Mastering Minor Care: Bartholin Gland Abscess
/Introduction & Pathophysiology
Bartholin glands (aka the greater vestibular glands) are located on either side of the vagina introitus at the 4 o’clock and 8 o’clock positions. These glands secrete mucus through small ducts, which plays a role in vaginal lubrication [1]. When these glands or ducts become blocked, a Bartholin gland cyst or abscess can result. A Bartholin gland cyst is usually unilateral and asymptomatic but may cause pain or urinary irritation. Because they are often asymptomatic, Bartholin gland cysts are often incidentally found [2]. A Bartholin gland abscess occurs when this blockage results in infection and inflammation, causing significant pain and irritation.
PATIENT PRESENTATION & DIAGNOSIS
Symptoms:
Vulvar pain with sitting, walking, or sexual intercourse.
May report purulent drainage.
Physical exam:
Asymmetry with a protrusion on one side of the inferior aspect of the vulva.
Tender, erythematous Bartholin gland. Induration and fluctuance often present.
There may be areas of expressible purulent drainage [2].
work up in the emergency department
Bartholin gland cyst and abscess is a clinical diagnosis based on history and physical exam findings as stated above). In most cases laboratory work-up and abscess cultures are not indicated, with the following exceptions listed below:
Concern for sexually transmitted infection: Consider sending vaginal wet prep and antigen testing for N. gonorrhoeae, C. trachomatis [1].
Concern for sepsis/systemic infection: Consider sending CBC, lactate, blood cultures in patients who are ill-appearing, febrile, or have other vital sign abnormalities.
Recurrent disease: Consider sending a wound culture in patients with repeat presentations.
Concern for MRSA: Consider sending a wound culture in patients with risk factors for MRSA, including recent hospitalization/surgery, residence in long-term care facility, incarceration, military