Grand Rounds Recap 8.17.2016
/Air Care Grand Rounds
Air Care Simulation
The Case: You're called to the scene of a 50 yo F, helmeted motorcyclist who rear ended a pick-up truck on the freeway and was found underneath the truck. She has a GCS of 14, vitals consistent with shock with HR in the 130s and BP 63/29. On initial assessment there is a make-shift tourniquet made out of a belt on her left thigh with ongoing arterial bleeding. Both lower extremities, her left upper, and her right forearm are mangled and she does not have IV access yet. What is your first step?
Key Points:
- Hemorrhage control: place a tourniquet to stop arterial bleeding. Ideally you or the flight RN can do this while the other focuses on assessment of ABCs.
- Access: very limited in this patient due to extremity trauma. Intraosseous lines are a quick go-to in cases where traditional IV access may be limited.
- Resuscitation: Blood products and TXA (if a second line can be established).
- Assess for pelvic stability. This patient had a grossly unstable pelvis and in the setting of shock a T-pod should be placed prior to transport.
epoc® Blood Testing
Blood testing device now carried on AirCare which allows us to obtain a lot of information from a small sample of blood including: H/H, Blood Gases, Electrolytes, Creatinine. Key considerations: may be particularly useful in longer flights or ICU-to-ICU transfers for vent monitoring, electrolyte considerations (hyperkalemia), concerns for bleeding.
"Super Sucker"
Robust suction device located behind the MD seat in the aircraft. Two suction attachments available including a typical yankauer and a large suction device for particularly high volume needs. Consider if you know you're going to be managing a bloody or emesis filled airway.
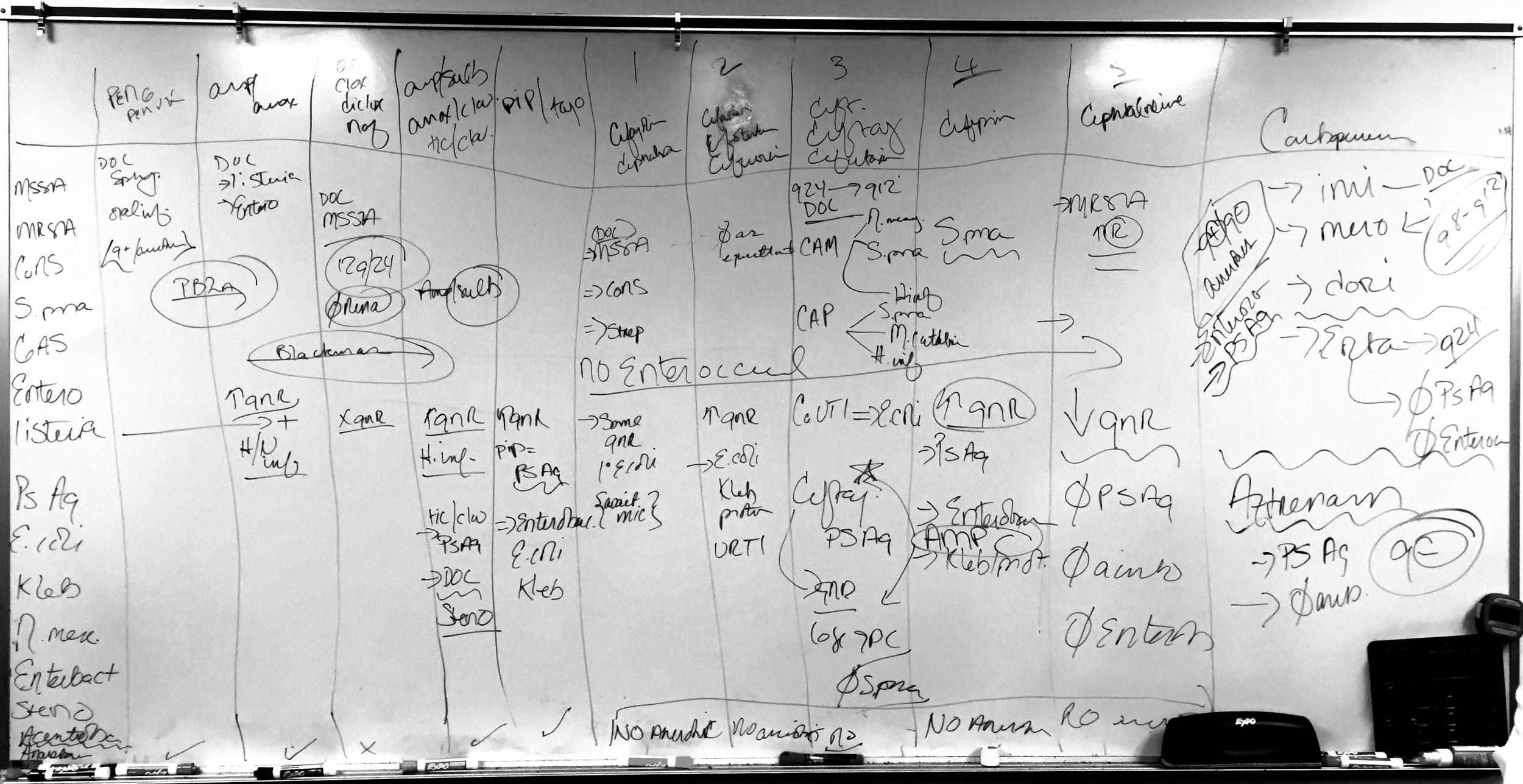
Antibiotic Chalk Talk: Beta Lactams with Dr. Renee Hebbeler-Clark
Beta Lactams
- How they work: Time dependent killing (not concentration dependent)
- Pencillins
- Penicillin/PenVK
- Syphilis
- Great for oral or dental infections because it has good gram positive and anaerobic coverage
- Penicillin/PenVK
Resistance Mechanism: Pencillin Binding Proteins
- Ampicillin and Amoxicillin
- Better gram negative coverage and includes anaerobic coverage as well
- Listeria
- Drug of choice for enterococci (both vancomycin resistant (about 75% are still amp susceptible!) and vancomycin susceptible)
- Oxacillin/Dicloxacillin/Nafcillin (Semi-synthetics, designed to be anti-staphylococcal)
- Not great gram negative or anaerobic coverage
