Back on the Block - Heart Blocks Part 2
/Case 1
A 43-year-old male with no significant medical history presents to the emergency department via EMS with an episode of pre-syncope. The episode occurred 30 minutes ago after getting out of a hot shower, and he is currently asymptomatic. Vitals per EMS were BP 130/88, HR 59, RR 20, O2 sat 99%, T 97.5, and BS 99. He currently appears comfortable and he is in no acute distress.
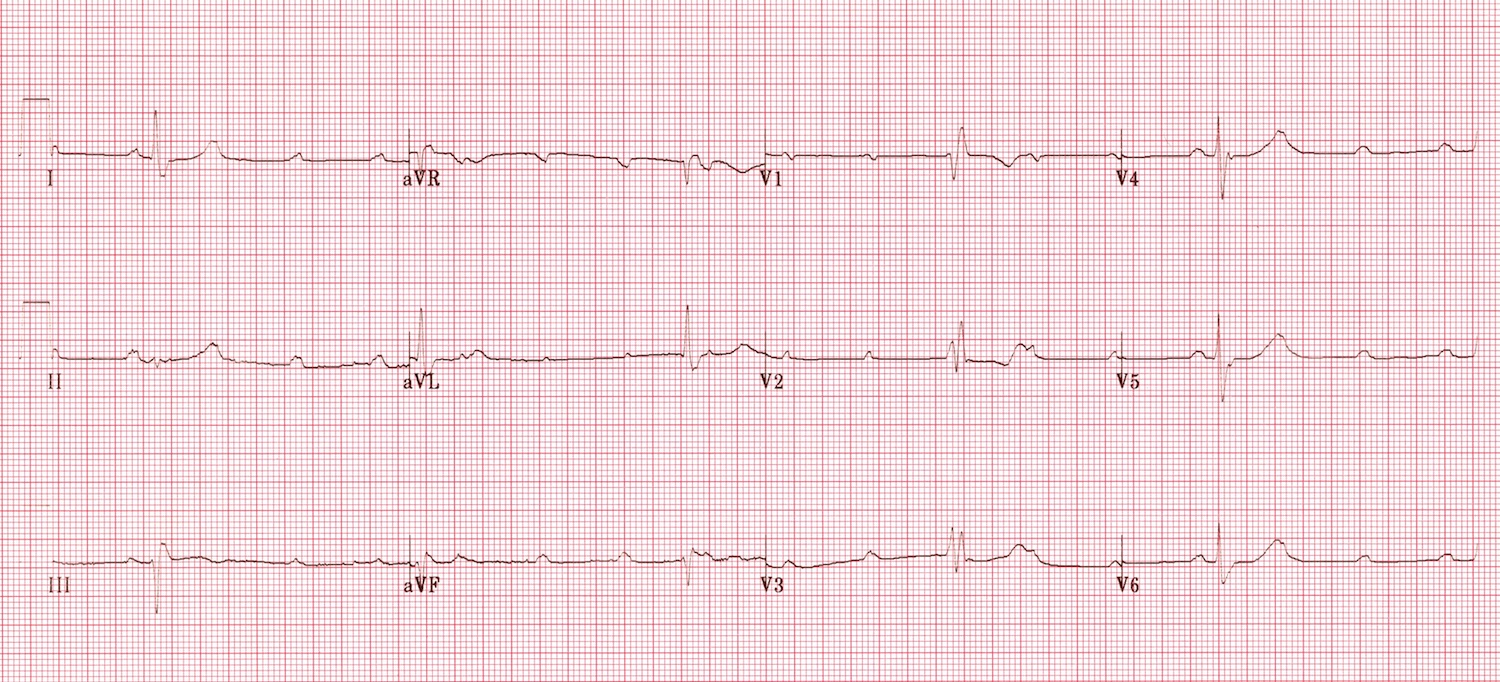
You are handed this EKG:
What is the conduction abnormality?
2nd degree Mobitz type 1, Wenckebach
Based on this patient’s EKG alone, does he require admission?
In isolation, a patient with a 1st degree AV block or 2nd degree Mobitz type 1 block can be discharged with follow-up. [2] These blocks are essentially benign but should be managed by the patients PCP
- 1st degree AV block does not cause hemodynamic instability and requires no specific treatment [2]
- 2nd degree Mobitz Type 1 can cause a minimal hemodynamic disturbance and rarely progresses to a 3rd degree AV block
- High grade 2nd degree AV block, 2nd degree Mobitz type 2 block and 3rd degree AV block have a high risk of hemodynamic compromise, syncope, ventricular standstill and sudden cardiac death. These blocks require admission for further work-up, cardiac monitoring, backup temporary pacing, permanent pacemaker evaluation and possible placement [2]
- LAFB and LPFB do not require admission, although disposition ultimately depends on patients symptoms and clinical context [2]
- Trifascicular block is always pathologic and requires admission for further evaluation of underlying cause and likely pacemaker placement [2]
Case 2
76-year-old female with a history of CAD, HTN and DM presents to the ED with dyspnea. Vitals are BP 110/76, HR 42, RR 22, O2 sat 94%, T 98.4, and BS 140. She appears uncomfortable and diaphoretic, but is otherwise in no acute distress.
Here’s her EKG Doc:
What is the conduction abnormality?
3rd degree AV block
The patient now complains of chest pain and starts feeling light-headed, she appears increasingly lethargic and her vitals are now deteriorating, BP 85/44 HR 32 RR 24 O2 sat 94%. How would you manage this patient?
