Heart Blocks: A Primer
/Summary and quick hits
- Recognizing a heart block on an EKG or monitor is important, but always start your evaluation with assessment of vitals, airway, breathing, circulation and clinically correlate your findings
- Heart blocks can be a sign of underlying pathology such as MI, Lyme disease, myocarditis, structural heart disease, pulmonary embolism, autoimmune disease, electrolyte disturbances, medication side effects, Lenegre’s or Lev’s disease, increased vagal tone, or could be a normal variant
- Distinguishing between a 2nd degree Mobitz type 1 and type 2 block can determine whether a patient needs admission and can be difficult to determine in a 2:1 block. Vagal maneuver, PR interval, and QRS length can help you distinguish the two
- In isolation, asymptomatic patients with a 1st degree AV block or 2nd degree Mobitz type 1 block can be discharged with follow-up
- High grade 2nd degree, 2nd degree Mobitz type 2 and 3rd degree AV blocks require admission for pacemaker placement and/or evaluation
- Treatment with Atropine is indicated in bradycardic, symptomatic and/or unstable patients with a 1st or 2nd degree Mobitz type 1 AV block. It is unlikely to be affective in high grade blocks as the block is usually below the AV node
- Atropine can still be used as a temporizing measure while setting up for transcutaneous pacing and/or transvenous pacemaker placement in high grade blocks
- In symptomatic or unstable bradycardic patients, have the transcutaneous pacer pads placed while simultaneously administering chronotropic agents such as Epinephrine; pacing is definitive treatment
- If transcutaneous pacing and chronotropic treatment is ineffective, prepare for transvenous pacing and obtain expert consultation
Brief heart block physiology
In the cardiac conduction system, electrical signals arise from the sinoatrial node spontaneously and travel to the atrioventricular node through the atria. After a brief pause, the stimulus is conducted from the AV node through the bundle of His to the ventricular Purkinje fibers through the left and right bundle branches. The SA node is located at the junction of the right atrium and superior vena cava, with blood supply coming from the right coronary artery in 55% of patients and the left circumflex artery in 45% of patients [1]. It is the dominant pacemaker and maintains a rate between 60-90 bpm in most adults. Disease of the SA node, such as in sinus arrest or sinoatrial exit block, the SA node fails to create an impulse and no atrial contraction is produced. Sick sinus syndrome and Bradycardia-Tachycardia syndrome are examples of SA node disease. When the SA or AV node fails to generate a spontaneous impulse, other myocardial tissue can assume the role, such as an atrial, junctional or ventricular focus.
The AV node is located within the interatrial septum, with blood supply coming from the RCA in 90% of patients and the LCA in 10% of patients [1]. The AV node has a slower intrinsic rate of 40-60 bpm. Disease of the AV node can occur at different locations within and below the AV node, and can cause characteristic blocks such as 1st, 2nd and 3rd degree AV blocks. The location of the block will determine what escape rhythm is produced, such as junctional or ventricular. In most cases, if the block occurs within the AV node, a junctional escape rhythm is produced with a rate between 40-60 bpm, which creates a narrow QRS complex [1]. If the block occurs below the AV node, a ventricular escape rhythm is produced with a rate between 20-40 bpm creating a wide QRS complex [1]. A left and right bundle branch block will also cause unsynchronized ventricular contraction, with widening of the QRS complex and create characteristic changes on an electrocardiogram.
The AV node terminates at the bundle of His, which splits into the left and right bundle branches in the interventricular septum. The left bundle branch is short and splits into the left anterior and posterior fascicle. The posterior fascicle has dual blood supply and is particularly resistant to ischemic damage. The left and right bundle branches taper out to produce numerous Purkinje fibers which stimulate myocardial contraction. Disease of these fascicles and bundle branches can lead to a left or right bundle branch block, left anterior or posterior fascicular block, bifascicular block or a trifascicular block.
Brief heart block summary
Sinus arrest/block and sinoatrial exit block- Sinus node dysfunction, SA node misses one or more cycles. This missed cycle or pause may induce an escape response. Sick sinus syndrome and Bradycardia-Tachycardia syndrome are examples [2].
Figure 1. Sinoatrial exit block. https://hqmeded-ecg.blogspot.com.au/search/label/sino-atrial%20exit%20block
AV Blocks- Blocks that delay or prevent atrial impulses from reaching the ventricles. A 1st degree AV block and 2nd degree type 1 Wenckebach are usually caused by impaired conduction within the AV node, while a 2nd degree Mobitz type 2 is caused by impaired conduction just below the AV node. A 3rd degree AV block is caused by a complete block of conduction within or below the AV node [1].
