Grand Rounds Recap 9/16
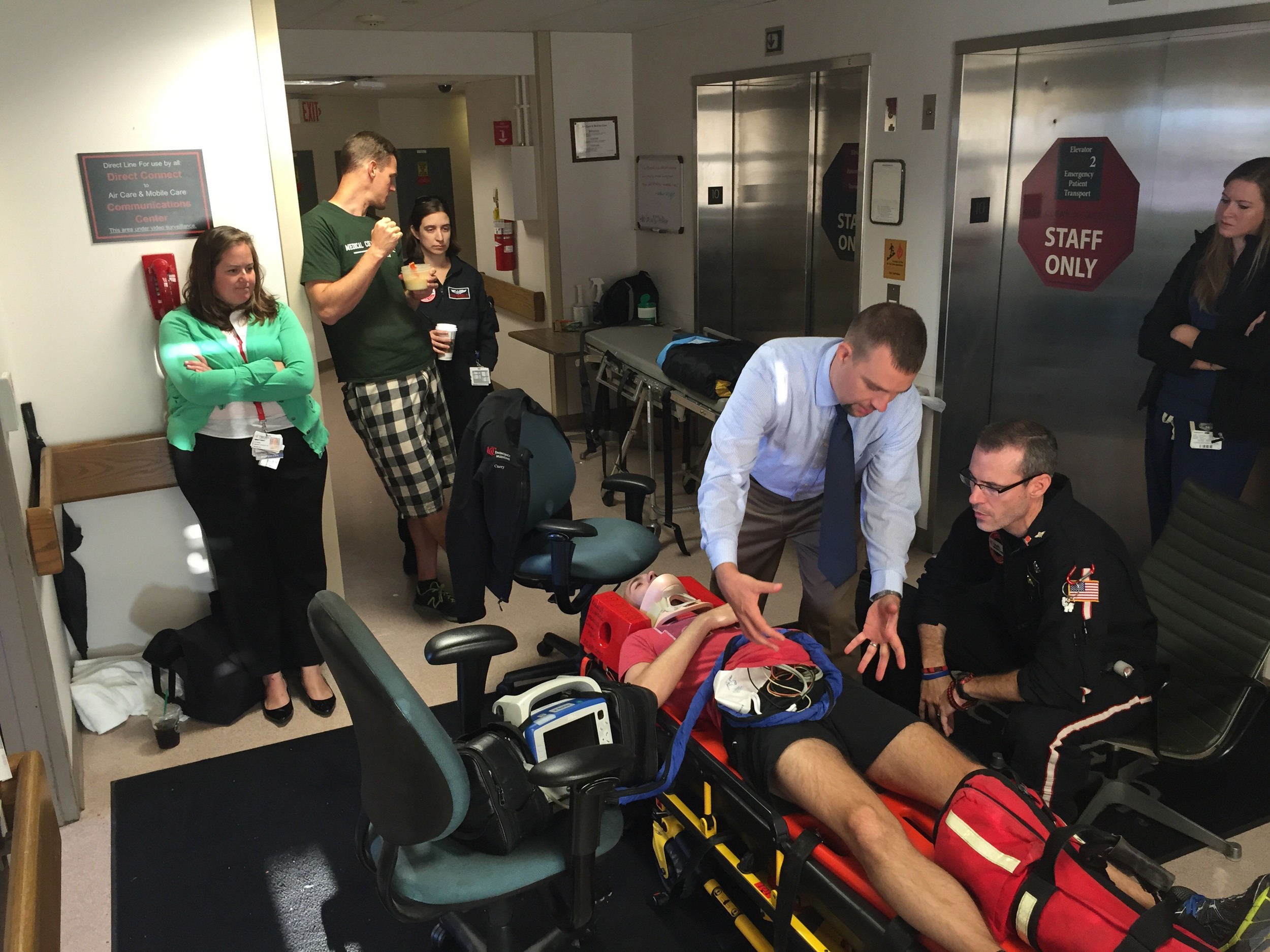
/Air Care Grand Rounds
What do I need to assess before I load this patient in the heli?
- Does your patient need plastic? (ETT, needle/finger thoracostomy)
- Get breath sounds / anticipate your possible interventions you may need
- Is your patient in shock?
- Don't have a lactate? Hyperglycemia in the absence of diabetes, thirst and diaphoresis should lend you towards 'yes'
What is Crew Resource Management
Know the strengths and attributes of your crew, what they can do, and how you can work together to make the mission successful and safe
Other tips from the morning
- To estimate IBW - start with 50kg for 5ft patient, add 2.3kg for each additional inch of height
- Use the pediatric vent circuit for any patients < 25kg
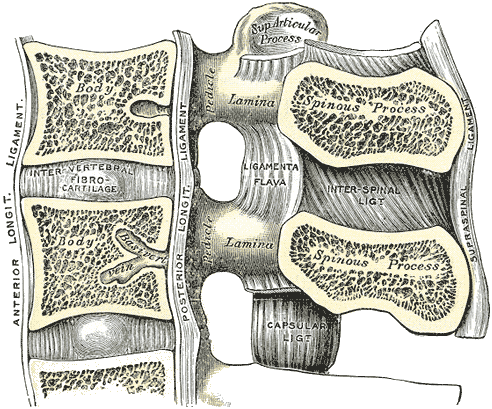
Ultrasound-Guided LP with Dr. Carleton
Why are LPs your least favorite procedure?
