Transfusion in Trauma: One Ratio to Rule them All??
/A couple weeks back we met for the first journal club of the year in our residency. For this first session, we tackled the clinical conundrum of transfusion ratios in trauma. The question came from a brainstorming session with the PGY-1 and 2 residents, where the following PICO question was derived:
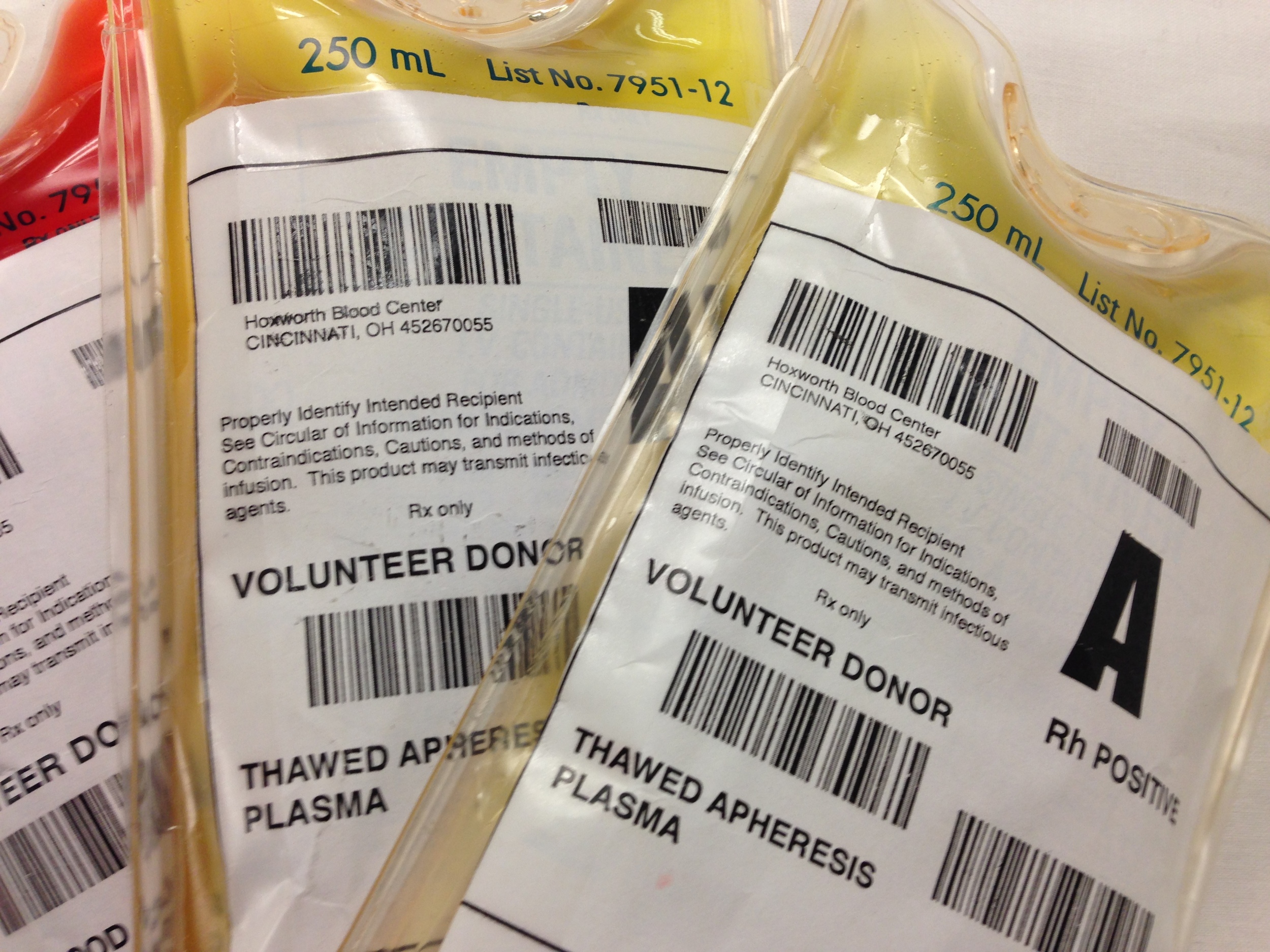
Patients: Victims of both blunt and penetrating trauma in need of blood transfusion as a part of the their initial resuscitation
Intervention: high plasma and platelet to PRBC ratio transfusion
Comparison: low plasma and platelet to PRBC ratio transfusion
Outcome: Mortality (in patient and 30 day mortality)
A literature search conducted on the spot led us to the following 3 articles which were analyzed and discussed in the Journal Club meeting last week:
- Holcomb, J. et al. (2013) The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) Study: Comparative Effectiveness of a Time-Varying Treatment With Competing Risks. JAMA Surgery. 148 (2). 127-136.
