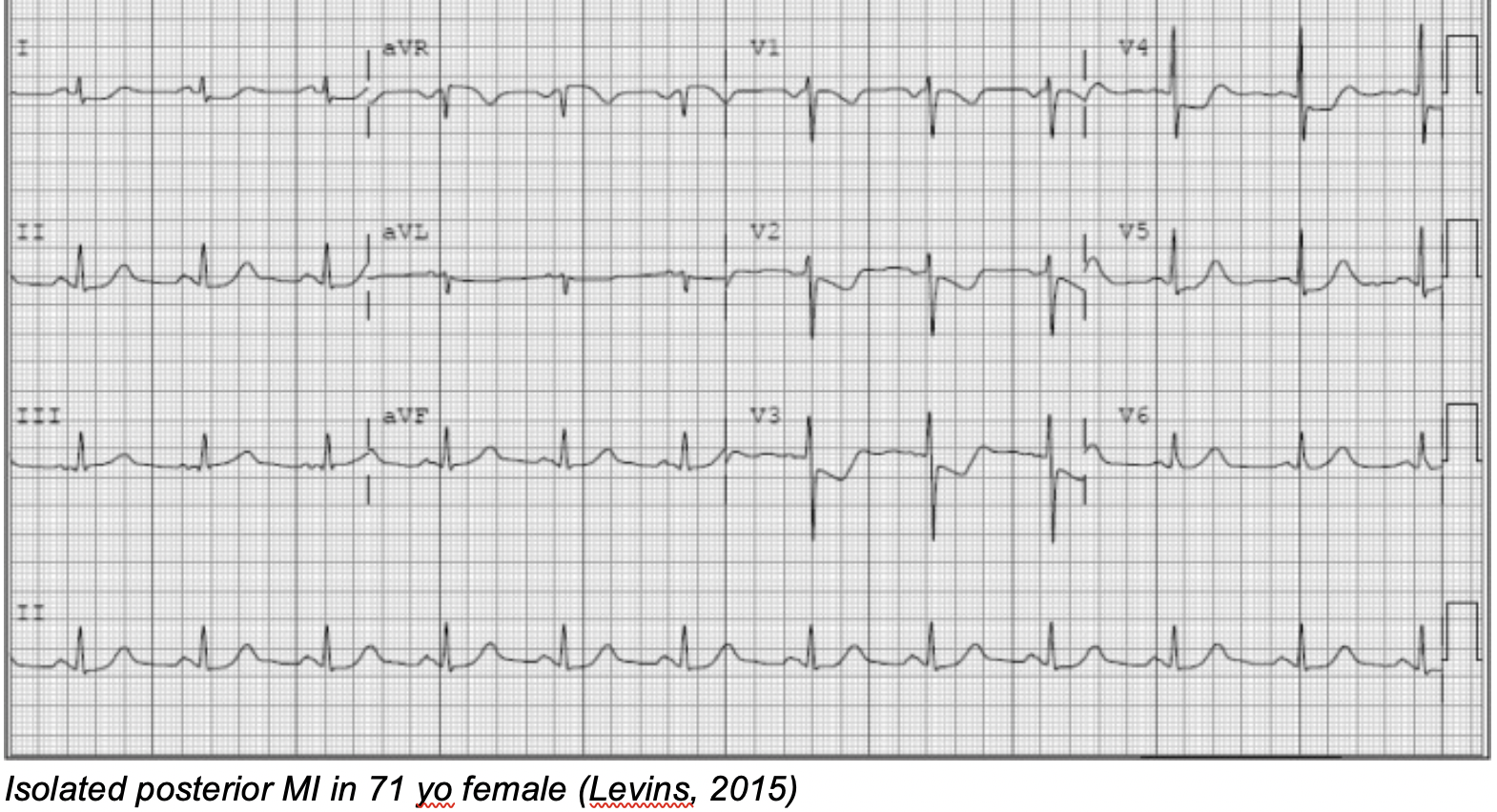
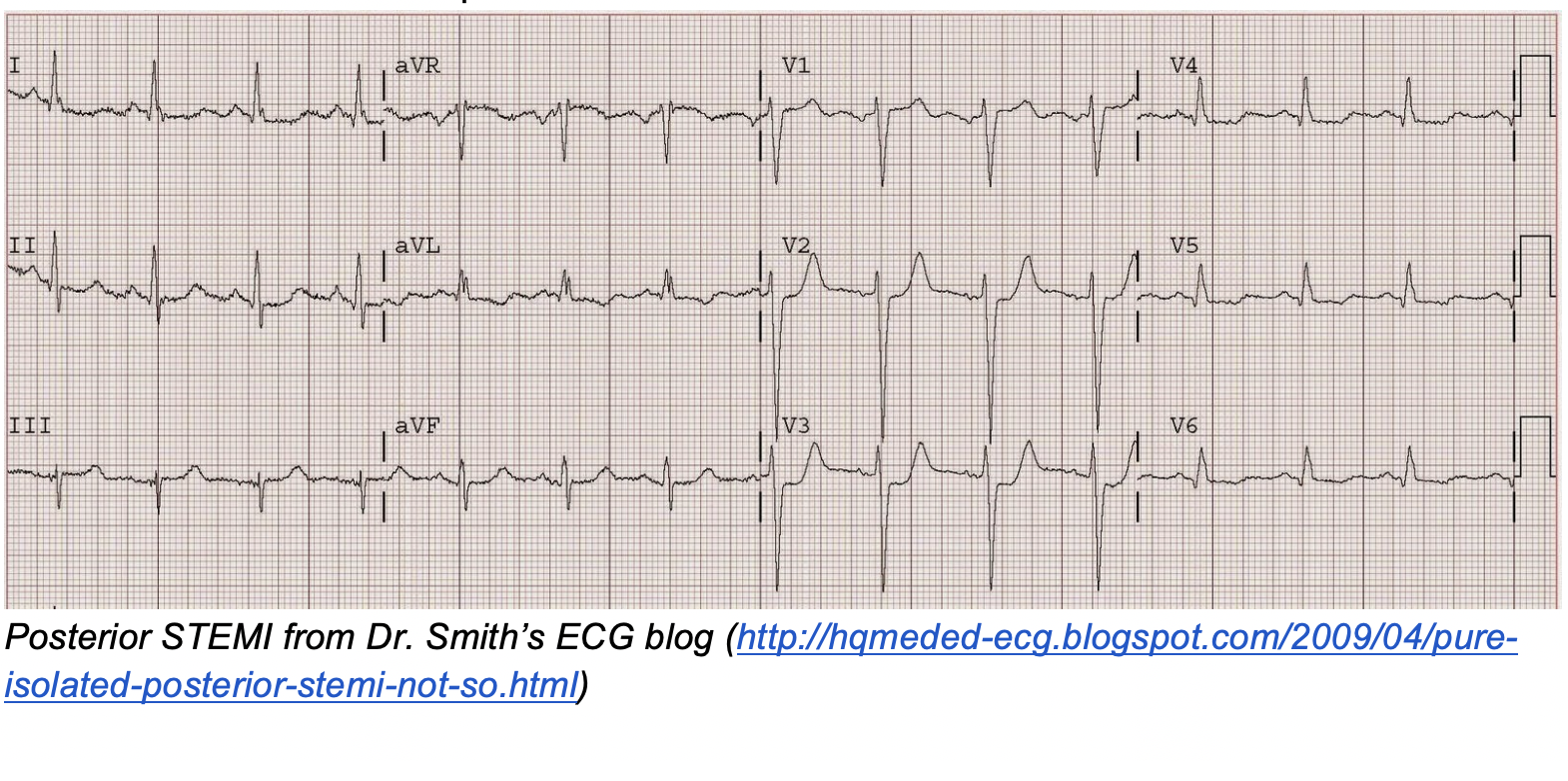
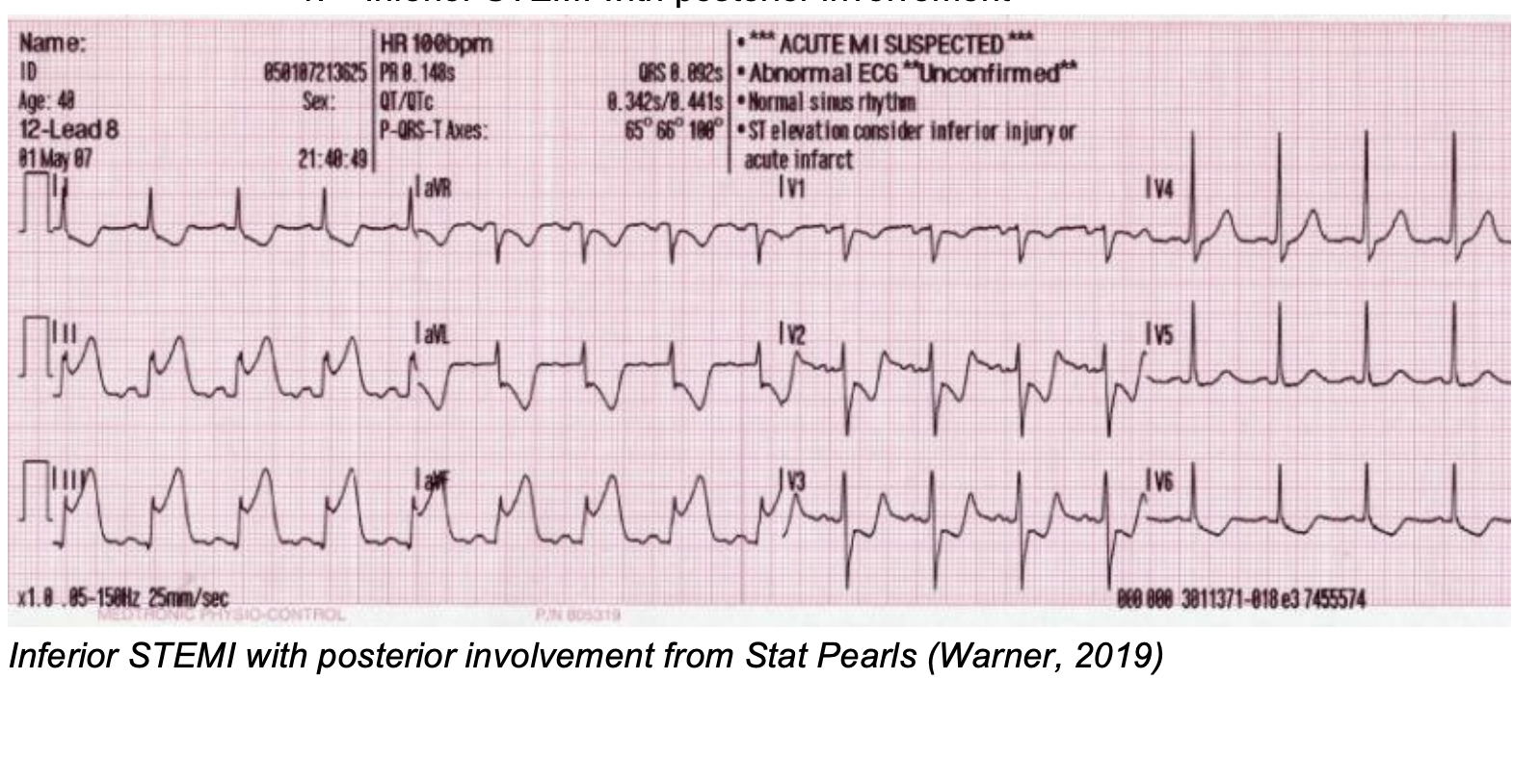
Management - Immediate reperfusion
Posterior EKG Lead Placement - Courtesy https://litfl.com/posterior-myocardial-infarction-ecg-library/
Can perform a posterior EKG (replace leads V4-V6 with V7-V9) to differentiate true posterior involvement from reciprocal changes related to inferior STEMI. Leads should show a typical STEMI pattern (with V9 having the best PPV)
Look for ST morphology
Tends to be more horizontal, although noted that it can be both upsloping and downsloping
Note that STE in posterior leads does not have to be as elevated as typical STEMI criteria, given distance between chest wall and posterior leads
T wave morphology - More likely to be upright, but can be inverted in very early infarcts
(EM Resident, 2019) https://www.emra.org/emresident/article/stemi-equivalents/
T wave inversions in aVL
These can represent mid-segment LAD lesions but can also be seen in LVH or LBBB
High specificity for isolated T waves (86.9%, although this was small number and in a Japanese single center, retrospective study) but very low sensitivity (Nakanishi, 2016).