service, history of MRSA infection or close contact with another individual with a history of MRSA infection, hemodialysis, HIV, injection drug use, antibiotic use in the past 6 months, sharing needles/razors [4].
MANAGEMENT
Asymptomatic cysts do not require intervention. Bartholin gland abscesses that are spontaneously draining may be managed conservatively with sitz baths and analgesics (1), whereas non-draining abscesses will require an incision and drainage procedure as detailed below. Patients with repeat presentation should be referred to Gynecology to discuss a marsupialization procedure (3).
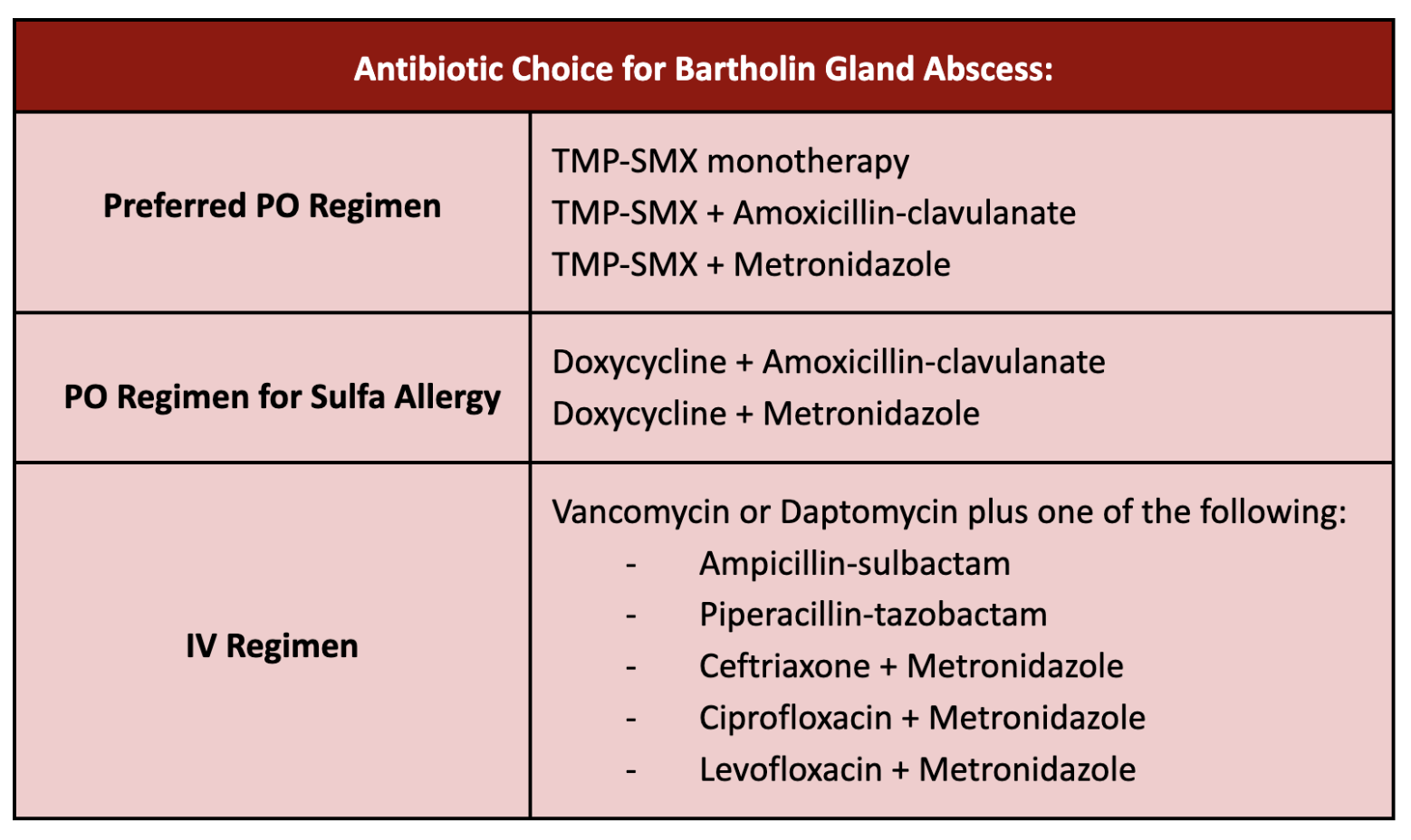
Antibiotics are not usually indicated, but shoud be considered for patients with the following risk factors:
Recurrent Bartholin abscess
Those with systemic symptoms including fever
Culture-positive MRSA (or risk factors for MRSA)
Extensive surrounding cellulitis
Immunocompromised patients
