Thromboelastography aka The TEG
/What is TEG?
Thromboelastography (TEG) measures the dynamics of clot development, stabilization/strength, and dissolution. Assuming the body’s ability to achieve hemostasis is a function of these clot properties, TEG provides specific, real-time indicators of a patient’s in vitro hemostatic state. This is in contrast to routine screening coagulation tests such as aPTT and PT/INR which are run with blood plasma alone and therefore do not take into account the cellular components of clotting.
How to read a TEG
TEG creates a graphical representation of the movement of a small pin suspended in a cup of whole blood as hemostatsis occurs. As the blood begins to clot and adhere to the pin, the movement of the pin increases. This increasing movement is interpreted by the computer as increasing amplitude on the TEG graph.
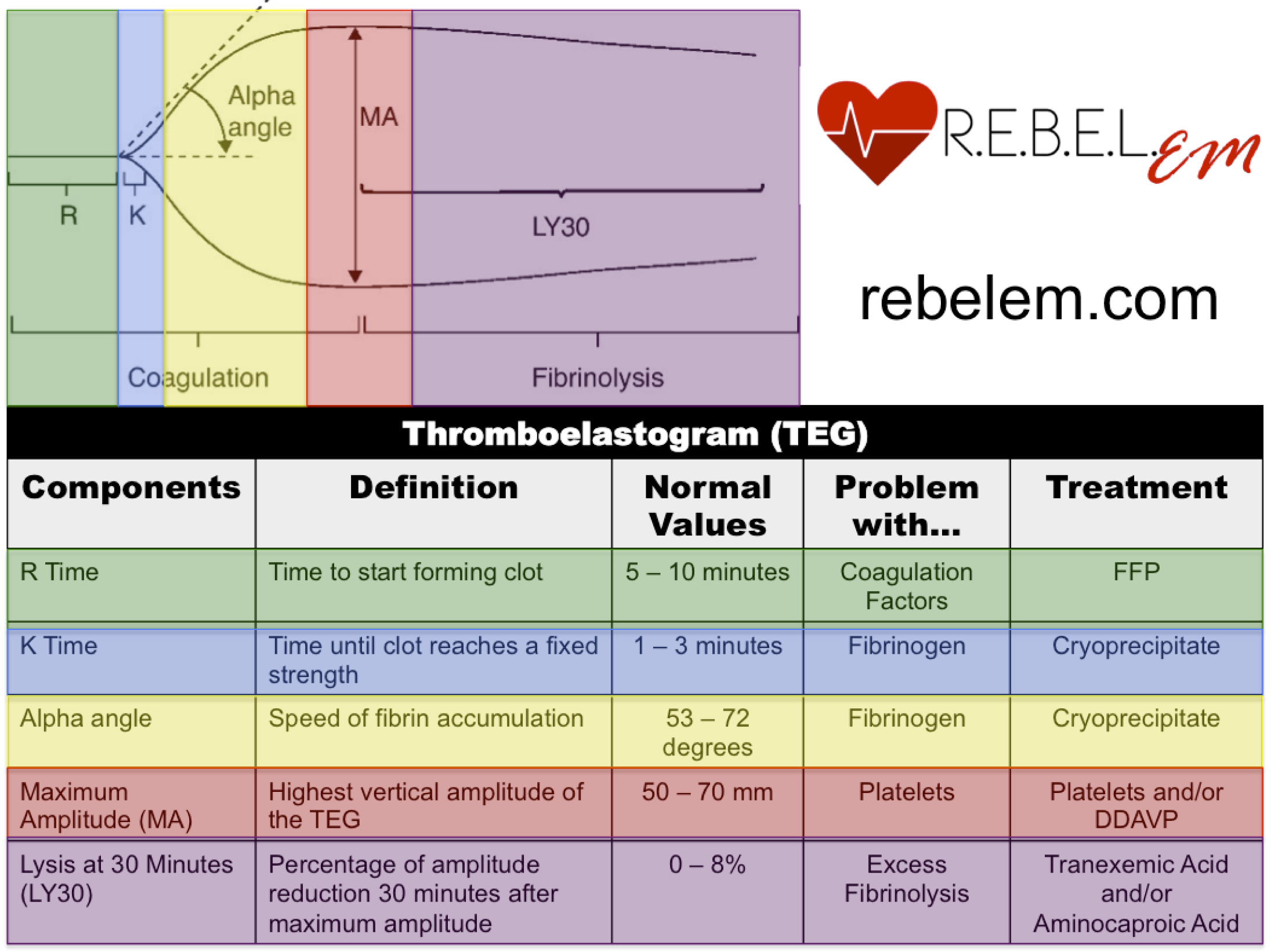
The image below, courtesy of R.E.B.E.L. EM, depicts a normal TEG and describes how to interpret it.
From Rezaie, S. Rebel Review #54 Thromboelastogram (TEG). http://rebelem.com/rebel-reviews/
*Note: contribution to maximum amplitude (MA) is ~80% platelets and ~20% fibrinogen, therefore MA can be decreased in hypofibrinoginemia
Time to Practice!
