Grand Rounds Recap 2/10/16
/R4 QUARTERLY SIMULATION with Drs. Curry, Loftus, Ostro and Strong
We presented a case of a 42 y/o female who presented with altered mental status, hypotension and bradycardia. She was ultimately found to have an unintentional labetalol overdose which she had been taking PRN for headache.
Beta-Blocker Overdose Take-Home Points:
- Hypoglycemia, from beta-blocker inhibition of glycolysis and glycogenolysis, can help differentiate BB overdose from CCB
- Fluids, atropine, pacing and glucagon are the main initial therapies
- Glucagon is given at 5mg IV bolus, repeat at 5 minutes. If there is a response you can start a drip of 2-5mg/hr in D5 or D10. You will quickly deplete your hospital's entire supply of glucagon
- HIET (high-dose insulin euglycemic therapy): 1u/kg bolus then 0.5-1u/kg/hr drip. Usually they do not get hypoglycemic
- Can use intralipid therapy as well. The dose is 1.5ml/kg of 20% intralipid followed by 0.25 mL/kg/min for 30-60 minutes
Chairman's Hour with Dr. Pancioli
Dr. Pancioli, Chair and Richard Levy Professor of Emergency Medicine, engaged us in a talk regarding the operations and business of operating an academic medical center in the current healthcare climate.
What makes an academic medical center work?
- Highly reliant on complex care for margins
- Seeing a high volume of simple cases quickly often not a core competency
- Tough to compete with high service community providers for low complexity cases
What is the ED's involvement?
- An academic health center needs sick patients in order to remain financially solvent
- How can we be a good steward of the "front door"? How do we contribute to bringing patients in to the system?
- If we give good customer service and timely treatment we can build a reputation and increase patients (and their families) wanting to come into our system
- We can work with EMS to create brand loyalty and educate on our capabilities to get them to bring us the patients
- We contribute to the specialized care that is usually only available in major academic medical centers (Trauma care, Post-ROSC cooling, ECMO, etc...)
ACEP Policy Statement
- Boarding contributes to
- Lower quality of care
- Reduced timeliness of care
- Reduced patient satisfaction
We have to reach a balance between importing patients while also managing our "front door" volumes and reducing ED boarding....a tough balance.
Physics
- The hospital is essentially a fixed container
- Fixed number of inpatient beds (and ED beds)
- Any increase in volume when a container is full significantly increases the pressure
- So how do we fix the "pressure" problem
- Build a new tower? That takes 3-5 years
- Add more beds in our current space? That takes 15-18 months
- Decrease the number of patients coming?
- EMS will not want to bring their patients to us if they know they have to wait to get beds and a large percentage of those patients end up getting admitted
- Improve efficiency
- Can we really do this?YES! Just moving a few patients through more efficiently can probably make a big difference with respect to beds available to see patients and the numbers support that there is only a small N (potentially single digits) that separates us from days where we are efficient to being under "pressure"
- Door to provider - a BIG metric these days. The faster you see the patient and the faster you put in orders, the faster things will be done
- Order to Result of the LAST test - this essentially dictates the length of your ED time and we constantly work with our radiology and clinical laboratory colleagues to drive down turnaround times
- Door to Dispo - WHEN we consult (early versus waiting on test results) and how long those consults take to complete has a huge impact on our overall ED stays
- Coordinate outpatient care more effectively
- Use our resources more wisely
- Decrease our admissions
- Why do we admit patients?
- They might die...
- They need some intervention only available as an inpatient
- To facilitate an otherwise outpatient workup where outpatient follow-up is not possible due to resources, patient reliability, access to care, etc...
- How can we avoid admitting patients?
- Continue using our ED based observation unit (Clinical Decision Unit)
- Discussing outpatient care with their PCP
- Working with the system to develop methods of efficient and reliable outpatient follow-up for select patients and conditions. Watch this space for exciting new opportunities!
- Why do we admit patients?
- The bottom line is that we are the guardians of the front door. We cannot control the back door of the hospital, but we can optimize our workflows to help the entire system.
PEPTIC ULCER DISEASE WITH DR. MURPHY
- There are 500,000 new cases of PUD every year which translates to $10 billion in direct and indirect costs.
- The two main causes of PUD are H. Pylori (48%) and NSAIDs (24%).
- H Pylori leads to symptoms in two main ways based on the colonization pattern.
- Pan-gastritis results in atrophy of the stomach epithelium leading to gastric ulcers and gastric cancers.
- Antral-predominant gastritis results in increased gastrin and acid production leading to duodenal ulcers.
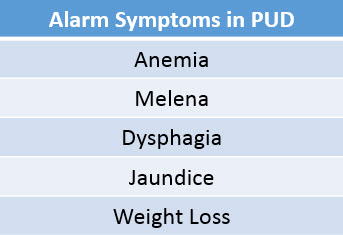
- Alarm symptoms necessitate endoscopy to ensure no complications.
- Complications of PUD include bleeding, gastric outlet obstruction, and perforation.
- Management for these conditions is mainly supportive in the ED with endoscopy or surgery being definitive therapy.
- Uncomplicated PUD is treated with a test and treat strategy if prevalence of H Pylori is > 10%.
- In the ED multiple studies have shown our prevalence is over 10% but at this time we have no point of care H Pylori testing at UC. Therefore, management of these uncomplicated patients involves PPI trial for four weeks and follow up with their PCP or GI.
