Ventilator Management Simulation Debriefing
/Case 1 - "Bucking the Vent"
You have inherited a patient in the VA MICU at signout. The patient presented with spontaneous bacterial peritonitis and altered mental status and was intubated for airway protection and hypoxic/hypercarbic respiratory failure. The patient’s altered mental status has resolved but the patient remains intubated waiting for a second large-volume paracentesis that can’t be done over the long weekend at the VA. The RT calls you asking for a one time dose of 5mg Versed, but on a quick glance at the chart, the patient has been getting these Q2 hours for the last several days. You go to the bedside and find an agitated patient motioning to take out the tube. “He’s bucking the vent doc!”
Vent settings: AC-VC: TV500 RR12 PEEP8 FiO2 30%
Debrief
This is a basic case to discuss vent comfort and issues with compliance that we see in patients lying flat or with truncal obesity. When evaluating for patient-ventilator dyssynchrony:
- Consider life threatening causes of distress - Hypoxia, hypercapnia, tension pneumothorax, or dynamic hyperinflation
- Consider the need for ongoing mechanical support. - If necessary, adjust vent settings and consider more comfortable modes of ventilation
- Address Analgosedation - Make your patient comfortable
Take Home Points:
Pure volume control (or CMV) has constant flow / accelerating pressure waveforms (as opposed to autoflow or pressure control) and will cause dyssynchrony with many spontaneous breathing patient. SIMV-VC→ similar problems
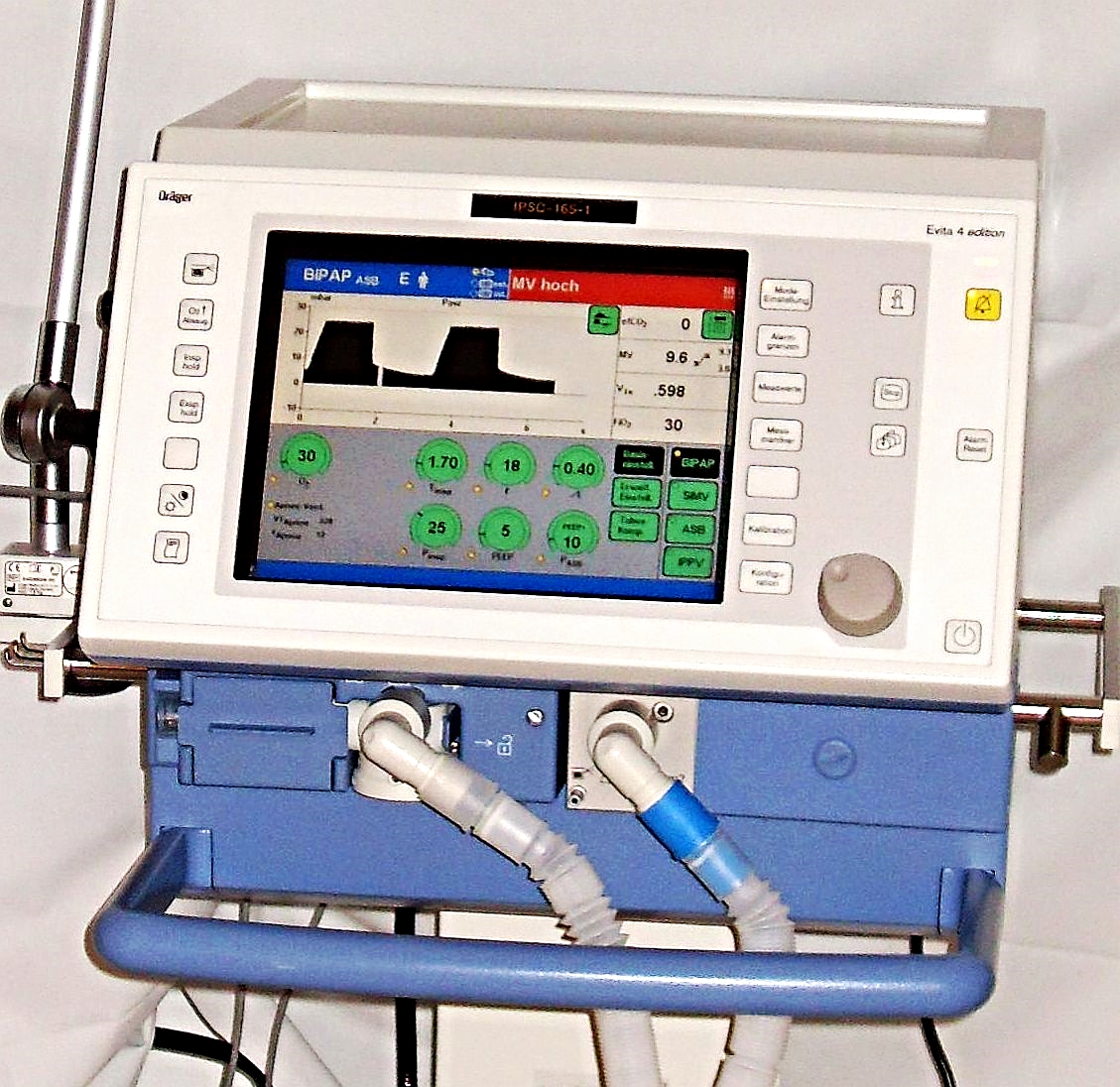
Autoflow is a registered trademark of Drager. It is not PRVC (but is similar - as is VC+). It converts a volume mode to a volume targeted, pressure limited mode. The goal is to deliver the set tidal at the lowest possible pressure (plateau pressure) utilizing a decelerating gas flow pattern. It automatically adjusts the flow and pressure based on lung compliance.