Case 1: 14 year-old male who presents with a chief complaint of rash. He states the rash came on over the past week and he also has noticed spots of blood when he blows his nose. He does not take any medications or supplements. On physical exam you note flat, red, non-blanching lesions on his bilateral lower legs. As you begin to examine his nose he starts to exsanguinate from the nares….
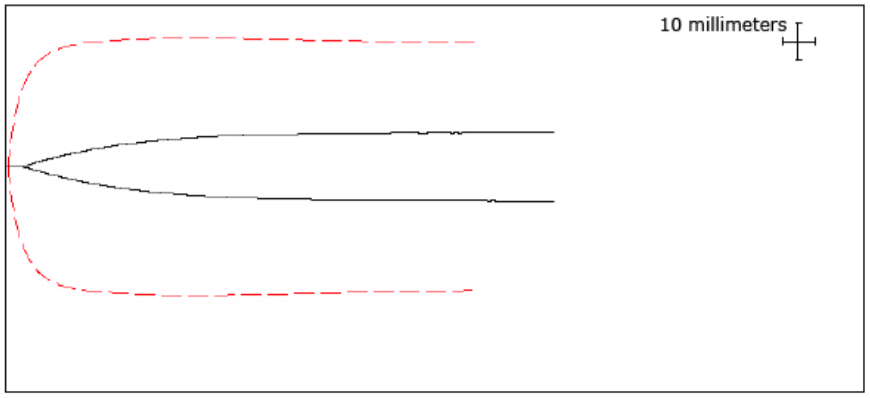
Note: The dashed red line represents a normal TEG and the black line is your patient’s read out
Which TEG parameters are abnormal?
- Low alpha angle, Low MA
What is the patient’s clotting abnormality?
- The patient is thrombocytopenic or has platelet dysfunction (less likely given patient history…see BONUS)
How will you use these TEG results?
- Consider transfusing platelets (or DDAVP for platelet dysfunction)
BONUS: What is the diagnosis?
- Immune Thrombocytopenia
Case 2: 26 year-old male arrives in the SRU 30 minutes after sustaining 2 GSWs to the chest. Vitals: BP 60/40 HR 115 O2Sat 88% on nonrebreather. Resuscitation is started and you send off a TEG….
Which TEG parameters are abnormal?
- Low MA, High Ly30
What is the patient’s clotting abnormality?
- High Ly30 indicates rapid fibrinolysis, likely initiating prior to achievement of maximal clot strength (maximum amplitude, MA). Therefore, low MA is more likely a reflection of rapid fibrinolysis rather than platelet dysfunction/deficiency
How will you use these TEG results?
- Transfuse TXA
BONUS: What is the diagnosis?
- Acute traumatic coagulopathy (ATC), this can occur early after injury in the setting of hypoperfusion and is thought to be independent from coagulopathy secondary to acidosis, hypothermia, or hemodilution. ATC is thought to be caused by dysregulation of Protien C.
Case 3: 42 year-old female arrives in the SRU 40 minutes after an MVC in which she was ejected from the car. EMS reports they found her significantly obtunded with a large contusion on her forehead and obvious bilateral femur deformity. Vitals: BP 110/60 HR 107 O2Sat 93% on room air. As the R2 prepares for intubation you notice that she has significant bleeding around the site of her IV. You send off a TEG….
Which TEG parameters are abnormal?
- Long R time, Long K time, Low alpha angle, Low MA
What is the patient’s clotting abnormality?
Long R time- patient is deficient in clotting factors
Long K time- patient is deficient in fibrinogen (factor I)
Low alpha angle/MA- patient is deficient in platelets or has platelet dysfunction
How will you use these TEG results?
- Consider transfusing FFP for clotting factor deficiency, Cryoprecipitate for hypofibrinoginemia, platelets for thrombocytopenia
BONUS: What is the diagnosis?
- Trauma induced DIC. Damage to vascular endothelium releases large amounts of tissue factor and other procoagulants => consumption of clotting factors, fibrinogen, and platelets. More damage = more likely to develop DIC, also associated with severe head trauma.
References
- Da Luz, LT, Nascimento, B, Shankarakutty, AK, Rizoli, S, Adhikari, NKJ. (2014). Effect of thromboelastography (TEG®) and rotational thromboelastometry (ROTEM®) on diagnosis of coagulopathy, transfusion guidance and mortality in trauma: descriptive systematic review. Critical Care 2014, 18:518
- Afshari A, Wikkelsø A, Brok J, Møller AM, Wetterslev J. (2011). Thrombelastography (TEG) or thromboelastometry (ROTEM) to monitor haemotherapy versus usual care in patients with massive transfusion (Review). The Cochrane Library 2011, Issue 3.
- Cohen, M and Kutcher, ME. Coagulopathy Associated with Trauma. In: UpToDate, Colins, KA (Ed), UpToDate, Waltham, MA. (Accessed on July 30, 2015.)
- Harrison, P. Platelet Function Testing. In: UpToDate, Tirnauer, JS (Ed), UpToDate, Waltham, MA. (Accessed on July 30, 2015.)
- R.E.B.E.L. EM