Twisting and Turning - Ankle Injuries in the ED
/BACKGROUND
Ankle injuries are among the most common reasons for ED visits [1]. Ankle fractures are the third most common fracture in the ED [2] and more than 20,000 patients are seen in the ED for ankle sprains each day [3]. Ankle injuries have financial implications for both the healthcare system and patients. Within the Medicare population alone, foot and ankle surgeries are responsible for more than 11 billion dollars spent annually [4]. Furthermore, a patient’s ability to work can be affected both by initial result of injury (e.g., weight bearing status, discomfort) or any sequelae (e.g., nonunion, post-traumatic arthritis or deformity).
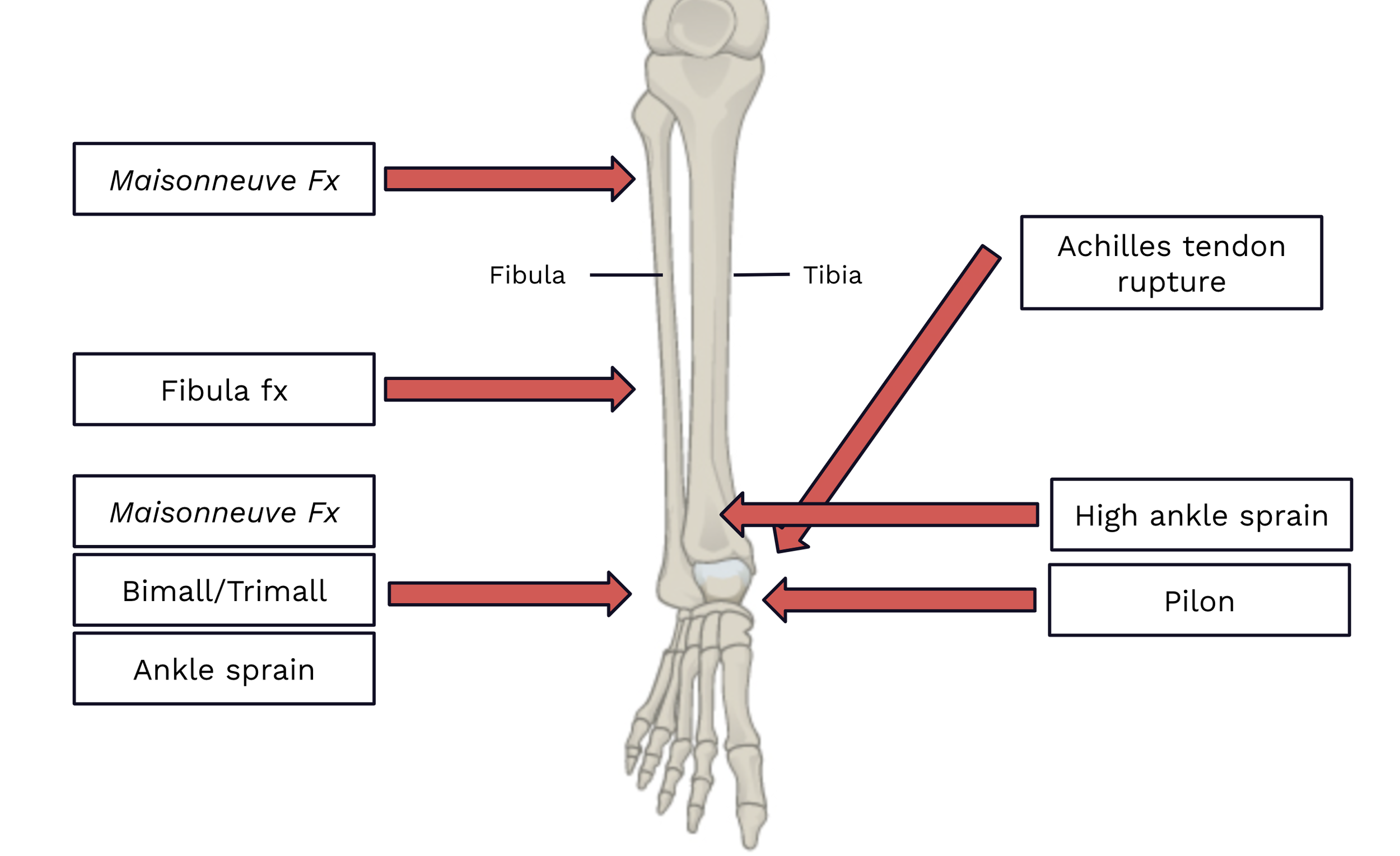
As an EM physician, it is important to have an understanding of the spectrum of ankle injuries and how these are appropriately evaluated. Certain injuries carry risks of further injury, injury-related complications, and poor outcomes which are exacerbated if they are inappropriately managed in the ED. This post will cover some of the most common and important injuries, but is not comprehensive. Injuries discussed are shown in Image 1.
