Grand Rounds Recap - 3/18/15
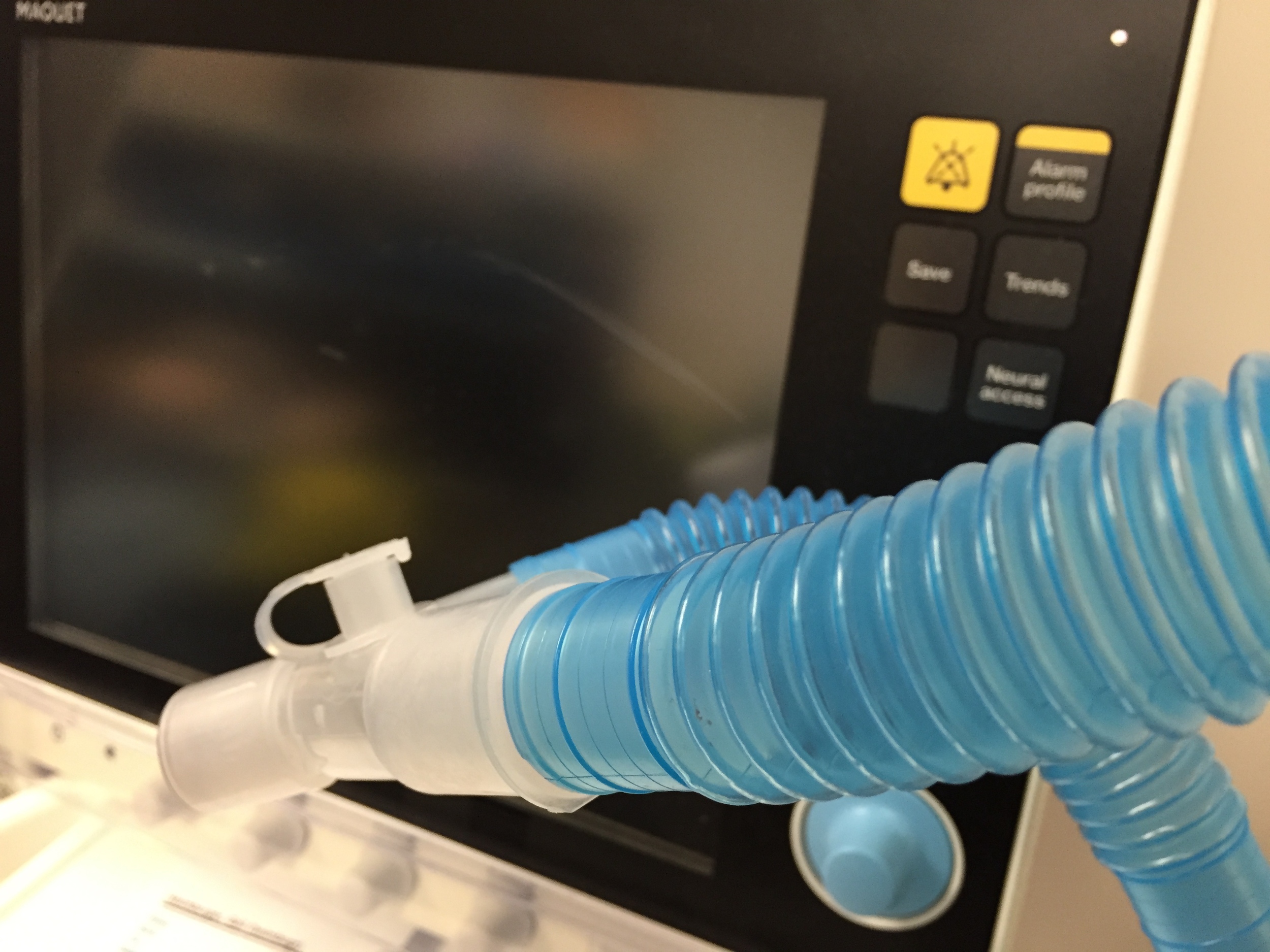
/Evidence-Based Emergency Medicine: Vent Management with Drs. Axelson & Scupp
The term Acute Lung Injury (ALI) is being phased out and instead Acute Respiratory Distress Syndrome (ARDS) is now graded mild, moderate, and severe depending on the PaO2:FiO2 ratio
The median onset of ARDS after presentation to the ED was 2 day but could be anywhere from 5 hours to 5 days
ARDS Net was a foundational trial in ventilator management and was a triall of tidal volume and plateau pressures. The primary end point, mortality, was reduced by >20% when folks were on a low TV (6cc/kg) and lower PP (25-30 mm Hg).
