To Appendectomy or Not to Appendectomy: The Alvarado Score
/Appendicitis is the most common surgical emergency that emergency physicians encounter each year. The prevalence of appendicitis in the US is estimated at 7%, with an incidence of 9.38 per 10,000 people annually [1,2]. Appendicitis shares many signs, symptoms, and laboratory features with other acute medical and surgical conditions, including diverticulitis, nephrolithiasis, and ovarian pathologies like tubo-ovarian abscess and ovarian torsion. Diagnostic tools such as the Alvarado score are designed to help emergency clinicians sharpen their diagnostic acumen by stratifying the likelihood of appendicitis based on scoring systems.
ORIGINS OF THE ALVARADO SCORE
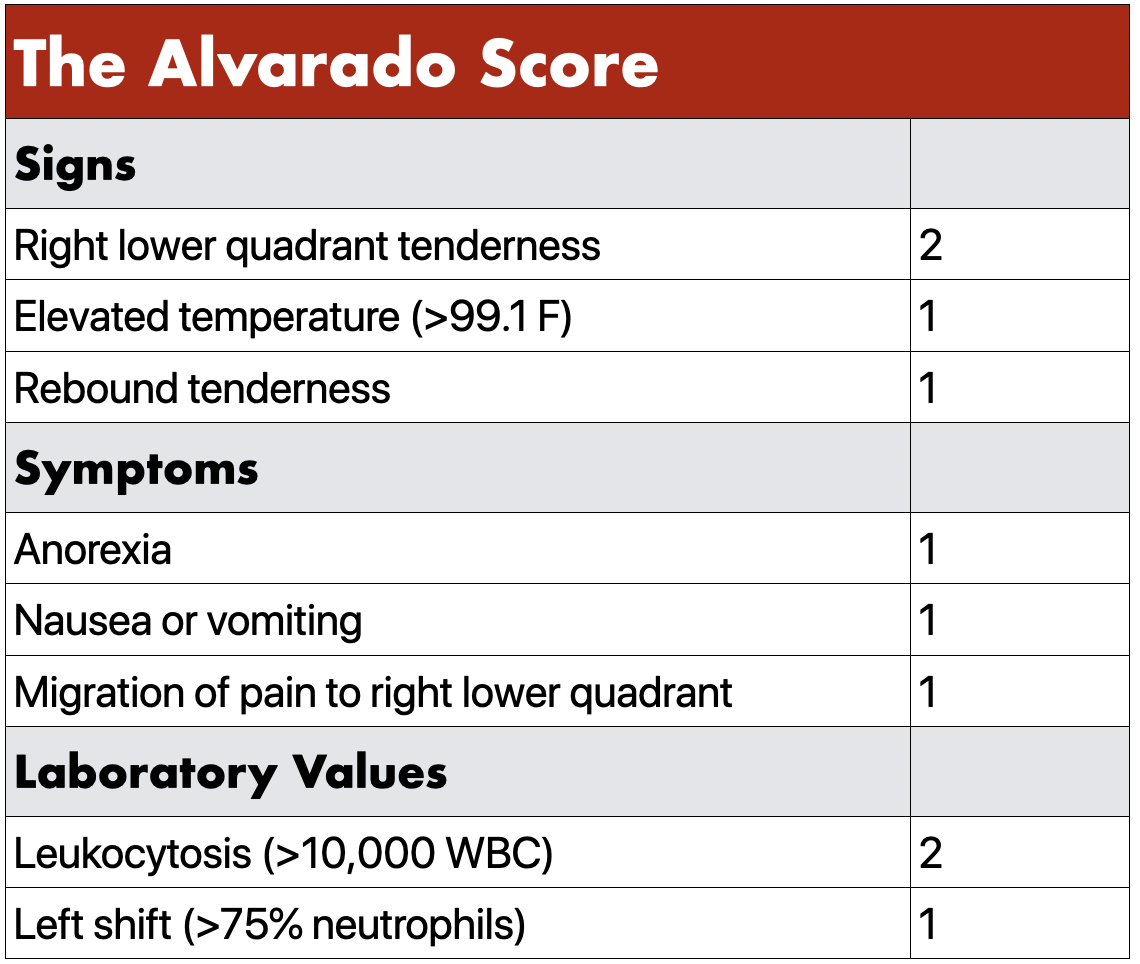
Table 1 - Scoring schema for the Alvarado Score
Dr. Alfredo Alvarado initially devised this appendicitis-scoring tool in Philadelphia, Pennsylvania as part of a retrospective study published in Annals of Emergency Medicine in 1986 [3]. Surgery rather than cross-sectional imaging was the most common way to diagnose appendicitis at this time; therefore the goal of this study was to reduce the number of negative appendectomies. Dr. Alvarado chose eight factors most commonly associated with appendicitis and weighted them according to their test characteristics and their ability to accurately predict appendicitis. These factors were comprised of signs, symptoms, and laboratory values. Their importance was weighted, from most predictive to least predictive, as follows: RLQ tenderness, leukocytosis, migration of pain, left shift on CBC, fever, nausea/vomiting, anorexia, and rebound tenderness. The most predictive factors were assigned a higher points value in the Alvarado score, with tenderness in the right lower quadrant and leukocytosis assigned values of 2 points, which is demonstrated in Table 1. The remaining six factors were given a points value of 1, as they demonstrated less diagnostic certainty. The maximum Alvarado score was therefore 10. The clinical implications of each score total listed in the original paper are summarized in Table 2.
