Diagnostics: Ophthalmologic Trauma
/Background
Epidemiology
About 55 million eye injuries occur annually every year and over one fifth of these injuries result in vision that would qualify for legal blindness. It could be your dad building that deck with a table saw and no glasses, your niece playing hockey with a puck to the eye, or even you on your way to work in a car accident. Eye injuries are all around us and are devastating when they happen. How can we evaluate and manage these injuries in the emergency department? First we must understand the anatomy of the eye.
Anatomy
The eye can be broken up into three main layers; external fibrous layer (made of the cornea and sclera), the middle vascular layer (made of choroid, ciliary body, and iris), and the internal layer (retina).
Generally, the sclera (covered by the thin transparent membrane of the bulbar conjunctiva) and cornea form an outer wall with their epithelium forming a barrier against infection. There is also tarsal conjunctiva which covers the underside of the eyelid.
The eye can also be divided into anterior and posterior structures with the lens as the demarcation between the two. Anterior structures include the iris, anterior chamber, and cornea. Posterior structures are the vitreous, retina, choroid, and optic nerve.
Notably, the anterior chamber is filled with aqueous humor and the posterior chamber or vitreous chamber is filled with vitreous humor.
Injuries also often affect the structures surrounding the eye such as the skin and tissues covering the eye or the structures confined in the bony orbit alongside the eye. The eyelid structure is defined by the tarsal plate within it and the canalicular system that drains tears into the nasopharynx.
Finally, as with other fixed compartments in the body, the bony orbit can build pressure and lead to potential damage to the delicate structures confined within. Most commonly this is dangerous for the eye, optic nerve, or the retinal, which can cause ischemic injury.
Injury classification
Traumatic eye injuries can be classified by the areas of the eye that they affect generally in three ways; open globe, closed globe, and periocular (or affected the structures around the eye).
Open Globe
Open globe injuries, or injuries that disrupt the entire outer layer of the eye including the sclera and cornea can be blunt or penetrating in nature. Interestingly, males comprise over 80% of open globe injuries. When the external wall barrier of the eye is opened, there is also a risk of endophthalmitis (infection of internal structures of the eye) which is most commonly due to bacillus or coag negative staphylococcus species.
Blunt injuries, due to general external pressure, tend to disrupt the external layer at weak points such as the limbus (transition from cornea to sclera) or at the insertion of the rectus muscles. Previous ocular surgeries tend to increase the risk of blunt trauma leading to open globe injury.
Penetrating injuries, due to piercing external pressure, can be further classified by the location of injury. Zone 1 being on cornea, Zone 2 being in the anterior sclera, and Zone 3 in the posterior sclera.
A specific subtype of penetrating trauma to the eye would be the intraocular foreign body. These injuries usually are due to a metallic object, such as BB pellet or construction work material and are associated with a worse overall prognosis and risk of infection.
Signs of an open globe injury include: obvious penetrating foreign body, significantly decreased visual acuity, teardrop pupil, extrusion of vitreous, or prolapse of internal eye structures like iris, ciliary body, or choroid.
Closed Globe
Closed globe injuries can be injuries with partial thickness wounds to the outer layer of the eye (called lamellar lacerations) or no eye wall wound (called contusions). Lamellar lacerations include conjunctival lacerations, partial thickness scleral lacerations (not through the choroid), and partial thickness corneal lacerations (not deep enough to cause leak of aqueous humor). Other common closed globe injuries include:
Abrasions of the conjunctiva (over the sclera) or the cornea
Hyphema (bleeding in anterior chamber, see below) or vitreous hemorrhage (bleeding in vitreous chamber)
Iritis or inflammation in anterior chamber due to trauma
Displacement of eye structures such as lens dislocation or retinal detachment
Commotio retinae (self-limited retinal edema after blunt closed-globe injury)
Periocular
Lastly, periocular injuries can occur in isolation or in combination to ocular injuries and these can be further classified into pre-septal or orbital depending on if they affect superficial structures or deeper eye structures.