One major drawback of these modes is the scenario when the patient desires a greater tidal volume than the set volume. While the patient works to increase Vt, the vent will actually decrease pressure in an attempt to reach the set Vt regardless of the patient.
Criteria for extubation:
Ability to protect airway
Ability to adequately oxygenation
Ability to adequately ventilation
Predicted clinical course
Use the SBT to assess: Rapid Shallow Breathing Index (RSBI) = RR/VT < 100, NIF > 20 cm H2O
Kipp’s Pro Tips
“Don’t fix blood gases. Fix the waveforms, and you fix the patient.”
“The first thing I would address is the inspiration you time by looking at the P-V loop. This will allow for the patient and the vent to cycle off the breath at the same time, therefore increasing synchrony.”
Case 2 - Trapping Air
Helicopter inbound from Dearheart County for an asthmatic in respiratory distress. The crew walks into the SRU bagging a patient they just intubated. The crew sighs relief and proudly reports the patient was successfully intubated with benadryl and versed no less than 3 minutes before they landed. The medic has been bagging because a mouse built a nest in their ventilator, so it was thus out of commision. The patient is an 18 y/o M, 5’6”, 220 lbs.
Debrief
This is a case to discuss management of the sick patient with obstructive lung disease. There are a couple important underlying principles. It starts with the decision to intubate this patient, was it purely for hypoxia as in the sick asthmatic? Or is there a component of hypercarbic respiratory failure as well? Regardless, the initial vent settings (including the mode) are very important. A couple overarching principles in addition to using all the classic treatments for reactive airway disease apply:
Ketamine for intubation look may help with bronchodilation.
Shoot for TV between 6-8mL per Kg via a decelerating flow mode to decrease turbulent flow
Paralyzing asthmatics is controversial. A non-paralyzed patient will be able to participate in respiration, which in theory decreases compliance / improves exhalation. There is no perfect I:E ratio but shooting for an initial ratio is 1:3 or 1:4 is reasonable. Keeping the I:E ratio as low as possible will decrease flow and therefore turbulence
Increasing flow may actually increase your PIPs, which may limit the volume delivered depending on the mode and alarm settings
Permissive hypercapnia is okay for intubated asthmatics and COPD. You will have to correct it prior to extubation, but you can worry about that once lung dynamics have improved.
Recognize autoPEEP (dynamic hyperinflation) by flow or volume not returning to baseline
- Fix by increasing I:E ratio or decreasing volume/respiratory rate.
- ePEEP is extrinsic PEEP - this is the PEEP you set on the vent
- iPEEP is intrinsic PEEP, often caused by air trapping (autoPEEPing), and can be measured by end expiratory hold
- Matching ePEEP to iPEEP may stent open distal airways and prevent air trapping
Kipp’s Pro-tip: "the flow/volume loop will also not return to baseline"
Case 3 - Dazed and Confused
ColeTrain Township brings a nursing home patient to the SRU. The patient was last seen normal 5 years ago, but today was noted to have fever. Neither a name nor a list of medical problems, except for the fact that she is a full code, were included in the stack of papers provided by the nursing facility. She is tiny little lady, 5’1”, 94lbs. She is sick, altered, and making gurgling sounds with each breath.
HR 145 BP 65/20 RR 28 O2 90% on RA T 100.8
Labs remarkable for pH 7.05, pCO2 of 20. CXR with hazy opacity at R lung base. You quickly add on a urine legionella before you page the R2 overhead. “R2 to the SRU for the ICU hat trick.”
Debrief
This is a classic case of the extremely high risk intubation. Hypotension occurs after 20-30% of intubations and is directly associated with increased in hospital mortality. We need to actively avoid this and optimize intubation conditions for the best possible outcome.
Optimize pre-intubation hemodynamics - Adequately fluid resuscitate the patient & have push dose pressors available
Drug choice - Consider decreased doses of the sedative-hypnotics but full doses of paralytics
Vent settings - ARDSNet protocol: TV 6-8ml/kg
Developed in up to 28% of severe sepsis / septic shock patients
Match the patient’s pre-intubation minute ventilation (compensatory respiratory alkalosis)
Consider continuous ETCO2 monitoring with goal in mid to low 20s!
Wean FiO2 as soon as possible, hypoxia/hyperoxia are likely both detrimental
Cuff leaks:
Inhaled volume will be significantly greater than exhaled volume
Airway pressures may be low
PIP reflects upper airways (resistance); plateau pressure reflects lower airway (compliance)
DDx for increased resistance - Coughing/dyssynchrony, tube kink, bronchospasm, partial mucous plug
DDx for decreased compliance - ARDS/ALI, PTX, atelectasis, PNA, complete mucous plug, pulm edema, chest wall rigidity, abdominal compartment syndrome, auto-PEEP / air trapping
Kipp’s Pro Tip
“Be careful using EtCO2 to adjust vent settings especially in a hemodynamically unstable patient. Ventilation is only one part of V/Q.”
DOPES: An approach to the crashing patient on the vent
Dislodgement of ETT - Verify with ETCO2 and physical exam
Obstruction - Attempt to pass suction catheter
Pneumothorax - Consider bedside ultrasound for lung sliding (may also use for ETT placement)
Equipment - Disconnect patient from vent if any concern for equipment failure
Stacking (breath stacking) - Check waveforms and consider disconnecting patient from vent