APPROACH TO ANKLE INJURIES
Presentation and Mechanism
Ankle injuries are most commonly caused by abrupt twisting of the ankle. Ankle sprains are most commonly caused by ankle inversion. Ankle fractures may present similarly to an ankle sprain, but are also seen in higher mechanisms of trauma, including MVCs, falls from height, penetrating wounds including GSWs, or other types of direct force to the ankle. Unstable injuries may be obvious at time of presentation, with the patient not being able to bear any weight.
Certain injuries are classically associated with certain mechanisms (e.g., traumatic axial loading with calcaneal fractures, pilons, and vertebral compression fractures) [5]. While knowing the mechanism can provide clues to potential injuries or increase your index of suspicion for certain injuries, mechanisms of injuries can be variable. Respect, but do not rely upon, the mechanism.
Exam
The exam (along with the history) is critical for proper diagnostic evaluation. Use your exam to guide your initial management as well as your imaging decisions and differential diagnosis.
Any significant bleeding should first be controlled in the setting of an open injury
Neurovascular assessment (perfusion, pulses, sensory function, motor function) should be prioritized, regardless of acuity. Abnormal neurovascular findings suggest injury to nearby structures (nerves and blood vessels) from dislocations, bony trauma, or increased compartment pressures.
Gross deformities often suggest fracture or dislocation [Image 2]. Obvious tendon or muscular deformity may be seen with Achilles tendon rupture [Image 3].
Skin tenting or other overlying skin changes are often indicative of impending open fracture or risk of skin necrosis. Significant swelling over a fracture may produce bullae known as “fracture blisters” [Image 4]
Palpate all bones and joints. In general, consider imaging of joints adjacent to an area of bony tenderness and imaging of bones adjacent to areas of joint tenderness.
Range all joints. If active ROM is impaired, perform passive ROM. Impaired ROM can be indicative of dislocation, ligamentous injury, or intra-articular pathology.
Certain provocative tests or inability to bear weight can be clues to instability. If instability is suspected or apparent, avoid having the patient bear weight.
In the setting of a more diffuse traumatic injury, always examine all other bones and joints even if the patient is only complaining of pain at the ankle (their ankle injury may be a distracting injury).
Consider examination and diagnostic evaluation for any injuries that are likely to co-occur (e.g., pilons with fibular fractures, bilateral calcaneal fractures, and vertebral compression fractures [6]).



Appropriate imaging
The vast majority of ankle injuries require at least basic radiographs for proper evaluation. Obtain at least 3 views when possible. While the Ottawa Ankle Rules [7] are often referenced and tested on exams, these criteria can miss significant injuries. You should consider full-length tib/fib films in all ankle injuries to rule out a more proximal fracture including a Maisonneuve fracture. Stress films are useful in assessing potential instability by assessing for any widening of the ankle mortise or syndesmosis. Some fractures are often difficult to see on XRs, so consider CT if your index of suspicion is high. Certain injuries require CTs for further characterization or surgical planning. MRI can be used in place of CT. Point-of-care ultrasound (POCUS) can evaluate for Achilles tendon rupture with a high sensitivity (96-100%) and specificity (83-100%) [8,9].
