Blunt Thoracic Trauma in the Emergency Department
/Blunt thoracic trauma represents a substantial proportion of trauma-related presentations to the emergency department, ranging from minor chest wall injuries to life-threatening conditions. This article outlines a practical approach to initial assessment using the ABCs, highlights the role of imaging (CXR and CT), and reviews management of common thoracic injuries—rib fractures, flail chest, sternal fractures, pulmonary contusions, pneumothorax, and hemothorax. This post does not address vascular, cardiac injuries, or major airway injuries.
Epidemiology and Mechanisms of Injury
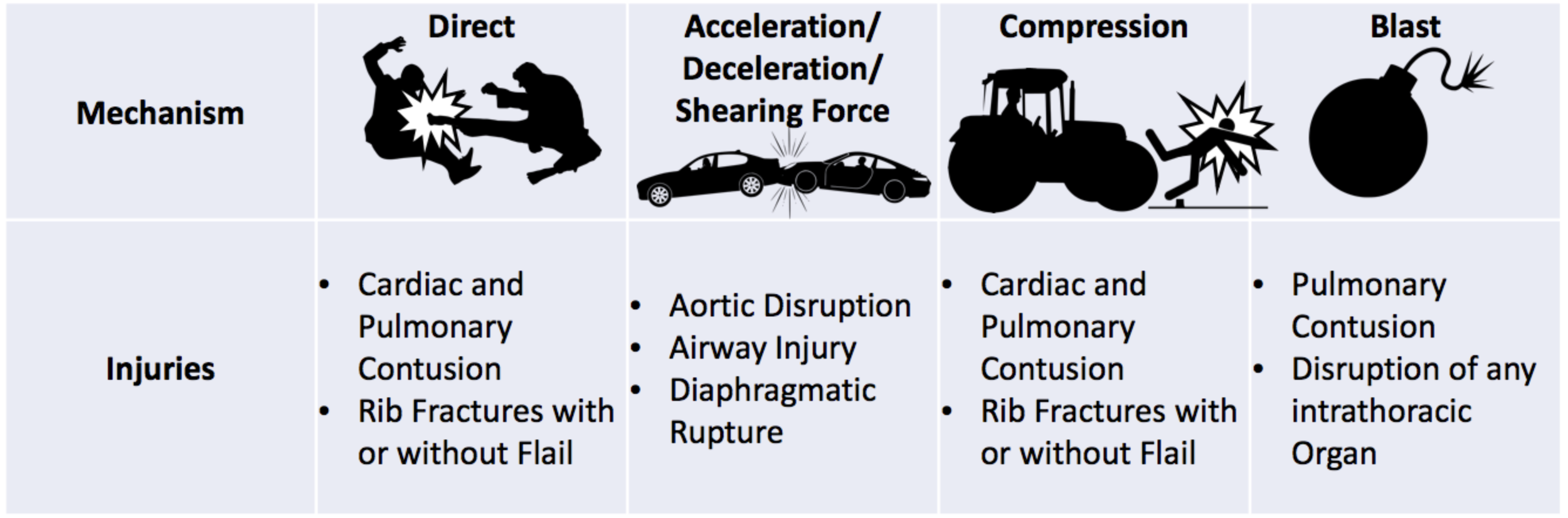
Understanding the mechanism of blunt chest trauma is essential for rapid diagnosis and appropriate management, as different mechanisms are associated with characteristic injury patterns and can independently influence patient outcomes. The severity of injury depends on factors such as the force, duration, and direction of the impact, as well as the effects of acceleration-deceleration or compression on thoracic structures.
Blunt thoracic trauma generally occurs through four primary mechanisms:
Direct impact to the chest, such as from assaults or collisions with objects.
Thoracic compression, which can result from crush injuries, occupational accidents, or falls from height.
Acceleration-deceleration forces, commonly seen in motor vehicle collisions (MVCs).
Blast injuries, typically associated with explosions or high-energy events.
Among these, motor vehicle collisions and falls from height are the most frequently encountered causes of blunt chest trauma in the emergency department.
But which patients should I be worried about?