Other studies showed a sensitivity of 76.7% in isolated T wave inversions in aVL, specificity of 71.4%. Again, single center with low numbers (Hassen, 2014).
Note: specificity of T wave inversions in aVL were increased when included with other T wave changes, specifically in lead I
RV infarction
Along with posterior MI, you may want to look at RV infarction when you see an inferior MI. Right ventricular infarctions are noted to occur with as many as 40% of inferior AMI. They typically do not occur in isolation, due to improved collateral blood supply of the right ventricle and overall smaller mass of this chamber. The importance of recognizing this pathology is that it is a preload dependent state, meaning that these patients are prone to becoming hypotensive. Initial management of this state revolves around avoiding nitrates, and giving fluids should they become hypotensive.
What Patterns to Look For?
Schematic of right-sided EKG from LIFTL https://litfl.com/right-ventricular-infarction-ecg-library/
You will typically see ST elevation in the right facing leads, namely V1 and III. You may also consider obtaining a right-sided EKG. V4R is thought to be the most sensitive lead for showing a right ventricular infarct, with high sensitivity (88%), specificity (78%). The following EKG findings are listed below, as well as how to perform a right-sided EKG:
ST elevation in V1 with ST depression in V2
ST elevation in III>II
ST elevation in V4R
Right-sided conduction blocks including RBBB and complete conduction blocks are also associated with RV infarction. In a review article from NEJM, found that these high grade conduction blocks can occur upwards of 48% of RV infarctions. One additional factor to note is the transient nature of this ST elevation, with many resolving 10 hours prior to presentation.
Example EKGs
Inferior STEMI with right-sided leads, showing RV infarction (LIFTL). Note the inferior STEMI, particularly the ST elevation in III>II along with the diagnostic ST elevation in V4R.
Below is a slightly trickier one from Dr.Stephen Smith’s ECG blog
http://hqmeded-ecg.blogspot.com/2018/07/is-there-right-ventricular-mi-in.html
Any RV MI? While ST elevation in V1 can cue you into considering a right ventricular MI, keep in mind that this can have low sensitivity, and you may want to go ahead and get a right sided EKG if you see evidence of an inferior MI.
Here’s the right-sided leads for the above patient, clearly showing ST elevation in V4R
http://hqmeded-ecg.blogspot.com/2018/07/is-there-right-ventricular-mi-in.html
References
Ahmed A. Harhash, Jennifer J. Huang, Sridhar Reddy, Balaji Natarajan, Mahesh Balakrishnan, Ranjith Shetty, Mathew D. Hutchinson, Karl B. Kern, aVR ST Segment Elevation: Acute STEMI or Not? Incidence of an Acute Coronary Occlusion. (2019)The American Journal of Medicine, 132 (5): 622-30. https://doi.org/10.1016/j.amjmed.2018.12.021.
Alam, Amit, et al. “IS AN ISOLATED ST SEGMENT ELEVATION IN LEAD AVR ASSOCIATED WITH HIGH GRADE CORONARY ARTERY DISEASE? SYSTEMATIC REVIEW.” JACC, Journal of the American College of Cardiology, 1 May 2019, www.onlinejacc.org/content/73/9_Supplement_1/552.
Barrabés, José A., et al. “Prognostic Value of Lead AVR in Patients With a First Non–ST-Segment Elevation Acute Myocardial Infarction.” Circulation, 28 July 2003, www.ahajournals.org/doi/full/10.1161/01.CIR.0000084553.92734.83.
Brady, William J, et al. “Electrocardiographic Manifestations: Acute Posterior Wall Myocardial Infarction.” The Journal of Emergency Medicine, Elsevier, 15 May 2001, www.sciencedirect.com/science/article/abs/pii/S0736467901003183.