- Elderly (calcified ligaments, inflexible spines, poor reserve)
- Obese (lack of landmarks, long distance, poor reserve)
- Children (poor compliance, respiratory compromise)
So does US improve our attempts?
Peterson el al AEM 204, 15% increase in success rate (trend w/o statistical significance) with using ultrasound for routine LP
3 myths of the Lumbar Puncture
- Interiliac line identifies L4
- One level higher of lower in up to 33% of patients
- Palpation reliably identifies the level
- Ultrasound 71% accurate
- Palpation 29% accurate
- The spinal cord ends at L1-L2
- 50% of patients have extension to L2, 3% extend to L3
- Greatest chance of variability in women/children
Great - now I am terrified. Tell me how to do this right with some soundwaves
- Identify your level (start longitudinal at L5-S1 and work up)
- Identify the midline in the transverse view
- Identify and explore the interspinous space in the longitudinal view
- Identify and mark anticipated site of entry and angle
- Determine the depth of the ligamentum flavum / dural complex in the cross-sectional plane
Mike and Matt from the Ultrasound Podcast have a great example of how to do this
Case Follow up with Dr. Betham
- Angioedema can be divided into two main mechanisms: Histamine mediated and Bradykinin mediated
- Histamine mediated including anaphylaxis, occurs after exposure to an antigen (environmental, drug, food, etc)
- typically rapid onset < 1 hour and lasts for hours
- Responds to therapy of H1 and H2 antagonists, epinephrine, and steroids
- Bradykinin mediated including Hereditary Angioedema, ACE inhibitor induced, and acquired.
- Occurs as a result of increased quantities of bradykinin, a molecule that causes vasodilation and increased vascular permeability
- Slower onset over several hours, lasts 24 hours to several days
- Typically does not respond to antihistamines, steroids, or epinephrine
- Targeted therapies are approved for hereditary angioedema (plasma derived C1 esterase, ecallantide, icatibant) but are not approved for ACE inhibitor related angioedema
- Consensus guidelines recommend standard treatment for angioedema for all undifferentiated patients, however bradykinin mediated angioedema is unlikely to respond.
- Start all assessments with airway, breathing, and circulation.
- Early nasopharyngoscopy or other laryngeal assessment in patients who do not need immediate intervention is recommended to determine extent of supraglottic swelling
- Awake, video-assisted intubation techniques are recommended if needed and early ENT assessment (where available) is also recommended for evaluation for possible surgical airway.
- Histamine mediated including anaphylaxis, occurs after exposure to an antigen (environmental, drug, food, etc)
- Bougie-Assisted Emergent Cricothyroidotomy Pearls
- Get to know your cricothyroidotomy kit ahead of time, know what it contains and how to use it. They are not all the same.
- Prepare yourself before the time comes:
- You can complete a cricothyroidotomy with nothing more than a scapel, bougie, and ET tube.
- If you can’t feel landmarks or the membrane on the skin due to body habitus, you can reassess after your incision.
- The bougie is crucial confirm placement in the trachea and hold the track.
- Beware the victory thrust in the heat of the moment, the balloon of the ET tube should just past through the trachea.
Case Follow up with Dr. Gorder
Pulmonary complications of IV opiate use
Pure respiratory depression is the most commonly seen complication in overdoses
Aspiration pneumonia is common in the post-overdose setting and its incidence is on the rise
IV heroin users are at greater risk for CAP, regardless of their HIV or Hep C status
Non-cardiogenic pulmonary edema is a known complication post-overdose
On the ARDS spectrum; defined as clinical or radiographic evidence of alveolar fluid accumulation with hemodynamic evidence of a cardiac etiology
Seen in 2-10% of all heroin overdoses and almost 100% of autopsy cases after opiate overdose
Presents rapidly after overdose, requires mechanical ventilation ~40% of the time and resolves quickly (24-48 hours)
Cause unknown but may be immune-modulated, a histamine response, or neurogenic in etiology
Jury is still out on narcan-induced pulmonary edema, so don’t be afraid to give patients the narcan they need
Inhalation of heroin can cause an eosinophilic pneumonia
They may present looking like an asthma patient
Treatment is steroids
Injection talcosis is caused by the filler products in prescription drugs or street drugs getting lodged in the pulmonary interstitium
Can cause fibrosis, granulomas and BOOP