Induction Reduction?
/Driver, B. E., Trent, S. A., Prekker, M. E., Reardon, R. F. & Brown, C. A. Sedative Dose for Rapid Sequence Intubation and Postintubation Hypotension: Is There an Association? Ann. Emerg. Med. (2023) doi:10.1016/j.annemergmed.2023.05.014.
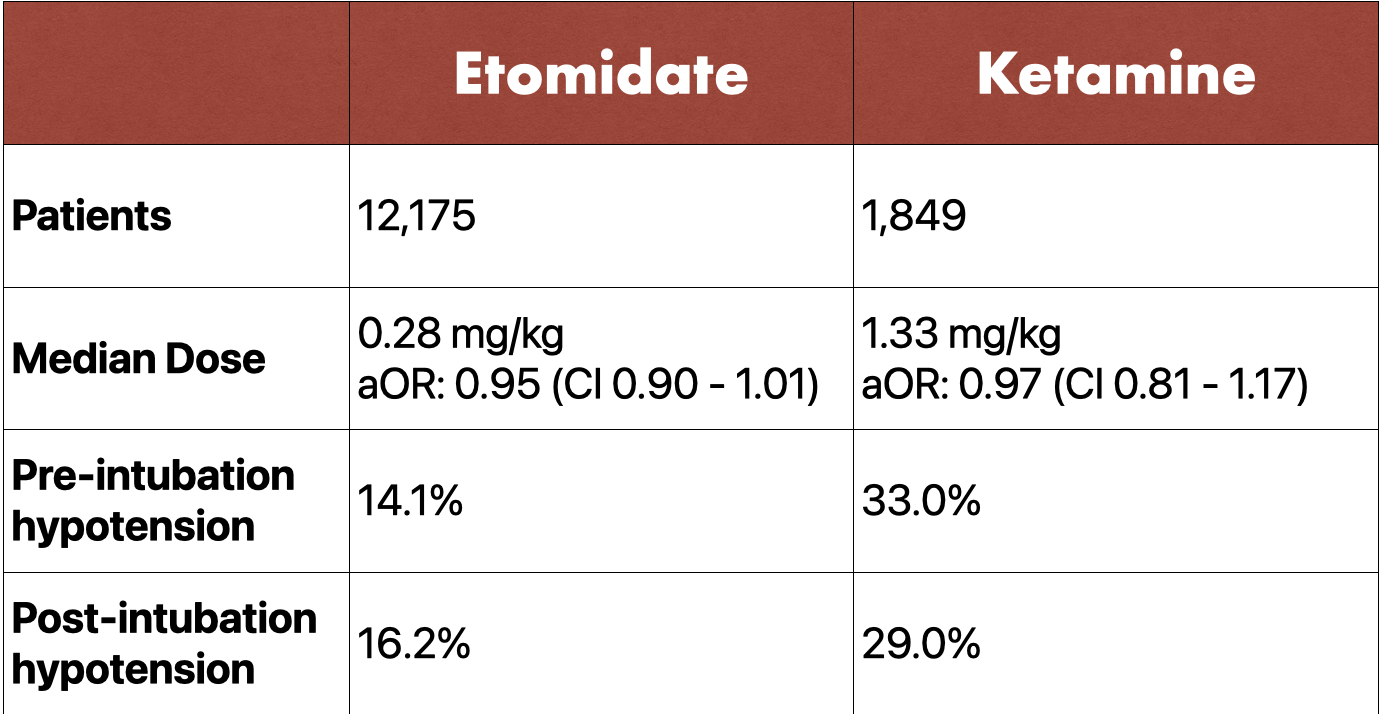
Clinical Question: Does the dose of etomidate or ketamine play a role in post-intubation hypotension?
Background
Rapid sequence intubation (RSI) is frequently performed under emergent conditions in acutely ill patients. RSI is a technique for managing the emergency airway that induces immediate unresponsiveness (induction agent) and muscular relaxation (neuromuscular blocking agent). In properly selected patients, it is a quick, safe, and effective approach that results in optimal intubating conditions. However, one of the feared complications of RSI is post-intubation hypotension leading to cardiovascular collapse. Although there are multiple possible reasons for hypotension post-intubation, the choice and dosing of induction agents has been implicated. In recent times, numerous studies and expert recommendations have opted for ketamine over etomidate in a critically ill-patients due to a theoretically better safety profile. Additionally, ketamine has been preferred as an induction agent over both propofol and midazolam due to their known dose-dependent impacts on hemodynamics. Despite ketamine’s superior safety profile to propofol and midazolam, there is scant data comparing ketamine to etomidate, or investigating the safety and efficacy of lowering the dose of these induction agents.
Study Design
This was an observational study that performed secondary analysis of data from a prospective registry. Study population was patients > 14 years of age who required intubation that was facilitated with etomidate or ketamine. Data was obtained from the National Emergency Airway Registry (NEAR). The NEAR database is a multi-center, prospective, observational, emergency medicine led registry. Exclusion criteria were pre-intubation hypotension, use of topical anesthesia, or missing data including primary outcome, patient weight, etomidate / ketamine dose.
Primary outcome was post-intubation hypotension, defined as SBP < 100mg Hg within the first 15 minutes post-intubation. Secondary outcome was post-intubation hypotension treated with IV fluids or vasoactive agents. Multivariable modeling was used to determine if drug dose (mg/kg) was independently associated with the outcomes as noted above.
Results
Conclusion
Neither etomidate or ketamine dose was significantly associated with post-intubation hypotension (primary outcome) or hypotension requiring fluids or vasopressors (secondary outcome). Results were similar in sensitivity analysis excluding patients with pre-intubation hypotension and including only patients intubated for shock.
Discussion
The study concluded with the statement that “in this large registry of patients intubated after receiving either etomidate or ketamine, we observed no association between the weight-based sedative dose and postintubation hypotension.” However, we know that intrinsically and per their mechanism of action, etomidate and ketamine do not have effects on blood pressure. Therefore, changing the dose of the medication, theoretically, should not affect a patient's hemodynamics. This then begs the question, why were the individual agents picked in each scenario and did the decision to pick one drug over the other influence the results? The strengths of this data come from the fact that there were broad inclusion criteria and there was a large database to evaluate, resulting in a large population that was analyzed. The study population used in this study is generally similar to the population encountered daily in the average emergency department in the United States. Unfortunately, the study is limited by the fact that it was an observational study and by the limited details available as to why an induction agent or its specific dose was selected. Additionally, this study did not address the potential for awareness in patients who received reduction of sedative dosing. And, minimal information was provided in regards to any other treatments apart from the induction agent that could have induced hypotension and confounded the results. At the end of the day, optimization of a patient's hemodynamic status should be of prime focus so as to avoid post-intubation hypotension regardless of the induction agent of choice.
Authorship
Written by: Raveena Chhabria, MD, PGY-3, University of Cincinnati Department of Emergency Medicine
Audio Recording and Editing by Saie Joshi, MD, PGY-2, University of Cincinnati Department of Emergency Medicine
Peer Review and Editing by Jeffery Hill, MD MEd, Associate Professor, University of Cincinnati Department of Emergency Medicine
Cite As
Chhabria, R., Joshi, S. Hill, J. Induction Reduction?. TamingtheSRU. www.tamingthesru.com/blog/journal-club/inductionreduction. 9/22/2023