Burns, Ed, and Andrew Chatfield. “LMCA Occlusion: ST Elevation in AVR • LITFL • ECG Library Diagnosis.” Life in the Fast Lane • LITFL • Medical Blog, 16 Mar. 2019, litfl.com/lmca-occlusion-st-elevation-in-avr/.
Burns, Ed. “De Winter T Wave • LITFL • ECG Library Diagnosis.” Life in the Fast Lane • LITFL • Medical Blog, 24 Sept. 2019, litfl.com/de-winter-t-wave-ecg-library/.
Carrington, Mafalda, et al. “De Winter Pattern: a Forgotten Pattern of Acute LAD Artery Occlusion.” BMJ Case Reports, BMJ Publishing Group, 8 Nov. 2018, casereports.bmj.com/content/2018/bcr-2018-226413.
de Winter, Robbert J, et al. “A New ECG Sign of Proximal LAD Occlusion.” The New England Journal of Medicine, U.S. National Library of Medicine, 6 Nov. 2008, www.ncbi.nlm.nih.gov/pubmed/18987380/.
de Zwaan, C, et al. “Angiographic and Clinical Characteristics of Patients with Unstable Angina Showing an ECG Pattern Indicating Critical Narrowing of the Proximal LAD Coronary Artery.” American Heart Journal, U.S. National Library of Medicine, Mar. 1989, www.ncbi.nlm.nih.gov/pubmed/2784024.
de Zwaan, C, et al. “Characteristic Electrocardiographic Pattern Indicating a Critical Stenosis High in Left Anterior Descending Coronary Artery in Patients Admitted Because of Impending Myocardial Infarction.” American Heart Journal, U.S. National Library of Medicine, Apr. 1982, www.ncbi.nlm.nih.gov/pubmed/6121481.
Hanna, Elias, and David Glancy. “ST-Segment Depression and T-Wave Inversion: Classification, Differential Diagnosis, and Caveats.” Cleveland Clinic Journal of Medicine, 12 June 2018, www.mdedge.com/ccjm/article/95520/cardiology/st-segment-depression-and-t-wave-inversion-classification-differential/page/0/1.
Hassen, Getaw Worku, et al. “The Neglected Lead on Electrocardiogram: T Wave Inversion in Lead AVL, Nonspecific Finding or a Sign for Left Anterior Descending Artery Lesion?” The Journal of Emergency Medicine, Elsevier, 25 Nov. 2013, www.sciencedirect.com/science/article/abs/pii/S0736467913010706.
Ibanez, et al. “2017 ESC Guidelines for the Management of Acute Myocardial Infarction in Patients Presenting with ST-Segment Elevation: The Task Force for the Management of Acute Myocardial Infarction in Patients Presenting with ST-Segment Elevation of the European Society of Cardiology (ESC).” OUP Academic, Oxford University Press, 26 Aug. 2017, academic.oup.com/eurheartj/article/39/2/119/4095042.
Inayat, Faisal, et al. “Pseudo-Wellens' Syndrome Secondary to Concurrent Cannabis and Phencyclidine Intoxication.” BMJ Case Reports, BMJ Publishing Group, 30 June 2018, casereports.bmj.com/content/2018/bcr-2018-225755.
Kinch, Jack W. “Right Ventricular Infarction: NEJM.” New England Journal of Medicine, 8 Sept. 1994, www.nejm.org/doi/full/10.1056/NEJM199404283301707?casa_token=RlXIfQeLJ0EAAAAA%3A9dsxNqpExxYjyKIqeddPAr9FsRNchgrVTnWXoRM0mddOsZ2dMRtLLv9R96SVKAHhZBjwarQoDEQ.
Kosuge, Masami, et al. “An Early and Simple Predictor of Severe Left Main and/or Three-Vessel Disease in Patients With Non–ST-Segment Elevation Acute Coronary Syndrome.” The American Journal of Cardiology, Excerpta Medica, 22 Dec. 2010, www.sciencedirect.com/science/article/abs/pii/S0002914910020886.