More superficial preseptal injuries can range from simple bruising or periocular ecchymosis to eyelid lacerations that require surgical repair. Canalicular lacerations require even more specialized surgical repair due to the disruption of the lacrimal drainage system.
As injuries delve deeper into the periocular structures, prognosis worsens with possible injuries to:
Levator muscles of the eyelid leading to ptosis
Fractures to the bones of the orbit that can result in CSF leakage, optic nerve injury, or muscle entrapment
Optic nerve leading to traumatic neuropathy or full avulsion of the nerve
Ophthalmic artery leading to ischemic damage to the eye
Diagnostic Evaluation
As with all trauma, it is important to evaluate and stabilize the life threatening injuries first and once injuries are confirmed to be only affecting the eye the vision threatening conditions must first be addressed.
History
To initially determine if there are any vision threatening conditions present, a focused history and basic physical exam are most helpful. Initial history should focus on mechanism of injury, time and location, symptoms, and ocular adjuncts/ocular history such as contact lenses or glasses. Importantly, if there is chemical exposure this should change immediate management to avoid vision loss (see management below). Once initial stabilization is completed then a more detailed history can be collected such as medications, allergies, past medical conditions, tetanus status, and last oral intake.
Stepwise Initial Exam
An initial exam should include a simple “look and see” visual assessment of eyes and periocular structures to understand which areas are affected, such as if there is an eyelid laceration or protruding foreign body. If no obvious initial injury then three main components of triaging a traumatic eye injury are:
1. Visual acuity - either measured with finger counting or more specifically with modified Snellen chart to determine level of current visual threat. It is also important to ask and understand baseline visual acuity and if visual adjuncts (contact lenses or glasses) are currently present.
IF there is significant acute decrement to visual acuity THEN the cause should be determined more quickly.
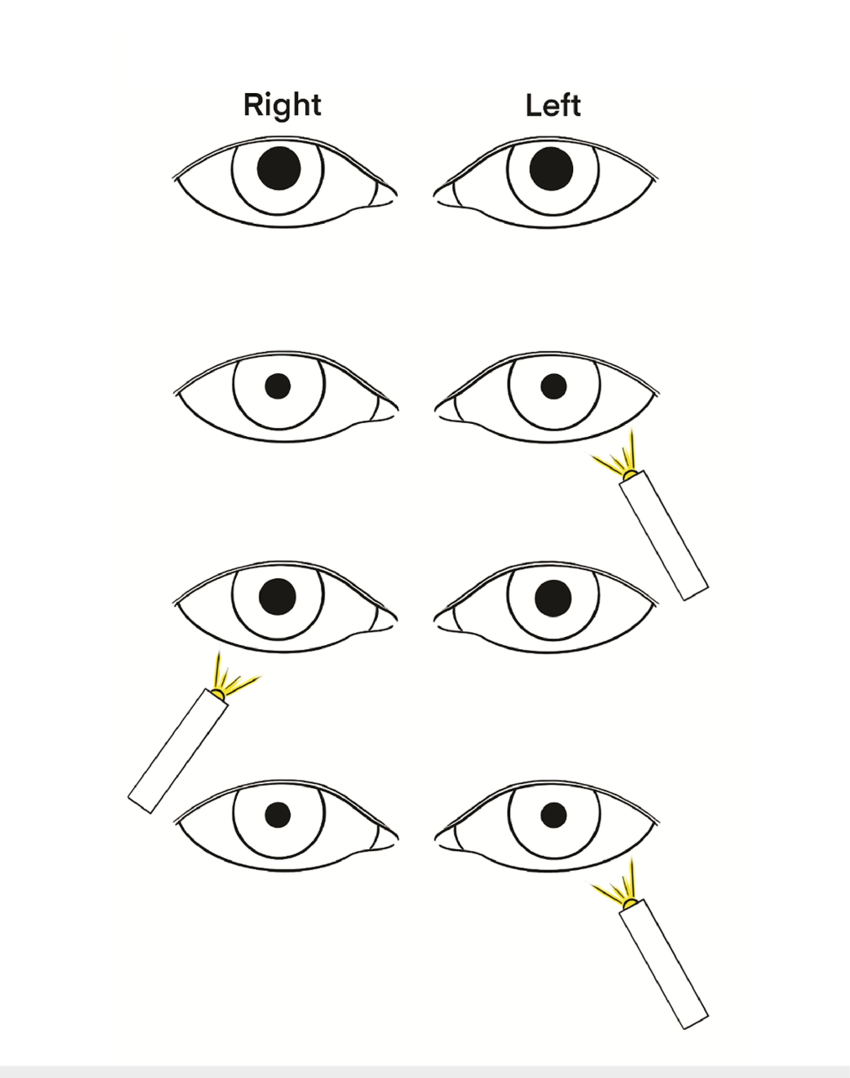
2. Pupillary response - especially with swinging flashlight test to establish if injury to the afferent (or toward the brain) system of light transmission is intact. This would include the passage through the globe/lens, retina, and optic nerve.
