Grand Rounds Summary 12.7.16
/R4 Case Follow Up with Dr. Richardson
Elderly patient arrived by ambulance for abdominal pain, also complaining of constipation and rectal pain. Multiple recent ED visits for constipation. Attempts at manual disimpaction at home have been unsuccessful. History of previous CVA with residual left hemiparesis as well as current IVIG treatment for Guillain-Barré. Examination is unremarkable, noted to have soft stool in rectal vault.
Constipation
- Why should we care?
- 700k annual ED visits
- 1.6 billion dollars in health care costs per year
- Functional constipation
- at least 25% of BM involve
- straining
- lumpy/hard stools
- incomplete evacuation
- manual assistance
- at least 25% of BM involve
- ED approach to constipation
- Is it just constipation?
- What’s the problem, and how much can we solve right now?
- How do we keep this from happening again?
- Discharge
- Can’t miss on the differential:
- Bowel obstruction/volvulus
- IBD with toxic megacolon
- Colorectal cancer
- Cauda equina syndrome
- and more...
- Etiology
- Consider thinking about constipation like heart failure (preload/afterload)
- Preload
- Stool quantity, consistency
- Motility (contractility)
- medications
- autonomics
- endocrine/metabolic
- Outlet obstruction (afterload)
- Fissures
- Abscess
- Mass
- Impaction
- Preload
- Consider thinking about constipation like heart failure (preload/afterload)
- Therapeutic options
- Bulking agents
- dietary fiber/psylium
- Patient needs to drink lots of water to make this effective
- dietary fiber/psylium
- Surfactants (docusate)
- Lubricant (minderal oil, vaseline)
- Osmotic (magnesium citrate, lactulose, miralax)
- Stimulant (senna, dulcolax)
- suppository (glycerin, dulcolax)
- Enema (saline, fleet’s soap suds, etc)
- Bulking agents
- Advanced therapeutics
- Peripheral mu receptor antagonists (methylnaltrexone)
- can administer 2 mg of naloxone via PO route to help with opioid related constipation, bioavailability PO is 2%, unlikely to promote systemic withdrawal
- Peripheral mu receptor antagonists (methylnaltrexone)
- Disimpaction: It’s a process
- Step 1: manual disimpaction if needed
- Get a commode in the room
- Patient in lateral decubitus position
- PPE and plenty of chucks
- Consider versed
- Lubrication and/or viscous lidocaine
- Goal is to break up stool
- Step 2: Enema
- Step 3: “Clean Out”
- One reason you see children admitted for constipation
- Completes bowel evacuation
- Osmotic laxatives
- Miralax 1.5 mg/kg (2 cap TID x 3 days)
- Mag citrate
- Stimulant laxatives
- Senna 30 mg BID x 3 days
- Step 1: manual disimpaction if needed
CPC with Drs. Bernardoni and Loftus
Patient is a young male with history of recent diagnosis of syphilis presents to ED with one month of alopecia and rash. Recent azithromycin prescription for reported possible viral URI. Seen at outside hospital for same, noted to have low white blood cell count, negative HIV antigen antibody test and positive T palladium test, Hyperpigmented macular rash of hands, feet, and face, physical examination otherwise unremarkable. Tachycardia to 120, BP 150/87, otherwise normal vital signs. WBC of 2.2 in our ED, some mild elevation of AST/ALT/lipase, positive syphilis, CXR unremarkable except for mild cardiomegaly, EKG with sinus tachycardia and 1st degree AV block.
A diagnostic test was ordered…
ANA screen returned positive.
RPR testing inpatient was negative, possible false positive T palladium testing from SLE.