Table 2 - Clinical Implications of the Alvarado Score
VALIDITY & ADJUNCTS
Since its inception, numerous studies have attempted to ascertain the validity of the Alvarado score in different clinical populations. A systematic review performed in 2011 assessed the diagnostic accuracy of the score at two cutoff points: 5 and 7 [4]. The cutoff point of 5 was used to delineate admission versus discharge for these patients; if a patient had a score of 1-4, appendicitis was unlikely and they could be discharged with return precautions. A score of 5-10 indicated admission or at least observation was needed, with probable additional diagnostic studies such as CT scan indicated to further elucidate whether appendicitis was present. This cutoff score of 5 was 99% sensitive for ruling out appendicitis. The cutoff point of a score of 7 or greater was used to analyze whether this score was sufficient to proceed directly to surgery. A score of 7-10 was only 82% specific for appendicitis in this study, meaning that the Alvarado score was less adept at “ruling in” the need for surgery based on higher scores.
Further studies have attempted to incorporate CT scan into the scoring system to better apply it to modern clinical practice [5]. A score of 4-6 was determined to be “equivocal” with only 35.6% sensitivity for appendicitis. The sensitivity of CT scans in this population was 90.4%, which led to the conclusion that equivocal Alvarado scores would likely benefit from CT scans. This study recommended no imaging in scores of 0-3, and surgical consultation for scores of 7-10. Another study in 2018 used the score to reduce exposure to unnecessary radiation and to reduce the length of stay in certain patients with abdominal pain [6]. This study examined almost 500 patients and showed that scores of 0-1 had a 0% incidence of appendicitis, whereas scores of 9-10 in men and 10 in women had a 100% incidence of appendicitis.
Ultrasound has become increasingly important in the evaluation of appendicitis, particularly in children and pregnant women where exposure to radiation from CT scans is especially harmful. Some studies have combined the Alvarado score with ultrasound in attempt to improve the test characteristics compared to the use of either tool alone. One such study used the Alvarado score to improve the negative predictive value of an inconclusive appendicitis ultrasound in pediatric patients [7]. An inconclusive appendicitis ultrasound coupled with an Alvarado score of less than 5 demonstrated a negative predictive value of 99.6% in a population of 522 children. A score of 5-8 coupled with an inconclusive ultrasound demonstrated a negative predictive value of 89.7% in the same population.
CONCLUSION
Overall, the Alvarado score by itself is most definitive at the extremes of its values. A very low Alvarado score is quite sensitive to rule out appendicitis, meaning the clinician may be able to forgo imaging, as it is unlikely to show appendicitis in these cases. A very high Alvarado score is relatively specific for appendicitis, and it may be appropriate to proceed to surgical consultation without obtaining CT or other diagnostic imaging if one’s suspicion is high enough. The “gray area” of the Alvarado score is equivocal and requires further diagnostic studies, such as CT or ultrasound, to determine whether appendicitis is present. Though an experienced clinician’s clinical gestalt may be just as good or better than the Alvarado score at determining the likelihood of appendicitis, the score can help more novice clinicians stratify the risk of appendicitis in certain patient populations.
REFERENCES
1. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910-25.
2. Buckius MT, Mcgrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012;175(2):185-90.
3. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-64.
4. Ohle R, O'reilly F, O'brien KK, Fahey T, Dimitrov BD. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med. 2011;9:139.
5. Mckay R, Shepherd J. The use of the clinical scoring system by Alvarado in the decision to perform computed tomography for acute appendicitis in the ED. Am J Emerg Med. 2007;25(5):489-93.
6. Coleman JJ, Carr BW, Rogers T, et al. The Alvarado score should be used to reduce emergency department length of stay and radiation exposure in select patients with abdominal pain. J Trauma Acute Care Surg. 2018;84(6):946-950.
7. Blitman NM, Anwar M, Brady KB, Taragin BH, Freeman K. Value of Focused Appendicitis Ultrasound and Alvarado Score in Predicting Appendicitis in Children: Can We Reduce the Use of CT?. AJR Am J Roentgenol. 2015;204(6):W707-12.
Written by Kristin Meigh, MD
Dr. Meigh is a PGY-1 at the University of Cincinnati Department of Emergency Medicine