Grand Rounds Summary 01.11.2017
/Taming the SRU with Dr. Shah
Transfer for stroke post TPA presents bradycardic, hypoxic, and normotensive. Agitated with a L hemiplegia initially but then goes unresponsive in CT scanner. After intubation, CXR shows wide mediastinum and the patient ultimately is diagnosed with an aortic dissection.
Aortic Dissection: Clinical Features
- Tend to be male, older (>63)
- 72% present with chest pain
- 50% tearing or ripping pain
- 5% of the time people present with stroke symptoms
Aortic Dissection: Diagnostics
- CT
- Sens: 83-100%
- Spec: 87-100%
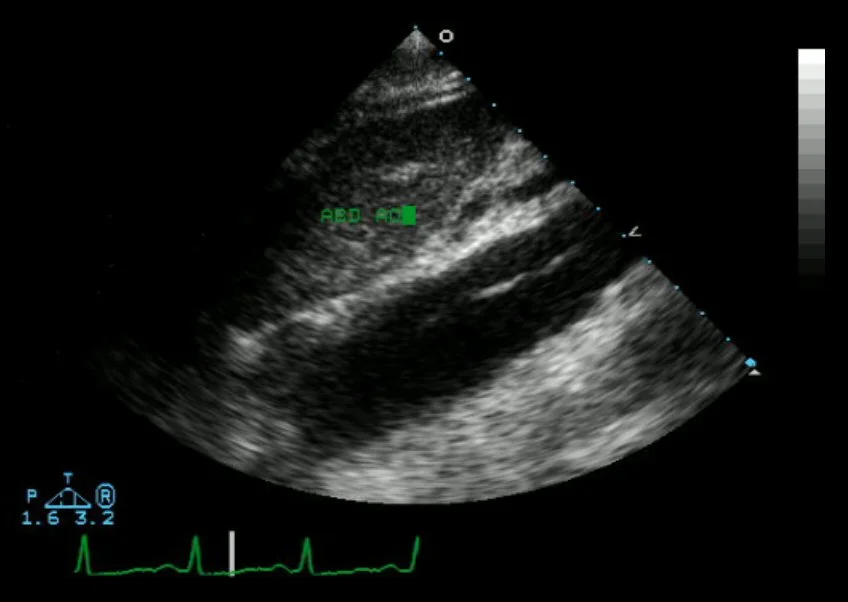
- TEE
- Sens: 100%
- Spec: ~95%
- TTE
- Sens: 77-80%
- Spec: 93-96%
- For ascending aorta only
- In hands of experienced operators
- Suprasternal view: put the US in the juglar notch, aim down
TPA: Pharmacokinetics
- Thrombolysis starts around t=30min
- Peak effect at t=60min
- Can effect coagulation cascade for up to 24h
TPA reversal: TXA the most beneficial of the factor complexes, no benefit to FVIIa alone
Consider FFP, platelets, or cryoprecipitate to replace your coagulation factors to reverse TPA (no good data for any of them).
CPQE: Acute Heart Failure with Drs. Harrison and Murphy
Acute Heart Failure (AHF): gradual or rapid deterioration in heart failure symptoms. EF 45-50% constitutes a reduced EF.
ED therapeutic and disposition decisions affect morbidity, mortality, and costs.