Other than considering primary patient factors such as age and co-morbidities, it is important to be able to identify mechanisms that are high risk, which would necessitate rapid evaluation and thorough imaging.
Common high-risk mechanisms include but are not limited to:
MVCs at speeds exceeding 30 mph, particularly those involving frontal or lateral impact
MVCs with vehicle ejection, rollovers, and direct chest trauma (steering wheel impact)
Vehicle ejection is associated with the highest Injury Severity Score, followed by rollover and side-impact collisions.
Falls from heights greater than 25 feet, with mortality rates increasing as the height of the fall increases. For example, falls exceeding 48 feet have mortality rates over 50 and falls from heights > 61 feet are almost always fatal.
These mechanisms as well as several others not listed are often predictive of increased injury severity, prolonged hospital stays, and higher mortality rates. Identifying patients who have sustained high-mechanism injuries is essential for guiding triage decisions, selecting appropriate imaging, and determining the necessary level of care.
Initial Evaluation and Resuscitation
Management of blunt thoracic trauma begins with a structured, algorithmic approach that prioritizes early identification of life-threatening injuries. Other than mechanism of injury as described above, the initial branch point in trauma evaluation hinges on two critical elements: ABCs and vital sign.
Knowing your ABC(DE)s
The ABCDE model remains the cornerstone of trauma assessment and is often referred to as the “primary survey”. ABCDE stands for:
Airway: Ensure patency and evaluate for potential obstruction.
Breathing: Assess for asymmetric chest rise, decreased or absent breath sounds, tracheal deviation, and subcutaneous emphysema.
Circulation: Monitor vital signs, evaluate cardiac rhythm, check for jugular venous distention, and identify signs of shock.
Disability/Exposure: Assess neurologic status and perform full exposure to identify occult injuries.
During the ABC’s, the six most cited life-threatening injuries are often identified, which include airway obstruction, tension pneumothorax, open pneumothorax, massive hemothorax, flail chest, and pericardial tamponade. These critical threats MUST be addressed first before shifting attention toward the evaluation, imaging, and management of the less severe injuries.
In patients with unstable vital signs or high-risk mechanisms, this primary survey should also include point-of-care eFAST ultrasound. Its integration into the primary survey enhances diagnostic precision and guides immediate interventions for life-threatening injuries such as pericardial tamponade, pneumothorax, or presence of blood in the abdomen (indicating a possible need for the operating room).
The Vitals Don’t Lie (except sometimes they do)
Hemodynamic stability must be assessed immediately and reassessed frequently—while this is ideally initiated in the prehospital setting, subtle presentations of hemorrhagic or obstructive shock can lead to mis-triage as “minor trauma.”
Even when traditional vital signs appear “normal,” clinicians must remain alert to subtle indicators of shock.
The Shock Index (SI)—calculated as heart rate divided by systolic blood pressure—is a valuable early marker:
Normal: SI < 0.5
Mild shock: SI 0.5–0.7
Moderate shock: SI 0.7–0.9
Severe shock: SI > 0.9
Beyond objective numbers, skin signs and mental status often provide the earliest clues. Pale, cool skin reflects peripheral vasoconstriction as the body shunts blood to vital organs. Anxiety or restlessness, even in the absence of overt hypotension or tachycardia, may signal cerebral hypoperfusion. A patient who is pale and anxious—with “normal” vitals—should never be dismissed; they may be the first harbingers of evolving shock.
Diagnostic Imaging – does everyone need a CT? (hint: no)
Imaging of the chest is a key part of evaluating patients who sustain blunt thoracic trauma. Chest X-ray is typically the first-line study because it is widely available and quick to perform. However, chest x-rays are not very sensitive and can miss subtle injuries.
Guidelines have been developed to help determine which patients truly need further imaging with chest CT, to both avoid missing injuries but also to avoid excessive use of CTs that can lead to increases in radiation exposure and healthcare costs.
Two validated sets of criteria, NEXUS Chest CT-Major and NEXUS Chest CT-All, can guide emergency medicine clinicians in deciding whether a CT scan is necessary for hemodynamically stable patients. These rules rely in part on physical exam findings, such as chest wall tenderness, so they are not suitable for patients who are unconscious or intubated.