Antibiotics should cover gram-positive species (Staph and Strep) as well as gram-negative anaerobes. Admission for IV antibiotics should be considered in patients with systemic illness, inability to tolerate PO, or those who have failed an appropriate outpatient antibiotic regimen. IV antibiotic regimens should cover MRSA in addition to other gram-positives and gram-negative anaerobes (4). Acceptable antibiotic regimens are listed in the table above.
PROCEDURE
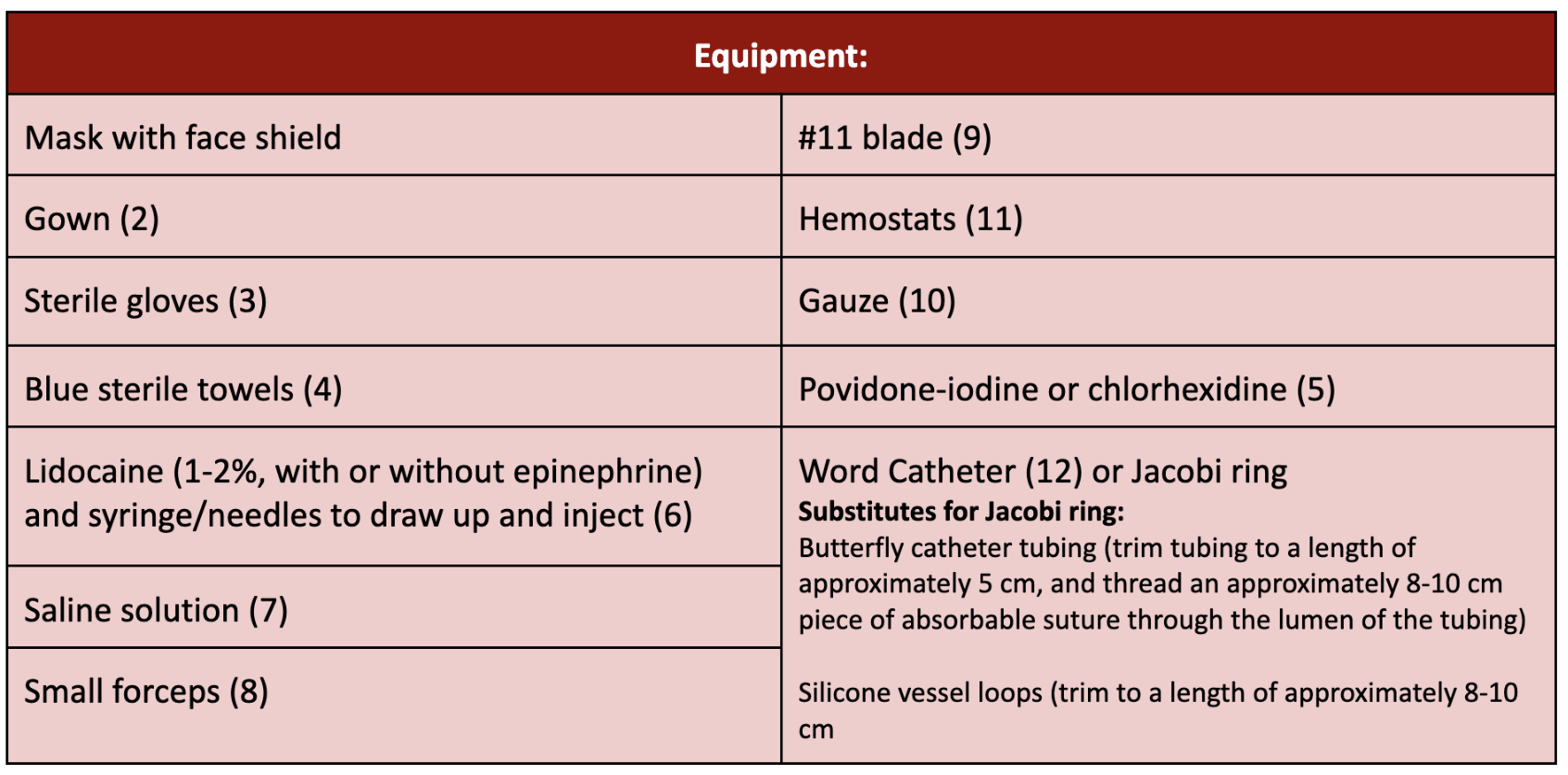
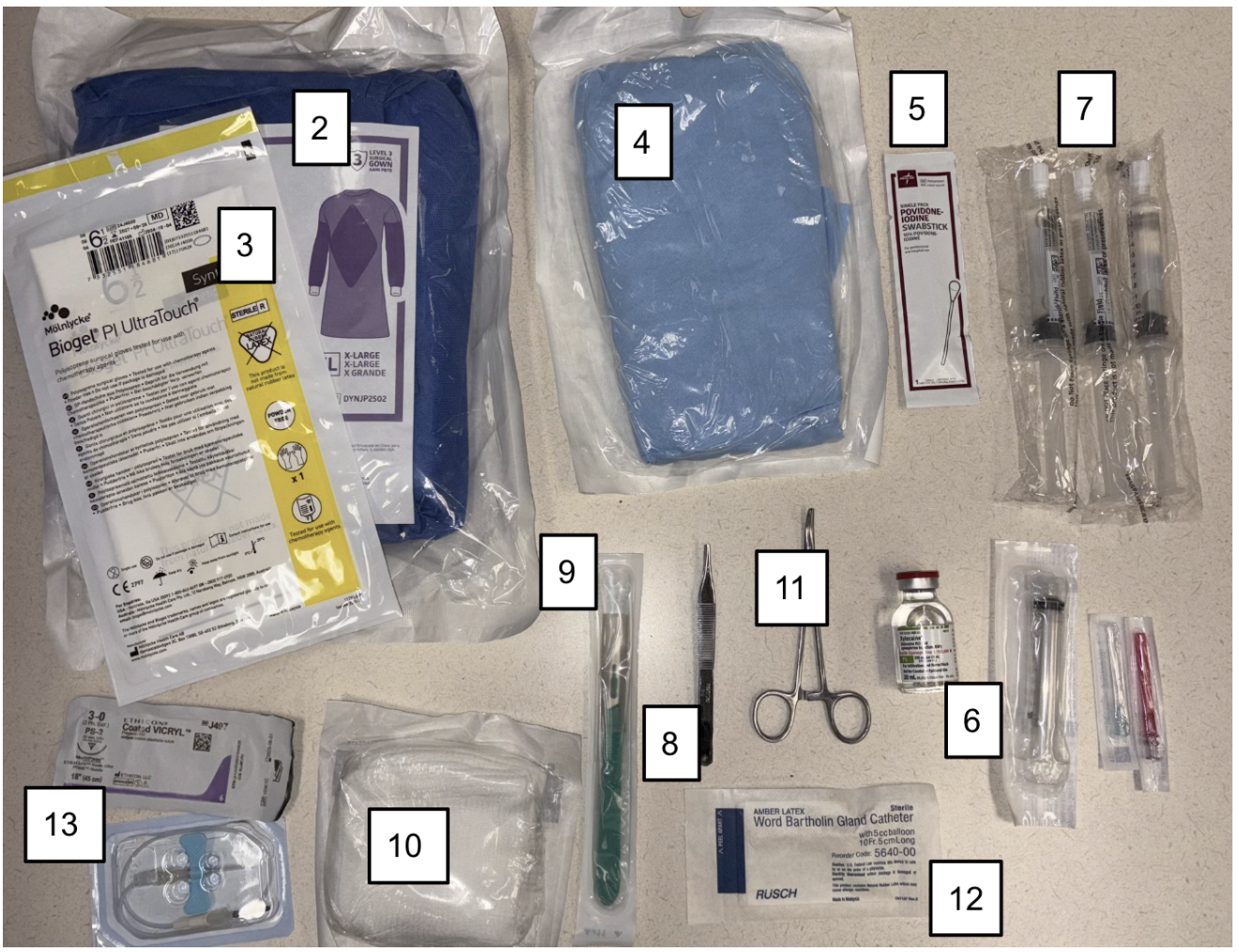
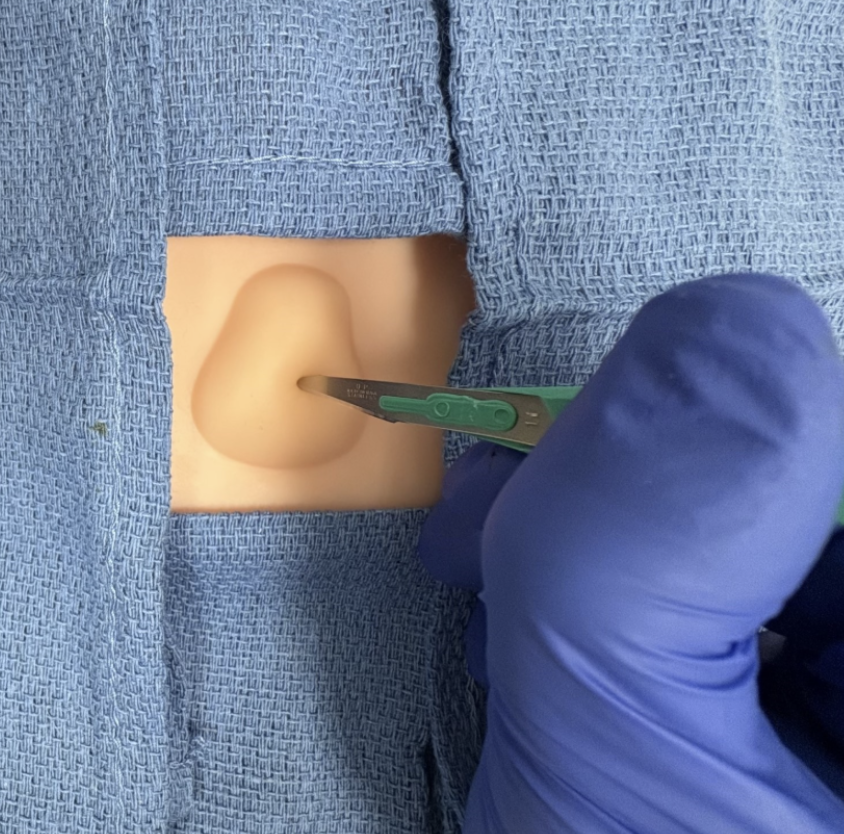
Consider administering oral or intravenous pain medications and/or anxiolysis prior to the procedure. Procedural or conscious sedation can also be considered in patients unlikely to tolerate the procedure otherwise, depending on policies and capabilities at your facility.
Clean area with povidone-iodine or chlorhexidine.
Create your sterile field with blue sterile towels and lay your equipment out in a sterile fashion.