A relative afferent pupillary defect (RAPD) is present in situations when the light signal is not being transmitted to the brain and bright light in the affected eye will not cause any constriction of the pupil but light in the contralateral eye will cause constriction of both pupils.
IF a RAPD is present indicating a problem with transmission of light signal THEN the red reflex should be evaluated.
3. Red reflex is used to determine if there is any opacification or object blocking the visual axis of the eye. If a new (not already present prior to injury) asymmetric red reflex is present in the setting of a rAPD then this suggests a retinal injury or vitreous hemorrhage. If there is a symmetric red reflex but a present RAPD then the issue with transmission of light signal is behind the eyes and the optic nerve should be further evaluated (see further studies below).
A red reflex is elicited shining a light (often in a dim setting with a fundoscope) through the visual axis of cornea, pupil, lens of the eye to the retina and eliciting a reflection of red light back to the observer's eye.
IF RAPD is absent THEN the initial exam should focus on eliciting any signs of open globe injury (discussed above) as this will guide immediate management. It’s important to remember that normal visual acuity doesn’t necessarily preclude the possibility of open globe injury.
IF no signs of an open globe THEN evaluate for a traumatic hyphema by looking for signs such as photophobia, anisocoria, or gross blood in the anterior chamber.
IF cause of visual acuity decrement still not apparent THEN further sequential exam and studies guided by history should help rule out other vision threats and pinpoint any traumatic ophthalmologic injury.
In-Depth Eye Exam
Visual acuity should be more thoroughly tested with each eye alone and with/without visual adjuncts. Normal is denoted as 20/20 with numerator referring to distance from chart and denominator referring to smallest line able to be read. This can be tested with classic Snellen charts, pediatric vision charts, or phone apps.
Inspecting periocular structures more closely specifically looking for eyelid lacerations, lid function (evaluating function of levator muscles and cranial nerves III/VII), facial sensation (cranial nerve V function), and palpation for bony step offs or crepitus (concern for orbital fractures or communication with sinuses). Notably, a ‘rock-hard’ eyelid, periocular swelling, and proptosis which may further indicate orbital compartment syndrome (OCS).
Pupil function and shape should be assessed as discussed above in the initial exam. Extraocular eye movements should be assessed in all directions to determine if any pain with movements or limited motility which may suggest direct muscular damage, entrapment, hematoma or swelling leading to impingement, or cranial nerve injury.
Tetracaine and other topical analgesia has been associated with delayed healing, corneal infection, and scarring in animal models so best to avoid when possible but helps to facilitate a more thorough exam.
Given time and equipment, a slit lamp examination is the gold standard evaluation tool for the anterior segment (corena, sclera, conjunctiva, anterior chamber, iris) of the eye. This should be done both with and without fluorescein stain. This stain can help elucidate epithelial defects such as abrasions and further can indicate micro-perforation injury with the Seidel test. The Seidel sign is the streaming of aqueous humor through the fluorescein as seen below.