NEXUS Chest CT Criteria:
CT-Major: abnormal CXR, distracting injury, chest wall tenderness, sternal tenderness, thoracic spine tenderness, or scapular tenderness.
CT-All: includes all CT-Major criteria + the presence of a rapid deceleration mechanism, such as a high-speed car crash or a fall from a significant height.
Approach to Imaging:
Initial Assessment: Stable patients are first evaluated using the NEXUS Chest criteria, which also consider factors like age over 60, rapid deceleration, chest pain, intoxication, distracting injury, and altered mental status. If none of these are present, it is generally safe to skip both CXR and CT.
After CXR (if you get one):
A normal CXR with low clinical suspicion usually means no CT is needed.
If suspicion remains high, the NEXUS CT criteria are applied:
One criterion present: CT can be considered.
Two or more criteria: CT is recommended.
Abnormal CXR: If they are visualized severe injuries, further imaging may be needed. If there is uncertainty or concern for additional injuries missed on CXR, CT should be obtained.
Using these stepwise approaches has been shown to decrease the number of chest CTs performed by about 20% without increasing patient risk to missed injuries. Following these guidelines helps emergency medicine physicians use imaging efficiently, minimize unnecessary radiation exposure, and reduce costs, while still identifying significant thoracic injuries.
Chest Wall Injuries
Once life-threatening injuries have been ruled out and the patient is hemodynamically stable, attention shifts to the more common—but still consequential—chest wall injuries. Rib fractures, flail chest, and sternal fractures make up the bulk of the chest wall injury presentations. While they may not demand immediate intervention, they carry significant morbidity and require thoughtful management to prevent complications like hypoventilation, atelectasis, pneumonia, and prolonged hospitalization.
1) Rib Fractures
Rib fractures are the most frequently encountered injury in blunt thoracic trauma. The majority of rib fractures are usually managed conservatively with pain control and observation. Historical approaches such as chest binding or casting are no longer recommended due to their restrictive effects on ventilation and the associated increased risk of hypoxemia and/or pneumonia.
But which rib fractures (fxs) are really bad?
Pretty much all of them.
1st-2nd rib fxs can have —> associated subclavian vessel, brachial plexus, or blunt aortic arch injury
4th – 10th rib fxs can have —> associated pulmonary contusions, lacerations, pneumothoraces
3 or more rib fxs should —> increase your concern for high-risk mechanism and underlying associated pulmonary complication
7 or more rib fxs can have —> associated mortality of up to 30%
Elderly patients with 3 or more rib fractures demonstrate approximately double the risk of both mortality and pneumonia compared with younger adults and these patients should be stronger considered for a stepdown or ICU admission.
So who can we send home if all rib fxs are bad?
Outpatient treatment decisions should be individualized, taking into account the patient’s overall clinical status and ability to attend outpatient follow up. Patients can be considered for outpatient management if they meet the following criteria:
3 or less rib fxs with NO associated other injuries
ability to pull > 15 ml / kg on incentive spirometry when pain is controlled
age < 65, oxygen saturation > 92% on room air
Any patients not meeting these criteria require close respiratory monitoring, particularly if they have three or more rib fractures, and if they are displaced, as these patients are at significantly increased risk for pulmonary complications such as including pulmonary contusion or delayed pneumonia due to impaired ventilation.
Management (whether outpatient or inpatient) focuses on multimodal pain control, including acetaminophen, ibuprofen, methocarbamol, and a transition from IV to oral narcotics, along with pulmonary “toilet”. This includes frequent use of incentive spirometer, diuretics when appropriate, and sometimes advanced chest physiotherapy. In older admitted adults, epidural analgesia is recommended to optimize pulmonary function and improve clinical outcomes.
2) Flail Chest
Flail chest is a severe form of chest wall injury that occurs when three or more contiguous ribs are fractured in at least two locations, resulting in a segment of the chest wall that moves independently from the remainder of the thorax. This paradoxical motion impairs effective ventilation, reduces tidal volume, and can significantly compromise oxygenation.