- Best used for MSSA (nafcillin is the drug of choice)
- Q4 hour administration: very difficult to achieve
- 1:1 interchange cefazolin for nafcillin, cefazolin can be Q8 hours for easier administration
- Nafcillin is the only penicillin that is NOT dose adjusted for renal function
- If using cefazolin for endocarditis, you need to use a higher dose
Resistance Mechanism: Beta-lactamase Inhibitors
- Ticarcillin-Clavulanate, Ampicillin-Sulbactam, Amoxicillin-Clavulanate
- Gram negative coverage is increased.
- Anaerobes covered about as well as penicillin.
- Ticarcillin/clavulanic Acid: First anti-pseudomonal drug, was the drug of choice for stenotrophomonas (until it stopped being made)
- Ampicillin-Sulbactam: is sometimes used as a sulbactam load for Acinetobacter
- Pip-Tazo: pipericillin gave pseudomonas coverage, tazobactam added better gram negative coverage for enterobactericiae family and some resistant e.coli
Cephalosporins
- First Generation: Cefazolin
- MSSA (drug of choice at UCMC): therapeutic interchange for nafcillin
- Coagulase-negative staphylococcus coverage
- Decent strep coverage but not a great go-to
- Second Generation: Cefotetan, Cefaclor, Cefuroxime
- Increased gram negative rod coverage (E. Coli, Proteus)
- Respiratory infection coverage
- More frequently used in pediatrics
- NO ANAEROBIC COVERAGE
- Third Generation: Ceftriaxone, Ceftazidime, Cefotaxime
- Neisseria coverage
- Strep pneumo
- H. influenzae
- Moraxella
- E. Coli
- Ceftriaxone:
- Often dosed every 24 hours, however in the ICU more commonly dosed Q12 (not renal or hepatically cleared).
- It is cleared through the biliary system and can cause slugging, particularly in children.
- Recommended dosing 2 gm, Q12 hours
- Ceftazidime: pseudomonal coverage (first cephalosporin to do this) - good gram negative coverage but you lose gram positive coverage so you don't want to use it for S. pneumo, URI, or meningitis.
- Important to note the resistance mechanism in Enterobactericiae: ampC inducible resistance which is not detectable in the lab, can be induced by 3rd gen cephalosporin - this can be overcome with addition of an aminoglycoside or use of fourth generation cephalosporin instead.
- NO ANAEROBIC COVERAGE
- Fourth Generation: Cefepime
- Pseudomonas coverage
- Increased Gram negative coverage - primarily enterobactericiae
- Again, NO ANAEROBIC COVERAGE
- Still have S. Pneumo coverage, but not great for CONS, MSSA etc
- Fifth Generation: Cephterolime
- Developed for MRSA Coverage however it is unfortunately becoming more resistant.