1 million ED visits/year for AHF
- 80% admitted
- 10% mortality after discharge for an admission for heart failure
Triggers of Acute Heart Failure
- HTN
- ACS
- Arrhythmias
- Infections
- Renal dysfunction
- Non-adherence
- Medications
Amplifying mechanisms of Acute Heart Failure
- Myocardial
- Renal
- Vascular
- Neuroendocrine
Diagnosis of Acute Heart Failure
- Hx of HF: +LR 2-5.8
- Dyspnea is most common symptom
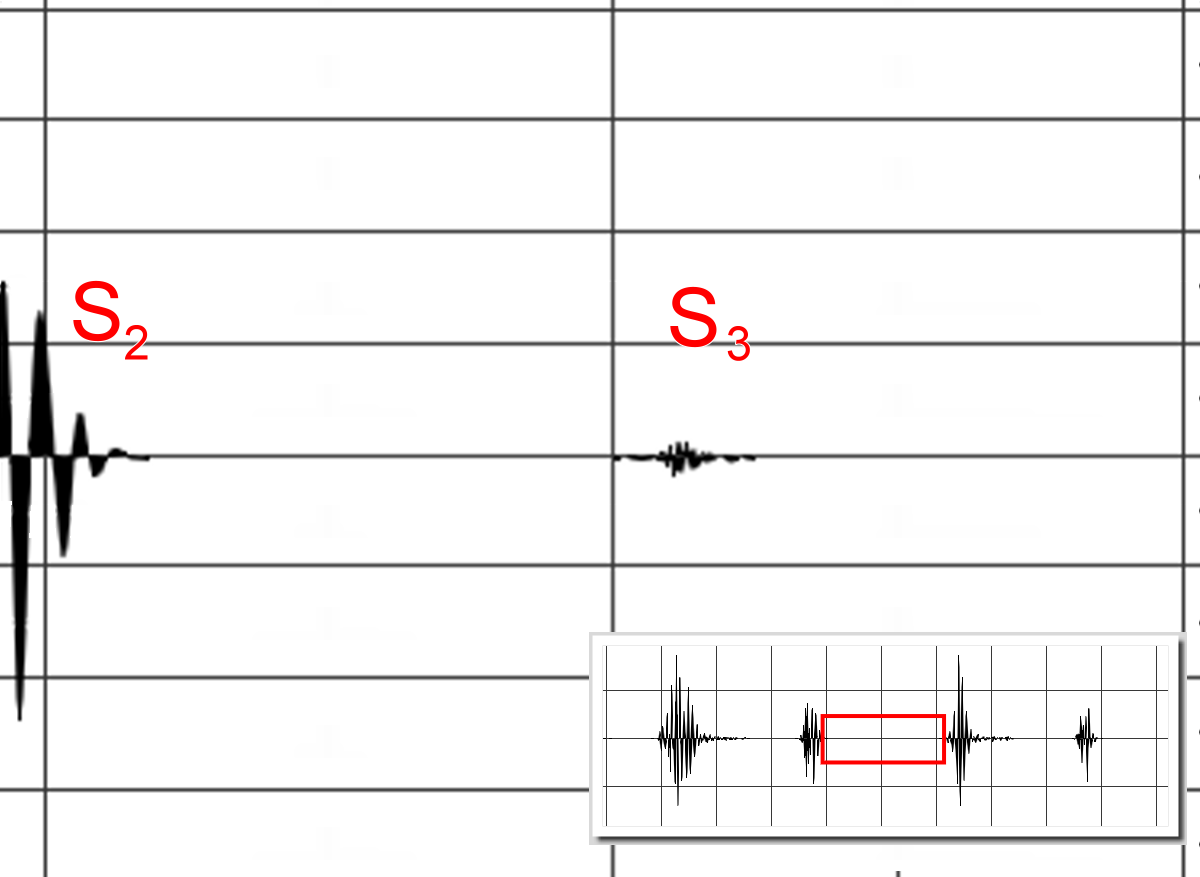
- S3 (98% specific), JVD most specific sign
- Clinical gestalt based on H&P had +LR 4.4
- New renal failure has high +LR
- ECG: not diagnostic in HF, may reveal etiology, associated comorbidities
- CXR: 20% may be normal in AHF
- Pulmonary Edema: +LR 4.8
- Cardiomegaly not sensitive or specfic
- BNP:
- <100: 93.5% sensitive, not specific (53%)
- >500: less sensitive but 89% specific
- Renal insufficiency increases BNP & NT-proBNP
- Age increases BNP<NT-proBNP
- BMI decreases both
- PE & PHTN decreases both
- EF decreases both
- HFpEF have lower BNP elevation than HFrEF
- changes >25-50% from baseline generally clinically significant
- Lung US
- >=3 B-lines in 2 bilateral lung zones
- +LR 7
- -LR 0.16
- +LR 7
- >=3 B-lines in 2 bilateral lung zones
Respiratory Distress? NIPPV
- Prospective RCT
- CPAP vs Bilevel vs Non-invasive face mask
- No mortality benefit
- NIPPV had symptomatic benefits
- Meta analysis did find mortality benefit in NIPPV
HTN >160: likely the HFpEF patients
- Nitrates: 0.4mg SLx3, q5min then to Nitro gtt (consider higher dosage when starting the gtt)
- Evidence for above: no mortality benefit, improves symptoms
- Diuretics
- If systemically volume overloaded: give 1-2x oral home dose via IV
Normotensive Patient: typically HFrEF
- Diuretics
- Compared low and high dose, along with Q12h bolus v gtt
- No significant differences between group
- trend towards increased symptomatic improvement with high dose group
- trend towards worsening renal function in high dose group
Hypotensive Patient: <90 HFrEF
- Inotropes
- Milrinone: phosphodiesterase inhibitor
- No change in mortality in patients who got milrinone
- Dobutamine: B-agonist
- No change in mortality in patients who got dobutamine
- Milrinone: phosphodiesterase inhibitor
Risk Stratification: 80% admission rates, some regional variation
- What is high risk?