The condition is frequently associated with high-energy mechanisms such as motor vehicle collisions and falls from height. Importantly, flail chest is rarely an isolated injury; it is often accompanied by pulmonary contusions, hemothorax, or pneumothorax, which contribute substantially to morbidity and mortality. The combination of chest wall instability and underlying pulmonary injury can rapidly progress to respiratory failure if not promptly addressed.
Initial management in the emergency department emphasizes aggressive analgesia, supplemental oxygen, and pulmonary hygiene to optimize ventilation. Patients with significant respiratory compromise may require non-invasive ventilation or endotracheal intubation with mechanical ventilation.
In select cases, surgical stabilization of rib fractures can improve outcomes by restoring chest wall mechanics and reducing the duration of mechanical ventilation. Early consultation with trauma surgery is recommended when surgical fixation is considered.
Although mortality rates have decreased with advances in critical care and pain management, flail chest remains associated with significant complications, particularly pneumonia and prolonged hospital stay. Older age and the presence of multiple associated injuries are important predictors of worse outcomes.
3) Sternal Fracture
Sternal fractures represent a relatively small proportion of chest wall injuries in blunt thoracic trauma but remain clinically significant due to their association with high-energy mechanisms. Motor vehicle collisions are the most common cause, accounting for approximately 84% of cases, often related to seatbelt or steering wheel impact. Isolated sternal fractures are uncommon, and most occur alongside additional injuries such as rib fractures, pulmonary contusions, or other thoracic trauma.
How to Diagnose
Clinical exams —> due to the very superficial nature of the sternum, if a patient does not have direct bruising to the sternum or tenderness over the sternum, it is very unlikely that they have a sternal fracture.
Standard chest radiographs —> limited sensitivity, unlikely to pick up a sternal fracture
Chest CT —> evidence from the NEXUS Chest and NEXUS Chest CT studies demonstrated that 94% of sternal fractures were identified only on CT imaging
I found a sternal fracture… now what?
Obtain an EKG and troponin!
The anatomical location of the sternum places patients at increased risk for blunt cardiac injury. A study conducted at a Level I trauma center demonstrated that elevated high sensitivity troponin levels (≥40 ng/L) combined with ECG abnormalities were more predictive of blunt cardiac injury than the presence of sternal fracture alone.
Who can be sent home?
Patients with isolated sternal fractures who demonstrate normal ECG and high-sensitivity troponin levels, stable vital signs, and adequate pain control with analgesics are appropriate candidates for outpatient management.
Inpatient care should be considered for those with abnormal ECG findings, persistent troponin elevation, or evidence of multisystem trauma. Elevated high sensitivity troponin levels should be trended until they plateau.
Pulmonary Injuries
After identifying chest wall trauma—rib fractures, flail segments, sternal injuries—the next step is to assess for associated pulmonary injuries. Blunt force can transmit energy inward, resulting in parenchymal damage such as pulmonary contusions or air leaks like pneumothorax. These injuries may not be immediately apparent but can significantly impact respiratory function and clinical trajectory.
1) Pulmonary Contusion
Pulmonary contusion is a common consequence of blunt thoracic trauma, particularly in patients with multiple rib fractures or high-energy mechanisms such as motor vehicle collisions. Clinical signs may be delayed, developing over hours to days, and tachypnea, difficulty breathing, and hypoxemia are common symptoms. Contusions occur in roughly 30–75% of patients with substantial chest wall injury and are a key predictor of morbidity and mortality.
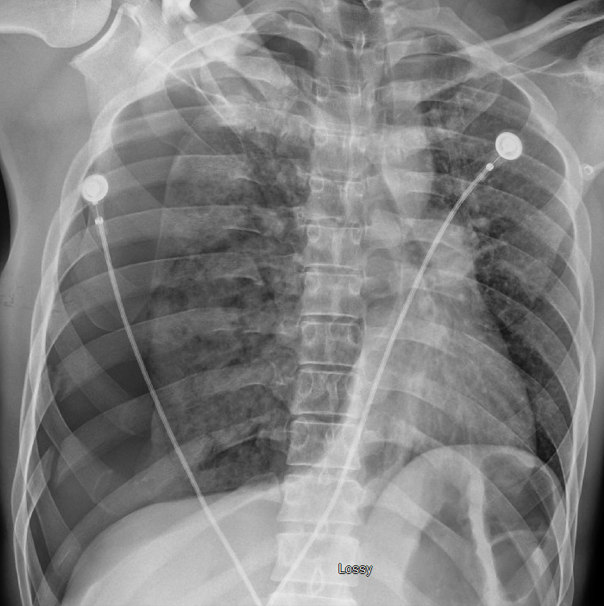
Radiographically, pulmonary contusions may be occult on initial chest X-ray, as findings often evolve over time and may not fully manifest until 24 to 72 hours after injury. CT imaging provides greater sensitivity and more accurately defines the extent of injury.