- 1st degree AV block- Prolonged PR interval greater than 0.2 seconds or one large square [2].
Figure 2. First degree AV block. https://lifeinthefastlane.com/ecg-library/basics/first-degree-heart-block/
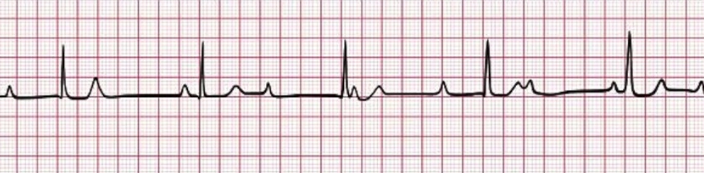
- 2nd degree Mobitz type 1, Wenckebach- Progressive prolongation of the PR interval with a non-conducted p wave, no ventricular conduction [2].
Figure 3. Second degree, Mobitz 1. https://lifeinthefastlane.com/ecg-library/basics/wenckebach/
- 2nd degree Mobitz type 2- Intermittent non-conducted P waves without PR interval prolongation, with regular and constant P waves [2].
Figure 4. Second degree, Mobitz 2. https://lifeinthefastlane.com/ecg-library/basics/mobitz-2/
- 2nd degree high grade AV block- P:QRS ratio of 3:1 or higher producing an extremely slow ventricular rate [2].
Figure 5. High grade AV block. https://lifeinthefastlane.com/ecg-library/basics/high-grade-block/
- 3rd degree AV block- Complete dissociation between atrial and ventricular contraction, no association between P waves and QRS complexes [2].
Figure 6. Third degree AV block. https://lifeinthefastlane.com/ecg-library/basics/complete-heart-block/
LBBB- When damage to the left bundle branch occurs, the direction of septal depolarization is reversed and becomes right to left, the impulse spreads first to the right ventricle via the right bundle branch and then to the left ventricle via the septum. This extends the QRS duration, produces a broad/notched R wave in the lateral leads, deep S waves in the precordial leads and at times LAD.
- Wide QRS, dominant S wave in V1, Broad R waves in leads 1, aVL, V5-V6, No Q waves in leads 1 and V5-V6 [2].
Figure 7. Left bundle branch block. https://lifeinthefastlane.com/ecg-library/basics/left-bundle-branch-block/
RBBB- When damage to the right bundle branch occurs, depolarization of the right ventricle is delayed as it is spread through the septum from the left ventricle. The early part of the QRS complex is unchanged, delayed activation of the right ventricle creates the characteristic secondary R wave (R’) in V1-V3 and wide S waves in the lateral leads.
- Wide QRS, rsr’ pattern in V1-V3, wide/slurred S wave in the lateral leads [2].
Figure 8. Right bundle branch block. https://lifeinthefastlane.com/ecg-library/basics/right-bundle-branch-block/
Left Anterior Fascicular Block (LAFB)- LAD, Q waves in lead 1 and aVL, small R wave in lead 3 and absence of LVH [2].
Tip: In LAFB, aVL may meet voltage criteria for LVH, but there will be no LV strain.
Figure 9. Left anterior fascicular block. https://lifeinthefastlane.com/ecg-library/basics/left-anterior-fascicular-block/
Left Posterior Fascicular Block (LPFB) - RAD, small R wave in lead 1, small Q wave in lead 3 and absence of RVH [2].
Tip: LPFB is rare in isolation, seen most commonly with RBBB in the setting of a bifascicular block. Rule out other more significant causes of RAD such as acute PE, tricyclic overdose, lateral MI, RVH, etc.
Figure 10. Left posterior fascicular block. https://lifeinthefastlane.com/ecg-library/basics/left-posterior-fascicular-block
Bifascicular block- RBBB and either LAFB or LPFB [2].
Complete trifascicular block- presence of conducting disease in all three fascicles.
- Bifascicular block plus 3rd degree AV block [2].
Incomplete trifascicular block- three types [2].
- Bifascicular block plus first degree AV block
- Bifascicular block plus 2nd degree AV block
- RBBB plus alternating LAFB/LPFB
References
- Yealy, D. M., Kosowsky, J. M. (2014). Dysrhythmias. In Rosen's Emergency Medicine: Concepts and Clinical Practice 8th edition (pp. 1034-1046). Philadelphia, PA: Elsevier Saunders.
- Nickson, C. (2015, April 22). Heart Block and Conduction Abnormalities. Retrieved November 12, 2017, from https://lifeinthefastlane.com/ccc/heart-block-and-conduction-abnormalities/
Written by Diego Iparraguirre, MD, PGY-1 UC EM
Peer Review and Edited by Jeffery Hill, MD MEd