- Bhangu, A. Nepogodiev, D., Doughty, H., & Bowley, D. (2013) Meta-analysis of plasma to red blood cell ratios and mortality in massive blood transfusions for trauma. Injury. 44. 1693-1699. http://dx.doi.org/10.1016/j.injury.2012.07.193
- Hallet, J., Lauzier, F., Mailloux, O., Trottier, V., Archambault, P., Zarychanski, R., & Turgeon, A. (2013) The Use of Higher Platelet: RBC Transfusion Ratio in the Acute Phase of Trauma Resuscitation: A Systematic Review. Critical Care Medicine. 41(12). 2800-2811. DOI: 10.1097/CCM.0b013e31829a6ecb
The formal analysis sheets for each of these articles are attached below.
- PROMMTT Analysis Sheet
- Bhangu, et al Plasma Meta-Analysis Sheet
- Hallet, et al Platelet Systematic Review Analysis Sheet
Here are some of the highlights of the discussion and some of the key concepts you need to know when looking at this literature.
Survival Bias
Survival bias occurs when patients in the study can die before they have the potential to receive the intervention being studied. Studies looking at ratios of blood product transfusion in trauma can be especially prone to this. Why? The vast majority of trauma patients (especially during the time when these studies were conducted) will receive some quantity of packed red blood cells (which were and are readily available in resus bays) prior to the administration of plasma (which, depending on your system may need to be thawed and delivered from the blood bank). If you have a particularly sick trauma patient who dies 20 minutes after arrival, it simply isn’t possible for that patient to achieve a 1:1 (FFP:PRBC) transfusion ratio. If you choose to include those patients in your data analysis, you end up with a significantly higher mortality in the “control” or “low ratio” group compared to the “intervention” or “high ratio” group. Thus, you risk showing a difference in mortality when none really exists.
When Summarizing the Evidence, What Goes In, Comes Out
One of the articles analyzed is a meta-analysis (Bhangu, et al) and another is a systematic review (Hallet, et al). Analyzing either a systematic review or a meta-analysis, one must first assess the validity of the evidence. Ask yourself the following questions:
- Did they find all the evidence on the subject being analyzed?
- What was the quality of the papers they analyzed?
Answers to the first question can be found by looking at the search strategies employed by the authors. Did they search multiple databases? Are the search terms reasonable and inclusive? Did they comb through unpublished data (abstracts, conference proceedings, trial registries)? The search strategy should be reproducible and should make you feel comfortable that the authors aren’t analyzing a skewed sample of the literature.
Answers to the second question can be a little harder to come by. Ideally, the meta-analysis would include only randomized control trials with good blinding, concealment, and important patient-specific outcomes. The two review articles we discussed analyzed retrospective reviews and analyses of registries (with the rare exception being the prospective observational trial we also analyzed, PROMMTT). The articles that Hallet et al and Bhangu et al sought to analyze were all of fairly poor quality and suffered from risk of selection bias and survival bias.
Heterogeneity
When looking at a meta-analysis or systematic review, you should look to see how similar the results are from study to study. If the point estimates of effect and confidence intervals for all of the included studies are similar, it should increase your confidence in the summary estimate of effect. If there are significant differences, it should lower your confidence in the summary estimate of effect.