Management
Immediate management:
Control significant bleeding (e.g., direct pressure, tourniquet)
Address any impairments in neurovascular status (e.g., role of consulting services, emergent closed reduction, need for vascular imaging).
In the ED:
Pain control, including consideration for nerve blocks in certain injuries
Wound management (irrigation and debridement, possible closure, consideration of Abx, tetanus immunization)
Closed reduction and/or splinting (make sure to obtain repeat XRs after)
Determine if injury is stable vs. unstable (inherent to injury or as evidenced on stress films or advanced imaging)
Determine if injury is operative vs. non-operative
Determine if Orthopedics (or other specialist) consultation is needed
Unstable or surgical injury (or if this is suspected)
Uncertainty in diagnosis
Uncertainty in management (e.g., weight-bearing status, operative vs. non-operative)
If necessary/helpful to ensure adequate follow-up
At time of discharge:
Counsel on expected course of injury, supportive care (e.g., RICE), and symptomatic management (e.g., NSAIDs, Tylenol, opioid pain medication)
Counsel on ER return precautions, complications that are more likely in certain injuries (e.g., DVT, compartment syndrome), and consider prophylactic measures as appropriate
Brace, other cast, walking boot, immobilizer, etc.
Crutches and crutch training
Give clear instructions on weight-bearing status and use of any braces or walking boots given
Ensure there is a clear follow-up plan and provide any necessary referrals
Who they should see (e.g., primary care physician, Orthopedics, other specialist)
Whether they need to be seen definitely or only if needed, and when
Confirm correct patient contact information in EMR
Open fractures and injuries
Wounds that are not open fractures should receive irrigation and debridement, closure (if indicated), tetanus vaccination, consideration of antibiotics, and wound care instructions. Orthopedics should be consulted for any wounds near joints with concern of extension into the joint (i.e., traumatic arthrotomy), with a lower threshold to consult if the joint is non-native.
Open fractures and dislocations are generally managed with bleeding control, close assessment of neurovascular status, antibiotics with routine gram-positive coverage (Ancef; clindamycin if penicillin allergy), tetanus vaccination, and early irrigation and debridement in the ER with low pressure normal saline [10]. Open fractures can be categorized according to the Gustilo-Anderson classification system [11], though this has been critiqued for poor interrater reliability. Smaller wounds may not require antibiotics, but if in doubt, one dose of Ancef in the ED is unlikely to cause significant harm. Larger wounds (Gustilo-Anderson Type III) should also receive gram-negative microbial coverage. Wounds with potential soil or fecal contamination should receive high-dose penicillin [10]. The management of open fractures is further discussed in these TamingTheSRU posts:
Table 1a Common Ankle Injuries and their management considerations
Table 1B Common Ankle Injuries and their management considerations
References
Bergh C, Wennergren D, Möller M, Brisby H. Fracture incidence in adults in relation to age and gender: A study of 27,169 fractures in the Swedish Fracture Register in a well-defined catchment area. PLoS ONE. 2020.15(12): e0244291. doi.org/10.1371/journal.pone.0244291
Rosenbaum AJ et al. Musculoskeletal health literacy in patients with foot and ankle injuries: A cross-sectional survey of comprehension. Foot & Ankle Specialist. 2016. 9(1):31-36. doi: 10.1177/1938640015593078
Weiss AJ, Jiang J. Most frequent reasons for emergency department visits, 2018. Agency for Healthcare Research and Quality. Statistical brief #286. 2021. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb286-ED-Frequent-Conditions-2018.pdf. Accessed March 5, 2023.