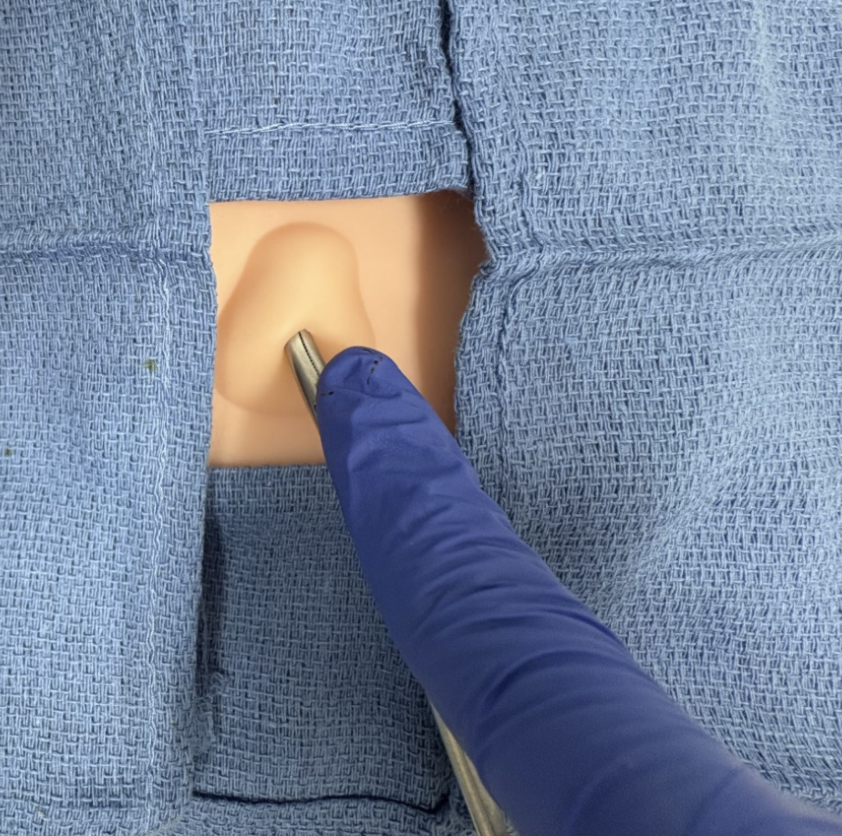
Anesthetize the area with lidocaine.
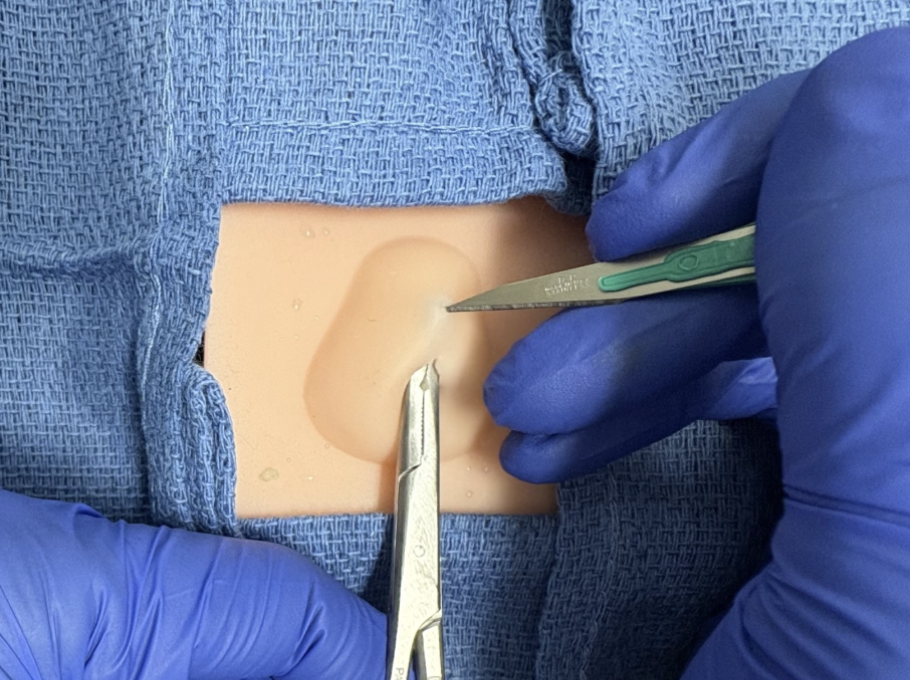
Make a small (3-5mm) vertical incision with the scalpel on the inner mucosal surface of the labia minora. The incision should be large enough to drain, but not so large that the Word catheter falls out.