Kreider, Daniel, and Jeremy Berberian. “STEMI Equivalents: Can't-Miss Patterns.” EMRA, 9 June 2019, www.emra.org/emresident/article/stemi-equivalents/.
Kulkarni, Anand U., et al. “Clinical Use of Posterior Electrocardiographic Leads: A Prospective Electrocardiographic Analysis during Coronary Occlusion.” American Heart Journal, Mosby, 31 Aug. 2004, www.sciencedirect.com/science/article/abs/pii/S000287039690280X.
Larkin, John. “ECG Case 084 • LITFL • ECG Top 100 Self-Assessment Quiz.” Life in the Fast Lane • LITFL • Medical Blog, 30 Apr. 2019, litfl.com/ecg-case-084/
Levis, Joel T. “ECG Diagnosis: Isolated Posterior Wall Myocardial Infarction.” The Permanente Journal, The Permanente Journal, 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC5293126/.
Mead, Nicole E, and Kelly P O'Keefe. “Wellen's Syndrome: An Ominous EKG Pattern.” Journal of Emergencies, Trauma, and Shock, Medknow Publications, Sept. 2009, www.ncbi.nlm.nih.gov/pmc/articles/PMC2776372/#CIT1.
Meyers, H. Pendell, and Stephen W. Smith. “Dynamic T-Wave Inversions in the Setting of Left Bundle Branch Block.” The American Journal of Emergency Medicine, W.B. Saunders, 24 Dec. 2016, www.sciencedirect.com/science/article/abs/pii/S0735675716309639?via%3Dihub.
Miner, Brianna. “Wellens Syndrome.” StatPearls [Internet]., U.S. National Library of Medicine, 9 Mar. 2019, www.ncbi.nlm.nih.gov/books/NBK482490/.
Morris, Niall, and Laura Howard. “BET 1: IN PATIENTS WITH SUSPECTED ACUTE CORONARY SYNDROME, DOES WELLENS' SIGN ON THE ELECTROCARDIOGRAPH IDENTIFY CRITICAL LEFT ANTERIOR DESCENDING ARTERY STENOSIS?” Emergency Medicine Journal, BMJ Publishing Group Ltd and the British Association for Accident & Emergency Medicine, 1 Apr. 2017, emj.bmj.com/content/34/4/264.2.
Morris, Niall, and Richard Body. “The De Winter ECG Pattern: Morphology and Accuracy for Diagnosing Acute Coronary Occlusion: Systematic Review.” Latest TOC RSS, Wolters Kluwer, 1 Aug. 2017, www.ingentaconnect.com/content/wk/ejeme/2017/00000024/00000004/art00002.
Nakanishi, Nobuto, et al. “Does T Wave Inversion in Lead AVL Predict Mid-Segment Left Anterior Descending Lesions in Acute Coronary Syndrome? A Retrospective Study.” BMJ Open, British Medical Journal Publishing Group, 1 Jan. 2016, bmjopen.bmj.com/content/6/2/e010268.
Rezaie, Salim. “REBEL Cast Episode 23: Is ST-Segment Elevation in Lead AVR Getting Too Much Respect? with Amal Mattu.” REBEL EM - Emergency Medicine Blog, 22 Mar. 2019, rebelem.com/is-st-segment-elevation-in-lead-avr-getting-too-much-respect-with-amal-mattu/.
Rezaie, Salim. “REBEL ECG of the Week #8.” REBEL EM - Emergency Medicine Blog, 14 Mar. 2019, rebelem.com/r-e-b-e-l-ecg-week-wellens-syndrome-stemi-2/.
Rich, Michael W., et al. “Electrocardiographic Diagnosis of Remote Posterior Wall Myocardial Infarction Using Unipolar Posterior Lead V9.” Chest, Elsevier, 14 Jan. 2016, www.sciencedirect.com/science/article/abs/pii/S0012369215460556.
Rokos, Ivan C., et al. “Appropriate Cardiac Cath Lab Activation: Optimizing Electrocardiogram Interpretation and Clinical Decision-Making for Acute ST-Elevation Myocardial Infarction.” American Heart Journal, Mosby, 10 Dec. 2010, www.sciencedirect.com/science/article/abs/pii/S0002870310007581?via%3Dihub#t0010.