- Even in patients that got intubated for reasons other than lung injury, a low TV strategy significantly reduced the progression to ARDS and mortality
Low tidal volume strategy protects the lungs and thus protects the patient, tape measures are now carried on every airway cart - use them to calculate the correct TV for patients
A single recorded episode of hyperoxia (PaO2 on ABG >300) has been associated with increased mortality in a variety of patients including TBI, stroke, and post-ROSC patients)
- Titrate your FiO2 to a SaO2 of 95-98% as quickly as possible
- Use PEEP to help minimize FiO2. PEEP tables are now on all of the airway carts to help better match PEEP with FiO2 use.
Be mindful of your ventilated patients, studies have consistently demonstrated "treatment momentum" in the ventilated patients meaning that what they get put on initially in the ED does not change often until they get to the ICU and in some cases even 24 hours into their ICU course were still on the same initial settings
Status Epilepticus with Dr. Foreman
Status epilepticus is defined as seizure activity for greater than 5 minutes or a lack of return to baseline between seizures.
Status is associated with a huge cost to the health care system (~$4 billion) and carries a 15-22% mortality rate. The most common precipitant for status is a patient with history of seizures who for one reason of another have subtherapeutic levels of their anti-epileptic medications.
Benzodiazepines are first line treatment for seizure/status and patients should receive at least 2 doses of versed or ativan before second line agents.
- Second line agents include phenytoin, valproate, and keppra. There is no agreed upon agent as the best and the new ESETT study will hopefully help better determine this.
- If patients continue to be in status despite these agents consider benzodiazepine or propofol drips but they will need their airways secured prior to starting these medications.
Have a high degree of suspicion of Non-Convulsive Status Epilepticus (NCSE) in the patient that remains comatose after a seizure and seriously consider continuous EEG in the patient who has no change in their mental status after 20 minutes and has not returned to baseline in 60 minutes after their seizure.
Soft Tissue Neck Radiology with Dr. Renne
Use the acronym CHESS to assess a soft tissue neck film fully:
- C- Confirm Adequacy (shot during end inspiration and with neck extended)
- H- Hypopharynx
- E- Epiglottis
- S- Subglottius
- S- Spine
Indications to get a soft tissue neck x-ray include foreign body localization, croup, epiglottitis, and RPA
When assessing for an RPA, assess the pre-vertebral spaces to determine if they are enlarged, at C1-3 the space is enlarged if it measures >50% of the vertebral body and from C4-T1 if it is >100%.
A lateral neck x-ray is >90% sensitive and specific for croup and will have a large hypopharynx with a small subglottic space
The relative rates of epiglottitis are increasing in adults due to waning H. flu immunity from vaccination, but classically a soft tissue neck will be adequate to assess for this if it is truly an upright. The epiglottis will look enlarged and ragged in epiglottitis on a soft tissue neck film and is often referred to as a "fingerprint sign"
While many foreign bodies in the pharynx end up being radiolucent if someone has dysphonia and/or subcutaneous gas on x-ray be highly suspicion for FB
Big Data in Health Care with Dr. Yamin
Rapid e-health record adoption has lead to increased amount of clinical data. Costs in the US are still rising, in some cases 2x that of other developed nations. The impending question is if reforms using big data can curb costs.
Big data, while a buzzword relates to the volume of data, the velocity of which the data is coming, and the variety of data sources it can be pulled from. Tons of other industries use it to help improve their business including Amazon and baseball (i.e. Moneyball). Big data may help identify and manage: high cost patients, readmissions, adverse events, triage, and multi-system disease management
Challenges of Big Data include: FDA regulations, making free text usable data, improving clinical decision support, and avoidance of alarm fatigue
Social Determinants of Health with Drs. Axelson & Stull
In the US today, EM is often on the first line of every form of prevention:
- Tertiary prevention (i.e. treating disease once it manifests)
- Secondary prevention (i.e. screening for disease before it manifests)
- Primary prevention (i.e. providing guidance/treatment to prevent disease)
However, the social determinants of health are the key that can put certain patients and population at greater risk for worse outcomes related to their illness. Examples of social determinants of health include education level, literacy, income, gender, race, and access to care, housing, and transportation
These issues are systematic, notoriously difficult to address, and can significant affect a patients presentation, adherence to treatment, treatment efficacy, and utilization of the ED as a source for care
We as physicians are responsible to at least in part address social determinants of health that are affecting out patients care even in the ED (according to our local survey >85% of our faculty/residents agree). Being aware that social determinants of health exist is the first step to addressing them, but as with everything in EM, we have to get creative to provide our patients the best care we can
Consider getting to know local community resources that you can actually recommend to patients as merely a referral to social work will not always address the problem. Patients with housing, especially those with psychiatric illness and/or substance abuse, utilize EMS and the ED significantly less than those without it. Lacking health literacy is more common than we think and can lead to significant recidivism
New discharge dot phrases will soon be rolled out to help provide suggested resources for access to housing and transportation and standard discharge instructions template written at a 5th grade level