Conjunctiva and cornea should be evaluated for subconjunctival hemorrhage, lacerations, foreign bodies, corneal edema, or chemosis (collection of fluid within the conjunctiva, also termed conjunctival edema).
The iris should be evaluated for sphincter tears on pupil margin that can result in mydriasis and the anterior chamber itself should be evaluated for “cell and flare” or floating white blood cells that may be a sign of traumatic iritis. Microhyphema may also be visible on slit lamp that can not be seen with general examination.
Lens opacification, subluxation (shifting off center), or complete luxation (either anteriorly or posteriorly) can also occur with trauma and be evaluated.
Intraocular pressure monitoring should be performed, such as with Tono-Pen, to evaluate for pressures greater than 21 mmHg (upper normal) which may indicate hyphema, OCS, hematoma, or even carotid-cavernous sinus fistula. However, if you are concerned about an open globe, DO NOT put further pressure on the globe.
Imaging Adjuncts
If there are any concern for open globe, foreign body, optic nerve injury, orbital fracture, or OCS (after emergent management) then computed tomography (CT) of orbits without contrast is preferred imaging test.
Ultrasound is extremely useful for expedited bedside evaluation of traumatic eye injury and has shown high sensitivity and specificity for lens dislocation, retrobulbar hematoma, retinal detachment, vitreous hemorrhage, and intraocular foreign body. More rarely, US with doppler color flow can identify carotid cavernous sinus fistulas as well. However, almost all findings on US are confirmed with further CT imaging or expert ophthalmologic examination.
Management
While a thorough diagnostic evaluation is necessary when permitted by time and resources, as soon as a vision threatening condition is identified it should be managed quickly to avoid permanent vision loss.
Vision Threatening Conditions
In any of these cases Ophthalmology consultation is warranted for further evaluation following stabilization.
Chemical exposure:
If chemical exposure is suspected, an initial decontamination should be performed prior to eye evaluation, and considerations should be made for systemic exposure and inhalation effects. History should include which chemicals are involved, duration of exposure, and depth of penetration to help guide management. Generally decontamination includes brushing off dry agents when possible around the eyes and removal of any contact lenses, clothing, or jewelry. A pH measurement should be performed in inferior fornix of eye, and if pH is < 6.5 or > 7.5 then irrigation should be initiated with copious water irrigation either manually or with Morgan Lens. The pH should be re-measured every 30 minutes until normal pH is reached. Some chemicals in which water irrigation is not recommended are dry lime, phenols, or elemental metals.
Orbital Compartment Syndrome (OCS):
OCS is a clinical diagnosis indicated classically by eye pain, swelling, proptosis, elevated IOP (palpated as hard globe), and presence of RAPD or visual acuity decrement. OCS is a true emergency and requires immediate intervention with lateral canthotomy to decompress the pressure built up in the orbit by cutting the lateral canthus and releasing the lateral canthal tendon. This procedure (detailed below) should not be delayed for IOP measuring or imaging if the signs above are present, but should be followed by monitoring of IOP and CT of orbits. If performed correctly, this procedure should immediately begin to resolve symptoms associated with OCS and decrease the risk of permanent vision loss.
Open Globe Injury & Large Penetrating Foreign Body:
If an open globe is suspected then providers should avoid ANY procedure or exam that places further pressure on the eyeball and ANY direct application of medication to the eye. Do not remove any protruding foreign bodies. Immediate CT and ophthalmology consultation should be performed. Make the patient NPO for surgical repair ideally within 24 hrs and start IV empiric antibiotics usually including Vancomycin and Ceftazidime or other fluoroquinolone to cover pseudomonas. Ketamine should be avoided to avoid perpetuation of increased IOP and rocuronium should be used instead of succinylcholine in the case that RSI is necessary. Control IOP by strictly managing pain, nausea and vomiting, and constipation. Consider elevating the head of the bed as well.