Management is supportive: supplemental oxygen, effective pain control, and pulmonary hygiene (e.g., chest physiotherapy) are foundational. Non-invasive ventilation is preferred when feasible, as intubation is typically reserved for more critically ill patients who require additional ventilatory support. Severe cases may progress to ARDS and require mechanical ventilation, with associated increases in ICU length of stay and pulmonary complications.
Saline fluid resuscitation should be judicious—overhydration may worsen pulmonary edema. In polytrauma patients requiring volume, intermittent use of diuretics may help mitigate overload and preserve oxygenation.
2) Pneumothorax
Pneumothorax occurs in approximately one-third of patients with blunt thoracic trauma and may range from clinically silent to life-threatening, depending on its size and the degree of cardiorespiratory compromise. Pneumothorax results from the accumulation of air within the pleural space, leading to loss of negative intrapleural pressure. This disrupts normal lung mechanics, causing partial or complete lung collapse. In blunt trauma, this may be due to alveolar rupture from rapid deceleration, rib fractures puncturing lung tissue, or direct compression. As the lung collapses, ventilation-perfusion mismatch ensues, reducing oxygenation. In cases of tension pneumothorax, progressive air accumulation exerts pressure on the mediastinum, compressing the contralateral lung and great vessels, which can result in shock and rapid cardiovascular collapse if not promptly treated.
Clinical Presentation
Simple pneumothorax often presents with mild dyspnea, pleuritic chest pain, and decreased breath sounds on the affected side. In some cases, it may be asymptomatic and incidentally found on screening imaging (i.e. standard trauma chest x-ray).
Tension pneumothorax is a medical emergency and typically presents with hypotension, tachycardia, severe respiratory distress, jugular venous distension, and tracheal deviation away from the affected side. If unrecognized, it can rapidly progress to cardiac arrest.
Diagnosis
Chest X-ray: Can diagnose SOME pneumothoraces. An upright chest radiograph is more specific than supine imaging for the detection of pneumothorax; however, in the trauma setting, patients are frequently imaged in the supine position, which significantly reduces diagnostic sensitivity.
eFAST: Bedside ultrasound has therefore demonstrated better sensitivity in trauma patients for identifying pneumothorax.
CT Scan: CT remains the most sensitive imaging modality for detecting pneumothorax, including small or occult collections of air not visible on plain radiographs. However, its use may be limited in hemodynamically unstable patients who are not suitable for transport to the scanner.
Clinical suspicion: the diagnosis of a tension pneumothorax is typically clinical and based on patient’s vitals and physical exam, and treatment should not be delayed for imaging when this is suspected.
Management
Treatment is guided by the patient’s hemodynamic status and the size of the pneumothorax:
Small, stable pneumothorax —> may be managed conservatively with observation and supplemental oxygen. If repeat imaging after 3 to 4 hours is stable, patients may be discharged with outpatient follow-up.
Larger or symptomatic pneumothorax —> typically requires chest tube placement + admission for ongoing monitoring.
In unstable patients with suspected tension pneumothorax, immediate needle decompression is indicated, typically followed by chest tube insertion.
A great more in-depth post on pneumothorax, including both diagnostic studies and management, can be found here.
3) Hemothorax
Hemothorax results from accumulation of blood in the pleural space, most often due to rib fractures lacerating intra-thoracic vasculature or injury to lung parenchyma. Clinical signs include respiratory insufficiency, decreased breath sounds, and in severe cases, hypotension. These are usually identified on x-ray imaging or CT but can also be seen on eFAST exam.