- Lower SBP associated with increased mortality
- Lower admission Na+ associated with increased mortality and length of stay
- BUN and Cr associated with increased in-hospital mortality
- Cr >2.75 and BUN >43 in one study
- Elevated troponin found to have increased mortality
- 8% v 2.7%
- Many AHF patients will have troponin elevations, most of them are not due to ACS
- Do all need to be admitted? If near baseline or downtrending, we may be able to observe these patients with low level troponins in the future
- What is Low Risk? AHF is a high risk population at baseline: 5-10% 30 day mortality. Impossible to get to 1% risk
- Emergency Heart Failure Mortality Risk Grade (EHMRG)
- Ottawa Heart Failure Risk Scale
- Adequate response to therapy
- If barriers to self care, consider admission
- Health Literacy
- Social Support
- Follow-up
Observation Medicine: decreases admissions and ED re-vists
R4 Clinical Soapbox: Hypertension in the ED with Dr. Winders
30% of adults have HTN
#1 risk factor for stroke, heart disease, and heart failure
Case: 45yo male with BP 165/90
- Can we diagnose HTN in the ED? Technically, no
- What are the odds this patient has HTN? 75% of asymptomatic patients with 2 BP >140/90 in the ED were still hypertensive 2 weeks later
- Use the EMR to find old BPs as this can solidify your diagnosis and justify treatment
- Any isolated BP >180/110 is diagnostic of HTN
- Does the patient need a workup? Level C recommendation. ACEP clinical policy:
- In ED patients with asymptomatic markedly elevated blood pressure, routine screening of acute target organ injury is not required
- In select patient populations (poor follow-up) screening for elevated serum creatinine level may identify kidney injury that affects disposition
- 30/180 in one study with asymptomatic HTN had abnormalities on their renal panel
HTN secondary to pain? No evidence that pain or anxiety is a driver of elevated BP
Ophthalmology with Dr. Jarrell
2 million ophtho related ED visits per year, 1.5% of total ED visits. 97% treated and discharged from the ED
Vital Signs of the Eyes:
- Visual Acuity
- Pupillary Exam
- IOP
- Visual Fields
- EOM
Acute Angle Closure Glaucoma:
- Presentation: Headache, nausea, vomiting, decreased vision, severe eye pain
- Exam: Conjunctival redness, corneal edema or cloudiness, shallow anterior chamber,
- Diagnosis: IOP, gonioscopy; ocular US?