Traumatic Hyphema:
If suspected due to findings above including layering of blood in anterior chamber, photophobia, decreased visual acuity, eye pain with pupillary constriction, or abnormal IOP then obtain further diagnostic evaluation including complete blood count,coagulation studies, and CT orbits. Hyphema is highly associated with other injuries to head, orbital bones, and open globe injuries. Sickle cell disease or trait and other bleeding disorders are associated with much worse prognosis of hyphema and should be treated appropriately with consultation of a hematologist. Similarly to open globe injuries, manage IOP closely and avoid ketamine and rocuronium. In consultation with an ophthalmologist, cycloplegics (i.e. cyclopentolate) can help manage pain and facilitate an exam. Further topical glucocorticoids can help reduce rebleeding and control inflammation. With less severe hyphemas, an eye shield can be placed and activity can be restricted for just 1-2 wks.
Vitreous Hemorrhage:
Should be suspected in setting head trauma with decreased vision, hazy vision, “black spots”, or “cobwebs” and may be further suspected in the case of loss of red reflex as above. May also be a sign of non-accidental trauma in young children.
Retinal Detachment:
Retinal detachment should be suspected in cases with loss of vision like a “curtain” coming across or down vision and loss of red reflex as above. Level of injury is best evaluated on fundoscopic exam with scleral compression exam (compression of globe to see edges of retina) but more easily seen on ultrasound. Ultrasound may also help distinguish whether the macula of the retina is still attached, in which case urgent surgery is indicated to ensure the detachment doesn’t progress to loss of vision. Acute retinal breaks occur with flashes or floaters and may require laser therapy or cryotherapy depending on the ophthalmologic evaluation. Purtscher retinopathy is another syndrome related to a compression injury of the legs, arms, or chest that can result in retinal hemorrhages and sudden decreased vision without direct injury to the eye but has no specific eye treatment.
Optic Nerve Injury:
Optic nerve injuries may be direct (laceration trauma to optic nerve) or indirect (contusion to nerve via injury to optic canal). A CT of orbits is recommended in all suspected cases and treatment depends on exact etiology and CT findings. Steroids are not routinely recommended.
Common Conditions
Once the vision threatening conditions have been ruled out, it is important to recognize and treat the most common traumatic conditions of the eyes.
Eyelid Lacerations:
Usually obvious on exam, these lacerations have been associated with ocular injury in up to two-thirds of cases. Globe injury should be suspected if the exam reveals fat prolapse (indicating damage to the underlying levator muscle, orbital septum), full thickness wound, or protruding foreign bodies. Ophthalmologist or cosmetic surgeon should be consulted in these cases or if there is extension through lid margin or medial canthus involvement (indicating possible damage to lacrimal system). Otherwise, typical laceration considerations should be taken into account and 6-0 fast gut or 7-0 nylon / prolene should be used in repair.
Corneal Abrasions & Small Foreign Bodies:
Seen on slit lamp exam and confirmed with fluorescein, these injuries are amongst the most common in the emergency department. If the abrasion is associated with a white spot or opacity suggesting corneal ulceration, a foreign body that can’t be removed, or hypopyon, then an ophthalmologist should evaluate the patient on the same day. More urgent evaluation should be consulted if there is purulent discharge, a significant acute decrease in visual acuity, an abrasion that is refractory to healing, or if the patient wears contact lenses due to the concern for retained foreign body, poor healing, superinfection, or infectious keratitis. All corneal abrasions should be treated with topical antibiotics due to risk for infection. If contact lens wearer, then pseudomonas coverage should be applied.
Removal of small foreign bodies is often done with water irrigation, a cotton swab, or a 25g needle. Sometimes these foreign bodies are associated with rust rings (or deposition around the foreign body on the conjunctiva. We recommend that rust rings should not be removed in the emergency department due to the potential for scarring and should be managed by ophthalmology follow up.
Conjunctival Injuries:
Conjunctival injuries are common due to it being the most external epithelium of the eye. Lacerations and abrasions warrant careful evaluation for open globe injuries and hyphema but if not present then topical antibiotics are a sufficient treatment. Subconjunctival hemorrhages are frequently found with vomiting, trauma, coughing, hypertension, or bleeding disorders. No acute treatment is necessary except for treating any underlying conditions.