Rostoff, Paweł, et al. “Value of Lead AVR in the Detection of Significant Left Main Coronary Artery Stenosis in Acute Coronary Syndrome.” Kardiologia Polska, U.S. National Library of Medicine, Feb. 2005, www.ncbi.nlm.nih.gov/pubmed/15815796.
Sedhai, Yub Raj, et al. “Pseudo-Wellens' Syndrome in Pulmonary Embolism.” BMJ Case Reports, BMJ Specialist Journals, 1 Nov. 2018, casereports.bmj.com/content/11/1/e227464.long.
Smith , Stephen. “Is There a Right Ventricular MI in Addition to Infero-Postero-Lateral MI?” Dr. Smith's ECG Blog, July 2018, hqmeded-ecg.blogspot.com/2018/07/is-there-right-ventricular-mi-in.html.
Smith, Stephen, et al. “Pure (Isolated) Posterior STEMI -- Not so Rare, but Often Ignored!” Dr. Smith's ECG Blog, Apr. 2009, hqmeded-ecg.blogspot.com/2009/04/pure-isolated-posterior-stemi-not-so.html.
“ST-Elevation in AVR with Diffuse ST-Depression: An ECG Pattern That You Must Know and Understand!” Dr. Smith's ECG Blog, Feb. 2018, hqmeded-ecg.blogspot.com/2018/02/st-elevation-in-avr-with-diffuse-st.html.
Tamura, Akira. “Significance of Lead AVR in Acute Coronary Syndrome.” World Journal of Cardiology, Baishideng Publishing Group Inc, 26 July 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4110611/.
Tandy, Thomas K, et al. “Wellens' Syndrome.” Annals of Emergency Medicine, Mosby, 4 Nov. 2005, www.sciencedirect.com/science/article/abs/pii/S0196064499703732.
Tzimas, Georgios, et al. “Atypical Electrocardiographic Presentations in Need of Primary Percutaneous Coronary Intervention.” The American Journal of Cardiology, U.S. National Library of Medicine, 15 Oct. 2019, www.ncbi.nlm.nih.gov/pubmed/31455501.
Verouden, J, et al. “Persistent Precordial ‘Hyperacute’ T-Waves Signify Proximal Left Anterior Descending Artery Occlusion.” Heart, BMJ Publishing Group Ltd, 15 Oct. 2009, heart.bmj.com/content/95/20/1701.long.
Warner, Matthew J. “Myocardial Infarction, Inferior.” StatPearls [Internet]., U.S. National Library of Medicine, 11 Jan. 2019, www.ncbi.nlm.nih.gov/books/NBK470572/.
Win Htut Oo, Swe Zin Mar, et al. “Omnious T-Wave Inversions: Wellens' Syndrome Revisited.” Journal of Community Hospital Internal Medicine Perspectives, Co-Action Publishing, 7 Sept. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5016748/.
Yamaji H, Iwasaki K, Kusachi S, Murakami T, Hirami R, Hamamoto H, Hina K, Kita T, Sakakibara N, Tsuji T. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography. ST segment elevation in lead aVR with less ST segment elevation in lead V(1) J Am Coll Cardiol. 2001;38:1348–1354
Zwaan, Chris de, et al. “Angiographic and Clinical Characteristics of Patients with Unstable Angina Showing an ECG Pattern Indicating Critical Narrowing of the Proximal LAD Coronary Artery.” American Heart Journal, Mosby, 25 Feb. 2004, www.sciencedirect.com/science/article/abs/pii/0002870389907424?via%3Dihub.
Zwaan, Chris de, et al. “Characteristic Electrocardiographic Pattern Indicating a Critical Stenosis High in Left Anterior Descending Coronary Artery in Patients Admitted Because of Impending Myocardial Infarction.” American Heart Journal, Mosby, 27 Feb. 2004, www.sciencedirect.com/science/article/abs/pii/000287038290480X.
Written by Laura Frankenfeld, MD PGY-1 University of Cincinnati Department of Emergency Medicine
Peer Review and Editing by Jeffery Hill, MD MEd