Systemic Lupus Erythematosis (SLE)
- Prevalence: 20-150/100,000
- Predominance for women of child bearing age, gender gap narrows in elderly
- Symptoms are often very non-specific
- ED workup
- History and physical
- Renal, CBC, UA, ?LFT/troponin
- Consider ANA testing if clinically suspicious for new lupus diagnosis
- Run every 48 hours, not reliably returning during ED visit
- High prevalence of chronic pain/fibromyalgia dx
- Psychiatric disease common
- Things not to miss when considering SLE:
- Infection
- Evaluating for SLE flare vs infection
- Steroid therapy + fever = infection until proven otherwise
- Consider procalcitonin to help clarify, good specificity in this scenario
- Consider steroids for lupus flare but also consider stress dose steroids if concerned for infection
- Evaluating for SLE flare vs infection
- Chest pain
- higher risk for coronary events
- considered possibly due to significantly higher coronary calcification burden at younger age
- Libman-Sacks endocarditis
- 1/10 SLE patients, often without symptoms
- often diagnosed after consequences from embolic phenomena
- higher risk for CVA
- Treatment with anticoagulation and valve repair when indicated
- Pericarditis, pleuritis, costochondritis
- NSAIDs if renal function permits
- Prednisone 0.5-1 mg/kg/day
- Myocarditis
- higher risk for coronary events
- Neurologic
- Stroke in up to 19% of SLE patients
- TIA most common
- Dural venous sinus thrombosis
- Meningitis
- SLE LP: baseline elevated protein and lymphocytic pleocytosis
- CNS vasculitis: fever, severe HA, confusion progressing to psychotic symptoms and seizures
- Treat with steroids
- Stroke in up to 19% of SLE patients
- Pulmonary
- Acute lupus pneumonitis, similar to ARDS
- Treatment with methylprednisolone 1g/day x 3 days, broad spectrum antibiotics
- Acute lupus pneumonitis, similar to ARDS
- Infection
R1 Clinical Diagnostics with Dr. Jarrell: Laboratory studies in Chronic Liver Disease (CLD)
Take a minute to review Dr. Jarrell's full review here
Ultrasound Grand Rounds with Dr. Carleton: Ultrasound guided regional anesthesia of the lower extremity
- Indications
- acute pain management of lower extremity injuries
- anesthesia for procedures
- alternative to procedural sedation/narcotic usage
- Maximizing safety
- Pre-procedural assessment of nerve function
- “Bomb-proof” knowledge of local anatomy
- Constant visualization of needle tip
- Constant visualization of injection
- Knowledge to recognize and treat local anesthetic systemic toxicity (LAST)
- Rationale
- Analgesia in the ED is notoriously underdosed and often omitted
- Observational studies in regional anesthesia showing significant reduction in pain as well as reduction in narcotic requirements
- Anatomy and sensory innervation
- Lateral femoral cutaneous nerve
- cutaneous innervation of lateral thigh
- Obturator nerve
- cutaneous innervation of medial thigh
- Intracapsular femur
- derives some sensation from sciatic nerve
- may be missed with femoral nerve block
- derives some sensation from sciatic nerve
- Fascial landmarks
- Fascia lata
- covers all musculature of anterior thigh
- seen as echogenic line on ultrasound
- Fascia iliaca
- lies on surface of iliacus musculature
- injection of anesthetic between these two fascial layers will include nerve blockade, however, great vessels are deep to this layer, providing some protection from LAST if superficial nerve blockade is all that is needed
- For proximal nerve blockade of femoral nerve injection may be placed just cranial to position where femoral artery divides into profounda femoris and superficial femoral artery
- Lateral circumflex femoral artery arises directly from common femoral artery in 20% of population, crosses laterally and superficial to femoral nerve. Important to identify with ultrasound approach
- Always interrogate intended needle path and injection area with doppler
- Fascia lata
- Ultrasound points
- Ultrasound beam must be perpendicular to nerve to maintain its appearance, can lose view of nerve if tilted rostral or caudal
- Room set up
- Position patient supine
- Ultrasound machine on opposite side of the bed
- Ultrasound probe in non-dominant hand
- Mayo stand to operator’s dominant side
- Prep area sterile, sterile probe cover, sterile towels
- Equipment and preparation
- Local anesthesia and skin wheal
- 22 gauge 3.5 inch spinal needle (whitacre vs standard) +/- injection tubing
- benefits of standard needle include more likely to feel “pop” when passing through fascia
- 10-40 mL of local anesthetic
- keep in mind that bupivacaine has association with higher incidence of LAST
- Which block?