- Management: timolol, acetamolamide, tropicamide
Conjunctivitis:
- Viral treatment: nothing
- Bacterial treatment: erythromycin ointment (cipro if contact lens wearer for pseudomonas coverage)
- Allergic treatment: systemic antihistamines
- Immunogenic treatment: treat underlying autoimmune disorder
Open globe
- Presentation: traumatic mechanism, decreased vision
- Exam: decreased VA, relative APD, eccentric or teardrop pupil, increased/decreased anterior chamber depth, extrusion of vitreous
- Diagnosis: Seidel's sign, CT orbits, ophthalmology consultation
- Management: NPO, ketamine relatively contraindicated, no drops, pain control, OR, and antibiotics
- Prognosis: blunt mechanism, VA: hand movement or worse, relative APD, posterior wound defect
Corneal Foreign Bodies & Corneal abrasions
Removing the foreign body:
- Topical anesthesia
- Remove FB (if present)
- Cotton swab
- 18g/30g needle
- Burr
- Sweep lids
- Fluorescein exam
- Oral analgesia, cycloplegia for comfort
- Topical abx
- Patch? do not patch contact lens wearer
- Ophtho follow-up in 2-3 days, 24h hours if FB or rust ring still present
Orbital Cellulitis
- Presentation: Proptosis, pain with EOM
- Complications: thrombophlebitis, CRAO, brain abscess
- Exam: proptosis, decreased EOM, pain with EOM, double vision decreased VA, edema be
- Diagnosis: CT ocular with IV contrast
- Management: surgery, IV antibiotic
Retinal Detachment:
- Presentation: increased flashes or floaters preceding painless loss of vision,
- Exam: decreased VA, may have abnormal red reflex, reduced visual fields
- Diagnosis: ophthalmology consult, US could be helpful
- Management: surgical
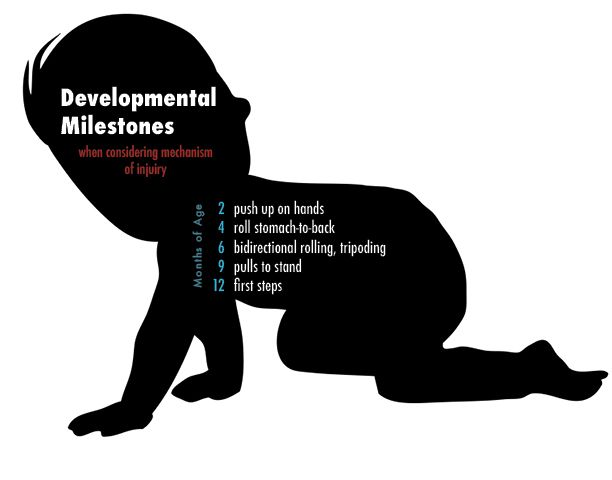
EM-Peds Combined Conference: Non-accidental Trauma
Physical Exam: things that should alert you to NAT
- Torn frenulum
- Palatal Petechiae
- Dip injuries
- Circular burns
- Patterned bruises or burns
- Bruising on the ears
- Bucket Handle Fx, Rib fx always concerning
In a simulation study that looked at 4 cases, 2 accidental and 2 abuse, with experienced practitioners, only 60% of the time did they make the correct diagnosis.
Incorrect Diagnoses:
- Accident vs Abuse: OR 8.8 of making an incorrect diagnoses
- Accident: High Risk Social History or Low Risk Social History OR 8.8 of making an incorrect diagnoses
- When they got it wrong, it was because they thought:
- Injury inconsistent with mechanism
- Social risk factors
- Changing history
How much are kids bruising at baseline?
- <5mo prevalence of bruising 1.3%
- Trauma chief complaints 15x more likely in kids who are bruised
- >5mo prevalence of bruising 6.4%
- Location of bruising on the chest, back & buttocks, ears and neck were predictive of NAT
Ask yourself the following questions: 97% sensitive and 84% specific for predicting NAT
- Bruising the TEN region of a child <4yo?
- Bruising in any region of an infant <4mo ?
- Confirmed accident in a public setting to explain the bruising in the TEN region or any bruising in the infant?
Utility of hepatic transaminases in children with concern for abuse:
- AST/ALT
- Sensitivity 83.8%
- Specificity 83.1%
- Lipase
- Sensitivity 61.5%
- Specificity 79.2%
R1 Diagnostics: Paracentesis & Thoracentesis with Dr. Klaszky
Check out Dr. Klaszky's in-depth post here.