Evacuate purulent discharge and collect culture if indicated (1). Use hemostats and saline solution as needed.
7. Insert Word catheter or Jacobi ring.
Word catheter:
7a. Insert the Word catheter with the tip inside the abscess cavity.
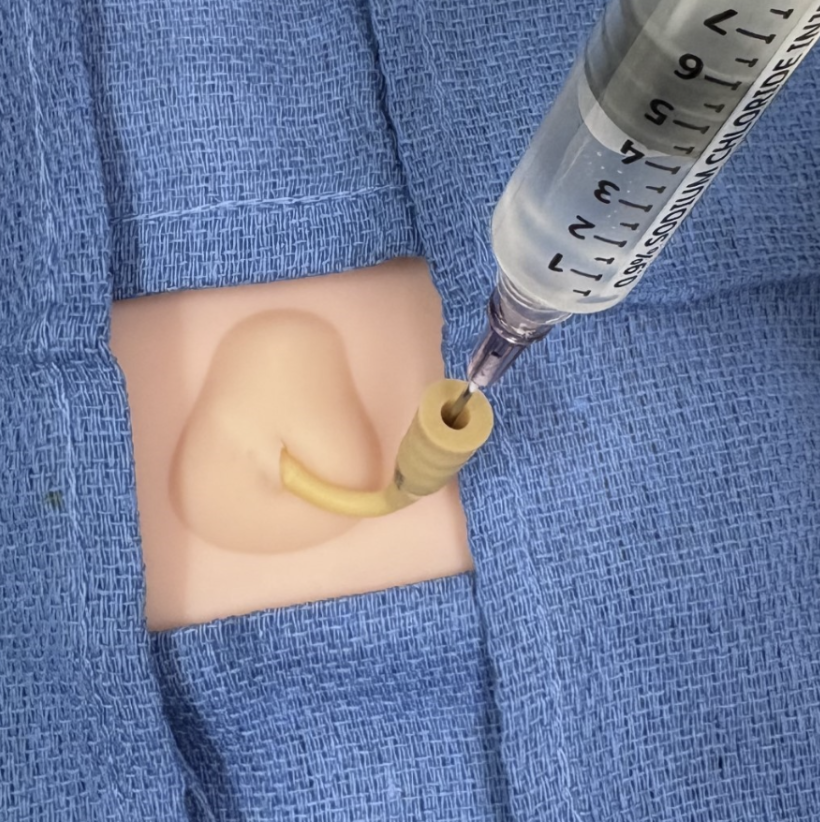
7b. Inflate balloon tip with ~3mL saline.
7c. The external portion of the Word catheter can be pushed into the vagina for comfort (1).
Jacobi ring or substitute:
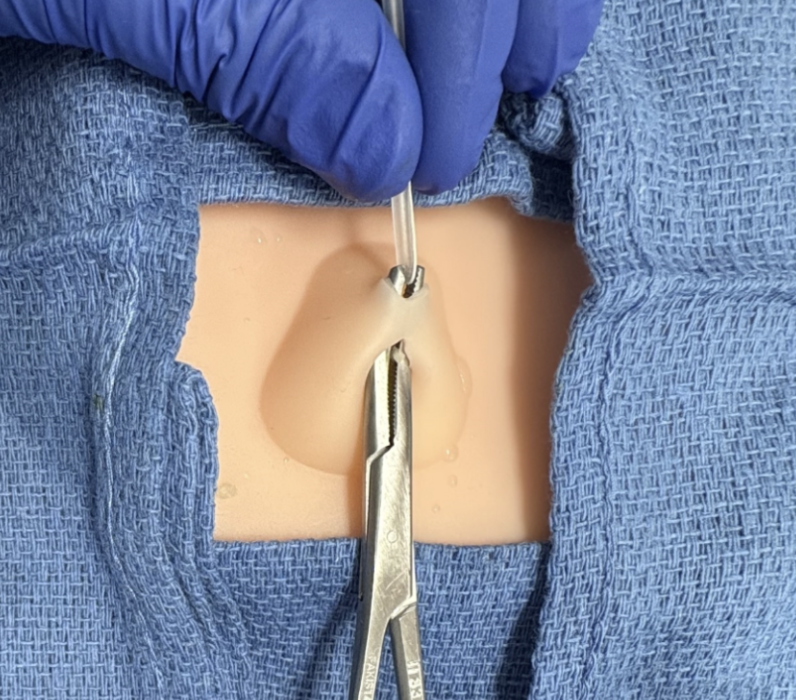
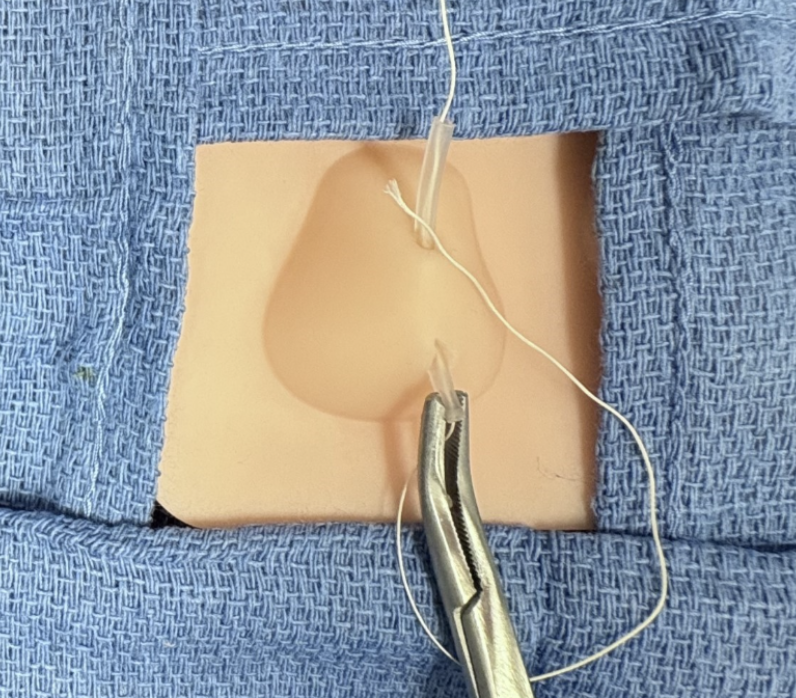
7d. Insert a curved hemostat into the initial incision.
7e. Create a tract with the hemostat and make a second stab incision with the scalpel at the other end of the tract. The second incision should still be in the inner mucosal surface.
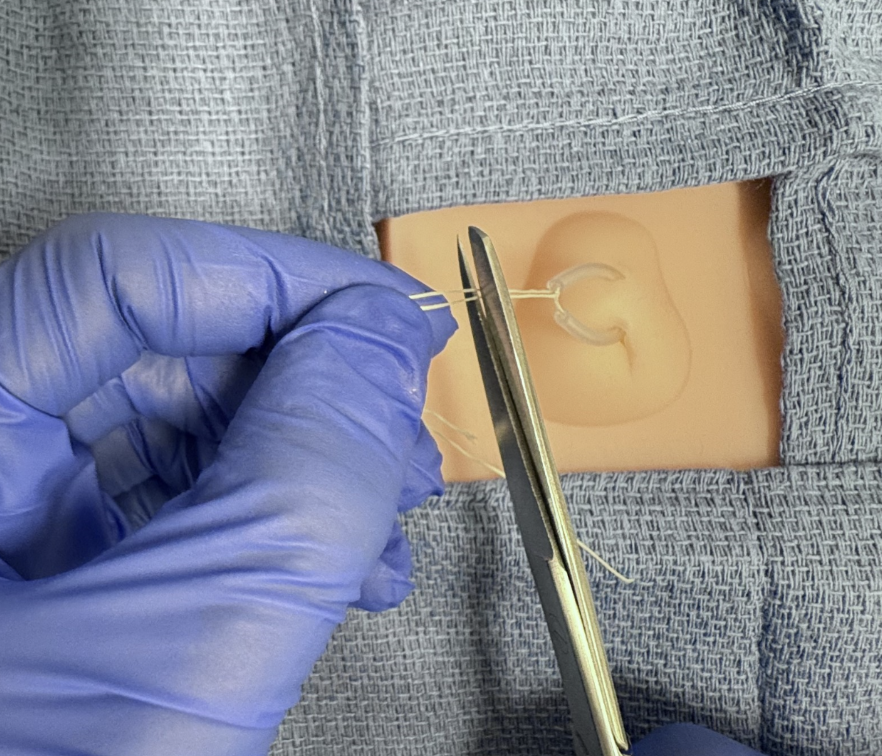
7f. Before removing the hemostat, grab the tubing with the hemostat.