- ABC’s, IV/O2/Monitor (if not already done) and place transcutaneous pacer pads. Per AHA/ACLS guidelines, Atropine, transcutaneous pacing, Epinephrine and Dopamine are used in symptomatic/unstable bradycardia, although Dopamine is less commonly used
- Atropine unlikely to treat a High grade AV block since the block is likely below the AV node, but can be used as a temporizing measure while pacer pads are placed and/or transvenous pacemaker is set-up 1
- Epinephrine is effective in a broader range of patients and provides a greater amount of hemodynamic support when compared to Atropine [3]
- A reasonable strategy is to attempt both electrical and medical therapy simultaneously, as it is unpredictable which therapy will work for which patient [3]
- If electrical and medical therapy fail, prepare for transvenous pacing and obtain expert consultation.
- Check out this great blog post by Dr. Mike Bohanske on transvenous pacemaker placement
- Assess for reversible causes, EKG to assess for STEMI or new ischemic changes and continue work-up. Disposition will be admission for the underlying cause, pacemaker evaluation and placement
Case 3
62-year-old male with a history of HTN, Hyperlipidemia, DM and 1 PPD smoker presents to the ED with chest pain that started 20 minutes ago while mowing his lawn. He is visiting from out of town. Vitals are BP 130/92, HR 96, RR 18, O2 sat 95%, T 98.3 and BS 95. He appears comfortable and in no acute distress.
You are handed this EKG (he has no old EKG):
What is the conduction abnormality?
Left Bundle Branch Block (LBBB)
Would you activate the cardiac cath lab? Why or Why Not?
No.
- A new LBBB is no longer a STEMI equivalent according to ACC guidelines. [4] According to current guidelines, a LBBB that is new or presumed new and an old LBBB are to be assessed equally [4]
- When evaluating a patient that has a LBBB on EKG, first assess for hemodynamic stability, if unstable and there is suspicion for MI, activate the cardiac cath lab for emergent reperfusion or fibrinolysis [4]
- If the patient is stable, interpret the EKG and use the modified Sgarbossa’s criteria [4] Sgarbossa Criteria:
- Concordant ST elevation > 1mm in leads with a positive QRS complex (score 5)
- Concordant ST depression > 1 mm in V1-V3 (score 3)
- Excessively discordant ST elevation > 5 mm in leads with a negative QRS complex (score 2)
- Score of greater than or equal to 3 is significant for STEMI Modified Sgarbossa Criteria:
- No longer uses a scoring system
- Concordant ST elevation > 1mm in leads with a positive QRS complex
- Concordant ST depression > 1 mm in V1-V3
- ST-elevation is “excessively discordant” when the ST-elevation (measured at the J-point) is > 0.25 or 25% the depth of the S-wave.
- ST-depression is “excessively discordant” when the ST-depression (measured at the J-point) is > 0.3 or 30% the height of the R-wave.
What is the disposition for this patient?
With a moderately suspicious presentation and negative cardiac markers, this patient has a heart score of at least 5. He requires admission for serial cardiac markers, serial EKG’s, echocardiogram, risk stratification and possible angiography.
What is the conduction abnormality
2:1 2nd degree AV Block
Is this a Wenckebach or type 2 AV block?
- This can be tricky, but in general, there are a couple of things you can look for to distinguish the two:
- PR interval tends to be prolonged in a type 1 block, whereas a wide QRS complex tends to make a type 2 block more likely [5]
- Vagal maneuver can also help, by having the patient perform a vagal maneuver this increases parasympathetic activity to the AV node and increases inhibition, if this leads to a high grade block such as a 3:1 or 4:1 block, a Mobitz type 1 is more likely [5]
- If vagal maneuver creates a 1:1 ratio or no change, a Mobitz type 2 is more likely [5]. If you are unable to determine if the block is a Mobitz type 1 or type 2, assume type 2 and admit the patient. Ultimately, evaluation to determine whether the patient has a Mobitz type 1 or 2 AV block is done by an electrophysiologist
What is the conduction abnormality?
- Complete trifascicular block: RBBB + LAD + 3rd degree heart block
- A trifascicular block is always pathologic, it requires admission for further evaluation and pacemaker evaluation and/or placement.
References
- Yealy, D. M., Kosowsky, J. M. (2014). Dysrhythmias. In Rosen's Emergency Medicine: Concepts and Clinical Practice 8th edition (pp. 1034-1046). Philadelphia, PA: Elsevier Saunders.
- Nickson, C. (2015, April 22). Heart Block and Conduction Abnormalities. Retrieved November 12, 2017, from https://lifeinthefastlane.com/ccc/heart-block-and-conduction-abnormalities/
- Farkas, J. (2017, February 13). PulmCrit- Epinephrine vs. atropine for bradycardic periarrest. https://emcrit.org/pulmcrit/epinephrine-atropine-bradycardia/
- Wilner, B., De Lemos, J. A., Neeland, I. J. (2017, February 28). LBBB in Patients With Suspected MI: An Evolving Paradigm. Retrieved November 12, 2017, from http://www.acc.org/latest-in-cardiology/articles/2017/02/28/14/10/lbbb-in-patients-with-suspected-mi
- Dubin, D. (2000, October 15), Rhythm, Part II: Blocks. In Rapid Interpretation of EKG’s 6th Edition (pp. 173-191). Cover Pub Co.
Author: Diego Iparraguirre, MD, PGY-1
Peer Review: Nicholas Ludmer, PGY-4, Jeffery Hill, MD MEd
Posting: Jeffery Hill, MD MEd