Belatti DA, Phisitkul P. Economic burden of foot and ankle surgery in the US Medicare population. Foot & Ankle Int. 2014,35(4):334-340. doi: 10.1177/1071100713519777
Forsthoefel C. Calcaneus fractures. [Updated 2022 Nov 23]. In: OrthoBullets [Internet]. Available from: https://www.orthobullets.com/trauma/1051/calcaneus-fractures
Fares A, Szatkowski J. Tibial plafond fractures. [Updated 2023 Apr 22]. In: OrthoBullets [Internet]. Available from: https://www.orthobullets.com/trauma/1046/tibial-plafond-fractures
Pires R, Pereira A, Abreu-E-Silva G, Labronici P, Figueiredo L, Godoy-Santos A, Kfuri M. Ottawa ankle rules and subjective surgeon perception to evaluate radiograph necessity following foot and ankle sprain. Ann Med Health Sci Res. 2014 May;4(3):432-5. doi: 10.4103/2141-9248.133473. PMID: 24971221; PMCID: PMC4071746.
Hartgerink P, Fessell DP, Jacobson JA, van Holsbeeck MT. Full versus partial-thickness Achilles tendon tears: sonographic accuracy and characterization in 26 cases with surgical correlation. Radiology. 2001;220:406-12.
Paavola M, Paakkala T, Kannus P, Jarvinen M. Ultrasonography in the differential diagnosis of Achilles tendon injuries and related disorders. A comparison between pre-operative ultrasonography and surgical findings. Acta Radiol. 1998;39(6):612-9.
Garner MR, Sethuraman SA, Schade MA, Boateng H. Antibiotic Prophylaxis in Open Fractures: Evidence, Evolving Issues, and Recommendations. J Am Acad Orthop Surg. 2020 Apr 15;28(8):309-315. doi: 10.5435/JAAOS-D-18-00193. PMID: 31851021.
Kim PH, Leopold SS. Gustilo-Anderson Classification. Clin Orthop Relat Res. 2012 Nov; 470(11):3270-3274. doi: 10.1007/s11999-012-2376-6 PMID: 22569719
Macknet D, Weatherford B. Ankle sprain. [Updated 2023 Feb 26]. In: OrthoBullets. Available from: https://www.orthobullets.com/foot-and-ankle/7028/ankle-sprain
Karadesh M. High ankle sprain & syndesmosis injury. [Updated 2022 Apr 7]. In: OrthoBullets. Available from: https://www.orthobullets.com/foot-and-ankle/7029/high-ankle-sprain-and-syndesmosis-injury
Wong PK, Hanna TN, Shuaib W, Sanders SM, Khosa F. What's in a name? Lower extremity fracture eponyms (Part 2). Int J Emerg Med. 2015 Dec;8(1):76. doi: 10.1186/s12245-015-0076-1. Epub 2015 Jul 25. PMID: 26223985; PMCID: PMC4512960.
Gomez A, Cadogan M. Danis-Weber classification. [Updated 2022 Mar 16]. In: LITFL - Life in the Fast Lane [Internet]. Available from: https://litfl.com/danis-weber-classification/
Taylor BC, Tarazona D. Ankle fractures. [Updated 2023 Apr 11]. In: OrthoBullets [Internet]. Available from: https://www.orthobullets.com/trauma/1047/ankle-fractures
Koujan K, Saber AY. Bimalleolar Ankle Fractures. [Updated 2023 Feb 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562254/
Authorship
Written by: Isabel Lott, MD, PGY-1, University of Cincinnati Department of Emergency Medicine
Peer Review by Bret Betz, MD, Associate Professor, University of Cincinnati Department of Emergency Medicine
Editing and Posting by Jeffery Hill, MD MEd, Associate Professor, University of Cincinnati Department of Emergency Medicine
Cite As
Lott, I., Betz, B., Hill, J. (May 22, 2023) Twisting and Turning - Ankle Injuries in the ED. TamingtheSRU. https://www.tamingthesru.com/blog/diagnostics/ankle-injuries-in-the-ed