7g. Pull tubing through the tracts with the hemostat.
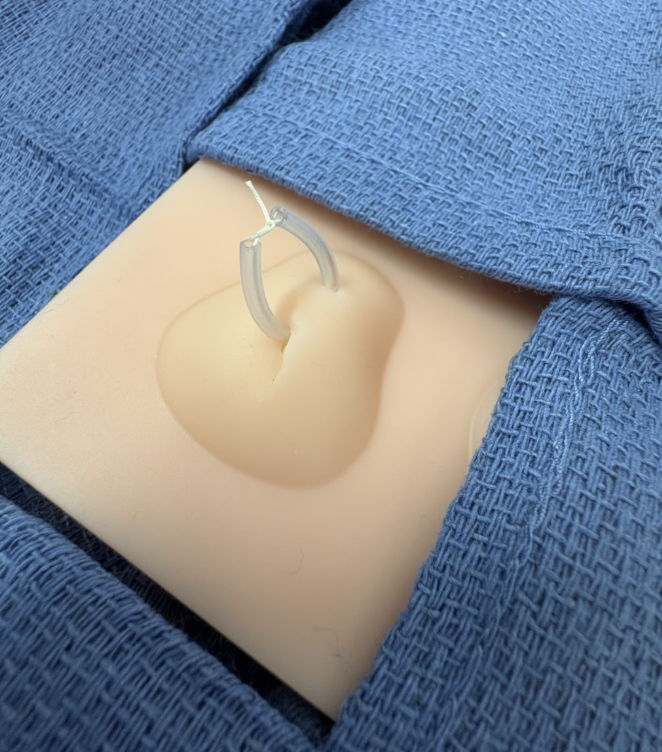
7h. Tie the two ends of tubing together to form a ring. Be sure to leave the loop loose enough such that it can still slide freely Trim any sharp or jagged edges on the ends of the loop to prevent discomfort or irritation to surrounding tissue (3).
DISPOSITION
The majority of patients will be appropriate for discharge. Consider hospital admission for patients with concerns for sepsis or for patients with indications for antibiotic therapy that are unable to tolerate oral antibiotics (4). Provide gynecology referral if they do not have an established gynecologist for Word catheter or Jacobi ring removal. This should occur in 2-4 weeks to allow for appropriate drainage and tract epithelization. The patient may also discuss additional interventions at this visit, such as a marsupialization procedure. Give instructions and/or materials for the patient to perform Sitz baths 2-3 times daily. This may help with discomfort and promote healing.
Post by victoria gabor, MD AND COLLEEN ARNOLD, MD
Dr. Gabor is a PGY-2 in Emergency Medicine at the University of Cincinnati
Dr. Arnold is a PGY-3 in Emergency Medicine at the University of Cincinnati and Mastering Minor Care Section Editor
Editing by ALEXA SABEDRA, MD and ANITA GOEL, MD
Dr. Sabedra is an Assistant Professor at the University of Cincinnati and a graduate of the UC EM Class of 2019
Dr. Goel is an Associate Professor at the University of Cincinnati and a graduate of the UC EM Class of 2018
References
Lee WA, Wittler M. Bartholin Gland Cyst. National Library of Medicine. Published 2020. https://www.ncbi.nlm.nih.gov/books/NBK532271/
Quaresma C, Sparzak PB. Anatomy, Abdomen and Pelvis: Bartholin Gland. National Library of Medicine. Published 2020. https://www.ncbi.nlm.nih.gov/books/NBK557803/
Omole F, Simmons BJ, Hacker Y. Management of Bartholin’s Duct Cyst and Gland Abscess. American Family Physician. 2003;68(1):135-140. Accessed July 27, 2022. https://www.aafp.org/pubs/afp/issues/2003/0701/p135.html
Chen KT. Bartholin gland masses. UpToDate. Published September 4, 2024. https://www.uptodate.com/contents/bartholin-gland-masses