A massive hemothorax is defined as the accumulation of more than 1,500 mL of blood within the pleural space, or ongoing bleeding of greater than 200 mL per hour for three consecutive hours, both of which are indications for surgical intervention. While chest radiography can provide a rough estimate of pleural fluid volume, the most accurate assessment of hemothorax is achieved following placement of a chest tube.
Almost all traumatic hemothoraces should be drained, regardless of size, to minimize the risk of retained hemothorax and subsequent infectious complications such as empyema. Initial management typically involves tube thoracostomy, accompanied by prophylactic antibiotic administration to reduce infection risk.
Summary
Blunt thoracic trauma encompasses a wide spectrum of injuries, from isolated rib fractures to life-threatening vascular or cardiac injuries. A structured approach, beginning with the ABCDE assessment and supplemented by appropriate imaging, is essential for rapid diagnosis and effective management. Rib fractures and pulmonary contusions are the most common injuries, but early recognition of critical conditions such as tension pneumothorax, massive hemothorax, cardiac tamponade, and aortic injury is crucial for optimizing patient outcomes. Management in the emergency department involves a systematic evaluation of the patient’s status, the use of appropriate diagnostic tools, and the maintenance of adequate respiratory function, with pain control playing a central role in supporting ventilation and overall recovery.
POST BY Jasmine Ware MD
Dr. Ware is a PGY-1 resident at the University of Cincinnati Emergency Medicine Residency.
EDITING BY ANITA GOEL, MD and Dr Timothy Pritts, MD
Dr. Goel is an Associate Professor at the University of Cincinnati, a graduate of the UC EM Class of 2018, and an assistant editor of Taming the SRU.
Dr Pritts is a Professor of Surgery at the University of Cincinnati. He is fellowship trained in trauma and surgical critical care, and actively involved in surgical resident education and research.
References
Dogrul BN, Kiliccalan I, Asci ES, Peker SC. Blunt trauma related chest wall and pulmonary injuries: An overview. Chin J Traumatol. 2020 Jun;23(3):125-138. doi: 10.1016/j.cjtee.2020.04.003. Epub 2020 Apr 20. PMID: 32417043; PMCID: PMC7296362.
Clancy K, Velopulos C, Bilaniuk JW, Collier B, Crowley W, Kurek S, Lui F, Nayduch D, Sangosanya A, Tucker B, Haut ER; Eastern Association for the Surgery of Trauma. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012 Nov;73(5 Suppl 4):S301-6. doi: 10.1097/TA.0b013e318270193a. PMID: 23114485.
Rodriguez RM, Hendey GW, Mower WR. Selective chest imaging for blunt trauma patients: The national emergency X-ray utilization studies (NEXUS-chest algorithm). Am J Emerg Med. 2017 Jan;35(1):164-170. doi: 10.1016/j.ajem.2016.10.066. Epub 2016 Oct 29. PMID: 27838036; PMCID: PMC5177494.
Moussavi N, Talari H, Abedzadeh-Kalahroudi M, Khalili N, Eqtesadi R, Sehat M, Azadchehr MJ, Davoodabadi A. Implementation of an algorithm for chest imaging in blunt trauma decreases use of CT-scan: Resource management in a middle-income country. Injury. 2021 Feb;52(2):219-224. doi: 10.1016/j.injury.2020.12.040. Epub 2021 Jan 6. PMID: 33441251.
Wolf S, Camacho M. Blunt Thoracic Trauma. In: Swadron S, Nordt S, Mattu A, and Johnson W, eds. CorePendium. 5th ed. Burbank, CA: CorePendium, LLC. https://www.emrap.org/corependium/chapter/recwp71YmuzjjxT8P/Blunt-Thoracic-Trauma#h.n9bih0yq5ezm. Updated October 30, 2024. Accessed October 3, 2025.
Perez MR, Rodriguez RM, Baumann BM, Langdorf MI, Anglin D, Bradley RN, Medak AJ, Mower WR, Hendey GW, Nishijima DK, Raja AS. Sternal fracture in the age of pan-scan. Injury. 2015 Jul;46(7):1324-7. doi: 10.1016/j.injury.2015.03.015. Epub 2015 Mar 14. PMID: 25817167.