- Decreased GNR - does not cover pseudomonas, acinetobacter, or enterobacter
- Does cover salmonella
Carbopenems
- Drug of choice for Acinetobacter
- Covers GR+, GR-, Anaerobes
- Developed to cover Enterococcus
- Anti-Pseudomonal as well
- Drugs: usually q8-q12, renal dosing
- Meropenem - Acinetobacter
- Imipenem - Acinetobacter
- Doripenem
- Ertapenem "The Evil Stepsister": dosed q24 hours, but is not very broad coverage as it does not cover pseudomonas or enterococcus. Used after MIC levels come back, it's a good q24hr dosing regimen for transition to outpatient. Should never be used empirically because it misses that coverage in critically ill patients.
Monolactam: Aztreonam
- Pseudomonas coverage
- Good gram negative coverage, no gram positive coverage
- Good CNS penetration
- Monolactam: does not cross react in people who have a true, anaphylactic reaction to beta-lactams.
Remember: Cephalosporins do NOT cover anaerobes or enterococcus.
Case Follow Up with Dr. Robert Whitford
Case: 60 yo F w/ history of liver failure status post transplant 1 month ago presents with chest pain.
EKG: Prehospital compared to initial showed subtle ST segment elevations in the inferior leads which appeared to be evolving
Labs: Troponins negative
Cath: DES deployed to LAD
Follow up: She returns one week later with deep symmetric T wave inversions in the inferior leads with elevated troponin. Admitted to CVICU on heparin. Taken back to cath lab with a new blockage found in the RCA and another DES placed. Likely due to ruptured, previously non-obstructing, plaque.
ACS is a dynamic process.
The composition of plaques, not necessarily the size, within the coronary arteries can predispose to risk. Early Cath in NSTEMI/UA: literature has not shown mortality or decreased MI benefit.
Wellen's Syndrome: Unstable angina - do not stress these patients, high risk, admit.
Take Home Points:
- History is the #1 predictor of ACS
- Non-traditional ACS risk factors: ESRD, pregnancy, HAART, steroids, lupus
- Prehospital EKG, serial EKGs capture more ACS
- Interpret ST segments in proportion to QRS
- Plaque composition, not size, is what matters. Don't be fooled by "non-obstructive" CAD.
Taming the SRU with Dr. Nick Ludmer
The Case: 33 yo female, found down at the base of 8 steps, + LOC, GCS 15 on scene, severe abdominal pain and back pain. Also, she's 32 weeks pregnant.
Trauma Assessment in Pregnancy:
- Background
- Trauma affects 5-9% of pregnancies
- 46% of all maternal deaths are trauma related
- 1/3 of admitted trauma patients will be delivered, fetal death rate is relatively high
- Domestic violence incidence is higher in pregnant patients
- Pregnancy is a risk factor for trauma.
- Primary Assessment
- Assemble your team: Trauma and OB STATs
- Primary Assessment of the Pregnant Trauma Patient
- Focus on the mom (ABCs):
- Maternal death is main cause of fetal death
- Maternal shock associated with 80% fetal mortality
- Primary Survey: unique considerations
- Higher risk of aspiration due to increased pressure on stomach from gravid uterus and lower esophageal sphincter tone is decreased. Consider stomach decompression.
- Elevated diaphragm means decreased vital capacity, decreased reserve for intubation.
- IVC compression from gravid uterus, consider positioning during resuscitation.
- High output/Low resistance system during pregnancy due to utero/placental system: BP drops
- Fetal Evaluation: recommended as part of primary survey, apply monitors, fetal distress may be apparent before maternal distress
- Focus on the mom (ABCs):
- FAST Exam
- Single center trial showed that it is useful in pregnancy
- What about radiation based imaging?
- Anything below 50 mGy cumulative should have no consequence on the fetus.
- CT of the abdomen/pelvis: ~30 mGy
- Nearly every other imaging study is about 20 mGy or much less: go ahead and get the CT Head, extremity x-rays etc.
- If Unstable --> Go to the OR. Trauma + OB.
- Stable Patients: Secondary Survey (special considerations)
- Pre-Term Labor
- Risk increases 2X even with minor trauma
- Contractions/rush of fluid
- Placental Abruption
- 5-50% of cases depending on severity of injury
- High risk for fetal demise
- Abdominal pain, uterine contractions, hypertonicity, vaginal bleeding
- Clinical diagnosis
- Ultrasound is NOT sensitive. 50-80% false positive rate.
- Delay in recognition is responsible for 60% of preventable deaths
- Consider CT in cases that are unclear. Good sensitivity and sensitivity.
- Uterine Rupture
- Rare 0.6%
- Risk factors: scarred uterus (fibroids/c-section)
- Peritoneal signs, abnormal uterine contour, guarding, rigidity
- These patients are typically in extremis.
- Direct Fetal Injury
- < 1% of blunt trauma
- More common with pelvic fractures if fracture fragment injures uterus and fetus.
- Rh Alloimmunization: Consider giving Rhogam to Rh- mothers in trauma.
- Pre-Term Labor