- Femoral nerve block
- isolates femur
- “3 in 1” block
- targeting entire thigh
- Femoral nerve block
- Post-injection pressure
- Caudal compression 1-2 cm below injection site for 5 minutes facilitates upward spread of anesthesia to targeted structures
- Lateral femoral cutaneous nerve
- Compartment syndrome and regional anesthesia
- Systematic review of relevant literature up to 2014
- found 2 prospective articles that looked in to this, no cases of compartment syndrome
- “no clear recommendations exist regarding the use of RA for adults with orthopedic extremity procedures at risk for developing compartment syndrome”
- Systematic review of relevant literature up to 2014
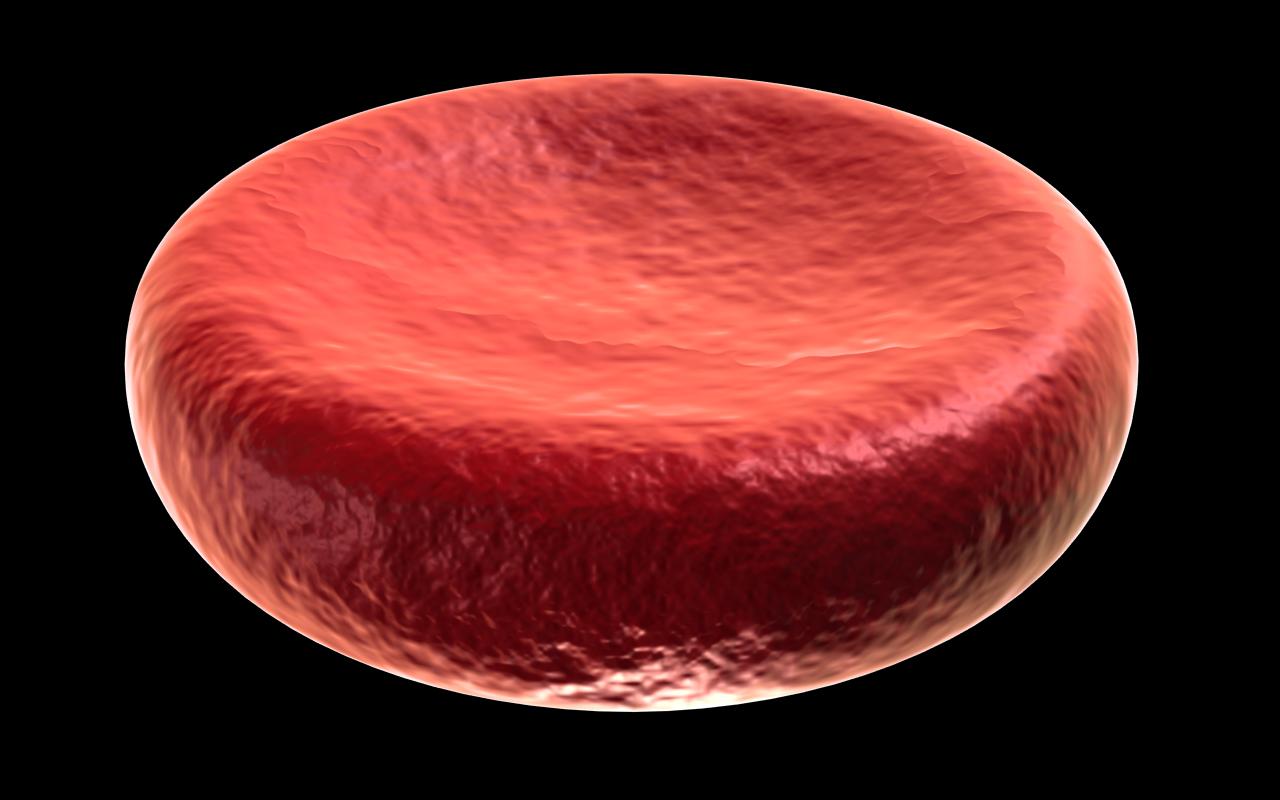
R1 Clinical Knowledge - Adult Non-Hemorrhagic Anemia with Dr. Klaszky
- Signs and symptoms of anemia caused by either direct tissue hypoxia or the body’s attempts to compensate for this hypoxia
- What’s included in the CBC?
- Hemoglobin
- Hematocrit (fraction of volume of blood that is occupied by red blood cells)
- Mean corpuscular volume (MCV)
- Useful in classification of anemia
- Normocytic (80-100 fL)
- Microcytic (<80 fL)
- Macrocytic (>100 fL)
- Red cell distribution width
- correlated with poor clinical outcomes when abnormal
- Haptoglobin
- decreased in hemolytic anemia
- lactate dehydrogenase (LDH)
- surrogate marker for hemolysis
- Classification of anemia
- Decreased RBC production
- iron deficiency
- nutrition deficiency
- medication induced
- etc
- Increased RBC destruction
- sickle cell disease
- RBC membrane disorders
- enzyme defects
- microangiopathic
- infectious
- Decreased RBC production
- Sickle cell anemia
- patent presentation
- often with vaso-occlusive pain crisis
- Acute stressor induces increased sickling
- dehydration
- acidosis
- infection
- hypoxia
- cold temperatures
- Acute stressor induces increased sickling
- life threatening
- acute chest syndrome
- aplastic crisis
- stroke
- sepsis/infection
- splenic sequestration
- often with vaso-occlusive pain crisis
- patent presentation
- Iron deficiency anemia
- Decreased serum iron level, decreased ferritin, and increased TIBC
- Consider GI referral for chronic GI blood loss
- Chronic kidney disease
- Kidneys are major producers of erythropoietin (EPO)
- Decreased reticulocyte count, increased serum iron and ferritin, decreased TIBC
- Goal hemoglobin of 10-12
- must replete iron status if deficient prior to administration of EPO for it to be effective