Simon B, Ebert J, Bokhari F, Capella J, Emhoff T, Hayward T 3rd, Rodriguez A, Smith L; Eastern Association for the Surgery of Trauma. Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012 Nov;73(5 Suppl 4):S351-61. doi: 10.1097/TA.0b013e31827019fd. PMID: 23114493.
Griffard J, Kodadek LM. Management of Blunt Chest Trauma. Surg Clin North Am. 2024 Apr;104(2):343-354. doi: 10.1016/j.suc.2023.09.007. Epub 2023 Oct 29. PMID: 38453306.
Dennis BM, Bellister SA, Guillamondegui OD. Thoracic Trauma. Surg Clin North Am. 2017 Oct;97(5):1047-1064. doi: 10.1016/j.suc.2017.06.009. PMID: 28958357.
Khandhar SJ, Johnson SB, Calhoon JH. Overview of thoracic trauma in the United States. Thorac Surg Clin. 2007 Feb;17(1):1-9. doi: 10.1016/j.thorsurg.2007.02.004. PMID: 17650692.
Zingg SW, Millar DA, Goodman MD, Pritts TA, Janowak CF. The Association Between Pulmonary Contusion Severity and Respiratory Failure. Respir Care. 2021 Nov;66(11):1665-1672. doi: 10.4187/respcare.09145. Epub 2021 Sep 28. PMID: 34584011.
Becker ER, Price AD, Whitrock JN, Smith M, Baucom MR, Makley AT, Goodman MD. Re-evaluating the Use of High Sensitivity Troponin to Diagnose Blunt Cardiac Injury. J Surg Res. 2024 Aug;300:150-156. doi: 10.1016/j.jss.2024.04.074. Epub 2024 May 29. PMID: 38815513.
Hussein B, Mercader D, Theophanous RG. Ultrasound-guided thoracic nerve blocks for emergency department patients with rib fractures: A review. J Emerg Med. 2025 Jan;68:1-14. doi: 10.1016/j.jemermed.2024.07.016. Epub 2024 Aug 14. PMID: 39809646
Nau C, Leiblein M, Verboket RD, Hörauf JA, Sturm R, Marzi I, Störmann P. Falls from Great Heights: Risk to Sustain Severe Thoracic and Pelvic Injuries Increases with Height of the Fall. J Clin Med. 2021 May 25;10(11):2307. doi: 10.3390/jcm10112307. PMID: 34070640; PMCID: PMC8199183.
Abu-Zidan FM, Eid HO. Factors affecting injury severity of vehicle occupants following road traffic collisions. Injury. 2015 Jan;46(1):136-41. doi: 10.1016/j.injury.2014.10.066. Epub 2014 Nov 6. PMID: 25467823.
Edgecombe L, Sigmon DF, Galuska MA, et al. Thoracic Trauma. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534843/
Benhamed A, Ndiaye A, Emond M, Lieutaud T, Boucher V, Gossiome A, Laumon B, Gadegbeku B, Tazarourte K. Road traffic accident-related thoracic trauma: Epidemiology, injury pattern, outcome, and impact on mortality-A multicenter observational study. PLoS One. 2022 May 6;17(5):e0268202. doi: 10.1371/journal.pone.0268202. PMID: 35522686; PMCID: PMC9075643.
Sutherland M. Pneumothorax. In: Swadron S, Nordt S, Mattu A, and Johnson W, eds. CorePendium. 5th ed. Burbank, CA: CorePendium, LLC. https://www.emrap.org/corependium/chapter/recqwx9YlVVlPl1mJ/Pneumothorax#h.a4ej7mhnmuoz. Updated July 11, 2025. Accessed October 13, 2025.
Carsetti, A., Antolini, R., Casarotta, E. et al. Shock index as predictor of massive transfusion and mortality in patients with trauma: a systematic review and meta-analysis.Crit Care 27, 85 (2023).
Kheirbek T, Martin TJ, Cao J, Hall BM, Lueckel S, Adams CA. Prehospital shock index outperforms hypotension alone in predicting significant injury in trauma patients. Trauma Surgery & Acute Care Open. 2021;6:e000712.