Pediatric Trauma with Dr. Hoehn
This is a discussion of minor head trauma, blunt abdominal trauma and nonaccidental trauma
The recommendations here do NOT apply to major intracranial injury (GCS <14), unstable or multisystem trauma, penetrating trauma or medical indications for imaging
Minor Head Trauma
Infant Glasgow coma score
PECARN TBI Study
- Prospective colors of patients under 18
- Derived and validated clinical decision rule to determine who is very low risk for clinically important brain injury
- Defined clinically important brain injury as a TBI on CT that required intervention (neurosurgery or intubation for over 24 hours) or close observation (admission over 48 hours) or death
- Inclusion
- Children <18 yo with head trauma in the past 24 hours
- Exclusion
- Trivial injury mechanisms AND no signs or symptoms of head trauma
- Penetrating trauma
- GCS <14 (see infant GCS score chart above)
- Known brain tumors or neurological disorders
- Inclusion
There are two different decision rules depending on the age of the patient (<2 years and > 2 years)
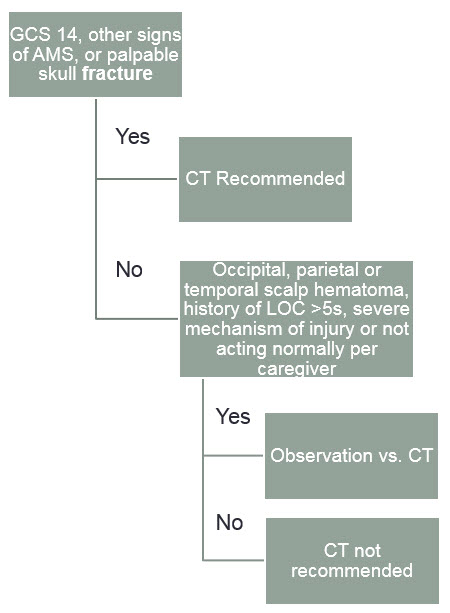
<2 years of age
decision algorithm for age <2
- The 6 factors in the decision rule are:
- Altered mental status
- Presence of a non-frontal hematoma
- LOC greater than 5 seconds
- Severe mechanism of injury
- Palpable or unclear skull fracture
- Not acting normally per caregiver
- If the patient has none of the above, they have a 0.6% risk of cTBI
- Sensitivity: 100%
- Specificity: 53.6%
- NPV: 100%
- PPV: 2.4%
- In the decision algorithm shown here, patients in the "observation vs. CT" group have a 0.9% risk of cTBI compared to <0.02% in the "CT not recommended" group
>2 years of age
decision algorithm for age >2
- The 6 factors in the decision rule are:
- Altered mental status
- LOC >5s
- History of vomiting
- Clinical signs of basilar skull fracture
- Severe mechanism of injury
- Severe headache
- If the patient has none of the above, they have a 1.1% risk of cTBI
- Sensitivity: 96.8%
- Specificity: 58.2%
- NPV: 99.5%
- PPV: 2.2%
- In the decision algorithm shown here, patients in the "observation vs. CT" group have a 0.8% risk of cTBI compared to <0.05% in the "CT not recommended" group
- "Observation" is considered observing the patient up to 4hrs after the injury
Blunt Abdominal Trauma
- We also have a decision rule to help us decide who we do not need to scan with blunt abdominal trauma
- "Identifying Children at Very Low Risk of Clinically Important Blunt Abdominal Injuries" by the PECARN research group
- A study of over 12,000 patients undergoing evaluation for intra-abdominal injury (IAI)
- It involves 7 factors:
- Seatbelt sign
- GCS <14
- Abdominal tenderness
- Evidence of thoracic wall tenderness
- Complaint of abdominal pain
- Absent or decreased breath sounds
- Vomiting
- The highest risk factors were ecchymosis, bruising or a seatbelt sign and GCS<14
- If none of these risk factors were present, the risk of IAI was 0.1% and CT is not recommended
- Again, this is designed to tell you who not to scan, not who you need to scan
- Sensitivity: 95%, Specificity: 37%
- What is the utility of screening labs in children with blunt abdominal trauma?
- "The role of elevated transaminase levels in children with blunt abdominal trauma"
- Prospective review of 87 children with blunt abdominal trauma
- Divided them into three groups:
- No signs of abdominal truma
- Signs of abdominal trauma without radiographically detected injury
- Intra-abdominal injury detected on CT
- Looked for rates of elevated AST and ALT in those with intra-abdominal injury compared to the other groups
- In the IAI group, the average AST was >119 and ALT was > 65
- If AST >110 and ALT >65, sensitivity was 92% and NPV 96%
- Authors recommend getting CT if AST > 200 and ALT >100
- Study had a small N, but did reach statistical significance
- "Liver Function Tests in Children with Blunt Abdominal Traumas"
- 115 patients, 16 with liver injury
- Average AST/ALT in injury group was 474 and 442
- "Blunt Abdominal Trauma In Children: How Predictive is ALT for Injury?"
- Compared liver injury ro other IAI
- 51 patients with liver injury, 65 patients with other IAI
- ALT > 104 was 96% sensitive and 80% specific for liver injury
- "The role of elevated transaminase levels in children with blunt abdominal trauma"