You can estimate the degree of heterogeneity by visual inspection.
Some Heterogeneity = Lowered Confidence in Summary Estimate
Low Heterogeneity = Increased Confidence in Summary Estimate
Or, you can look at a couple of statistical tests that should be performed and displayed with the results.
Tests for heterogeneity include:
- Yes-No tests - These assess the null hypothesis that the observed effects are similar across studies and differences observed in the effect size between studies are due to chance. (1) Thus, a low p (< 0.05) tells you that the observed differences between the groups are NOT due to chance (i.e. there really ARE differences in effect in the studies analyzed and there IS heterogeneity in the studies). Simply put, a low p-value is bad. A low p-value for tests of heterogeneity should lower your confidence in the summary estimate of effect
- I2 test - “describes the percentage of the variability in effect estimates that is due to underlying differences in effect rather than chance” (1)
- Rough guidelines: <20% suggests minimal variability, >50% suggests significant heterogeneity
What did we see in the papers we looked at?
Hallet, et al basically found such significant heterogeneity in the literature after conducting their literature search that they changed from doing a meta-analysis to a systematic review.
In Bhangu, et al, most all of the comparisons were impacted by significant heterogeneity. The results they found were:
For 24 hr mortality:
- For plasma:RBC ratio >1:1.5, OR = 0.34 (0.23-0.50) with low heterogeneity (2 studies)
For 30 day/in-hospital mortality:
- For plasma:RBC ratio >1:1.1, OR = 0.50 (0.37-0.68) with low heterogeneity (2 studies - same as above)
- For plasma:RBC ratio of 1:2, OR = 0.49 (0.31-0.80) with substantial heterogeneity (4 studies)
- For plasma:RBC ratio >1:2, OR = 0.56 (0.40-0.78 with substantial heterogeneity (6 studies)
- For plasma:RBC ratio 1:2.5-1:4, OR = 0.41 (0.16-1.00) with substantial heterogeneity (3 studies)
What about PROMMTT?
PROMMTT was a prospective, observational, multi-center trial that examined mortality in patients transfused a low plasma:RBC ratio (<1:2), moderate ratio (>1:2 but less than 1:1, and high ratio (>1:1).
When you look at a prospective observational article, one question you should ask yourself is: Were the groups studied balanced in terms of known prognostic risk at the beginning of the study?
In an RCT, the process of randomization accomplishes this for us. Randomization balances known and unknown prognostic factors. Without randomization, prospective observational trials can be prone to baseline imbalances of prognostic risk that can affect the stated outcomes. Unfortunately, PROMMTT does not describe the composition of the 3 analyzed groups. Thus, we are left not knowing whether or not the low ratio group had a significantly higher proportion of head trauma, greater overall injury severity score, was made up of a disproportionately older cohort of patients, etc, etc.
Add to this the significant differences in the way patients were transfused*, and we are left without full confidence in the results described by the authors.
*The paper describes significant differences in blood product administration from patient to patient. One patient may have received 4 units of PRBCs up front, then 4 units of FFP, then 6 units of PRBCs, then a 6-pack of platelets. Another patient may have received 8 units of PRBCs up front then 4 units of FFP, then 2 units PRBCs, then 4 units of FFP. These patients were NOT administered a fixed ratio of blood products from time-zero, or ED arrival, through their hospitalization.
Bringing It All Together
The evidence for transfusion of any given ratio of FFP:PRBCs or platelets:PRBCs is in no way settled. The current published literature, though limited by a number of the factors mentioned above, suggests that there may be a benefit in mortality for transfusion of higher volumes of plasma (perhaps with the greatest benefit with a transfusion ratio somewhere in the 1:1.5-2 plasma:RBC range). There will surely be more literature published in this arena. Of particular interest will be the analysis of TEG/ROTEM guided resuscitations (not covered in our lit review), transfusion ratios for particular types of traumatic injuries (blunt head injury vs torso and abdominal trauma), and investigation of the safety of high ratio resuscitations (incidence of transfusion associated lung injury, sepsis, multi organ system failure - only touched upon by the current literature)