Orbital Fractures:
A thorough trauma evaluation should be performed in patients with orbital fractures due to the potential for other co-injury. Often these fractures are associated with bony tenderness and swelling, periocular ecchymosis, diplopia, decreased sensation in face or facial nerve motor ability, or orbital emphysema. CT orbits and/or maxillofacial is indicated. Most orbital fractures are non-operative but may be if there are signs of entrapment, eye displacement, CSF leakage, or sinus disruption. Usually patients can be discharged with sinus precautions (no nose blowing, no straws, elevated head of bed) and intermittent cold application for swelling.
Lens Subluxation or Dislocation:
Lens subluxation (partial displacement) or dislocation (complete displacement) can often occur following trauma to the head or eye. Clinical findings are usually decreased visual acuity, monocular double vision, or a small pupil. If associated with minor trauma, then work up is indicated for Marfan syndrome or homocystinuria. Non-urgent surgery is required to replace the lens.
POST BY Cameron Pawlik, MD
Dr. Pawlik is a PGY-1 in Emergency Medicine at the University of Cincinnati
EDITING BY arthur broadstock, MD
Dr. Broadstock is an Assistant Professor in Emergency Medicine at the University of Cincinnati and assistant editor of TamingtheSRU.com
Cite As: Pawlik C., Broadstock A. Diagnostics: Ophthalmologic Trauma. TamingtheSRU. www.tamingthesru.com/blog/diagnostics/ophthalmologic-trauma. 6/3/2025.
References
Andreoli C, Gardiner M. Open globe injuries: emergency evaluation and initial management. UpToDate. Updated May 12, 2025. Accessed May 26, 2025. https://www.uptodate.com/contents/open-globe-injuries-emergency-evaluation-and-initial-management
Basil G, Luther E, Burks JD, et al. The focused neurosurgical examination during telehealth visits: guidelines during the COVID-19 pandemic and beyond. Cureus. 2021;13(2):e13503. doi:10.7759/cureus.13503
Cruz J. Traumatic ocular injuries. Core EM. Accessed May 20, 2025. https://coreem.net/core/traumatic-ocular-injuries/
Gardiner M. Approach to diagnosis and initial treatment of eye injuries in the emergency department. UpToDate. Updated December 13, 2023. Accessed May 26, 2025. https://www.uptodate.com/contents/approach-to-diagnosis-and-initial-treatment-of-eye-injuries-in-the-emergency-department
Gardiner M. Conjunctival injury. UpToDate. Updated April 24, 2024. Accessed May 26, 2025. https://www.uptodate.com/contents/conjunctival-injury
Gardiner M. Eyelid lacerations. UpToDate. Updated April 21, 2025. Accessed May 26, 2025. https://www.uptodate.com/contents/eyelid-lacerations
Gardiner M. Overview of eye injuries in the emergency department. UpToDate. Accessed May 20, 2025. https://www.uptodate.com/contents/overview-of-eye-injuries-in-the-emergency-department
Jacobs D. Corneal abrasions and corneal foreign bodies: management. UpToDate. Updated March 12, 2025. Accessed May 26, 2025. https://www.uptodate.com/contents/corneal-abrasions-and-corneal-foreign-bodies-management
Kaushik S, Bird S. Topical chemical burns: initial evaluation and management. UpToDate. Updated June 17, 2024. Accessed May 26, 2025. https://www.uptodate.com/contents/topical-chemical-burns-initial-evaluation-and-management
Knoop K. Slit lamp examination. UpToDate. Updated June 25, 2024. Accessed May 26, 2025. https://www.uptodate.com/contents/slit-lamp-examination
McKee C. Air Care Procedures Quick Reference. Taming the SRU. Published December 17, 2015. Accessed May 26, 2025. https://www.tamingthesru.com/air-care-procedures-quick-reference/#canthotomy
Mohseni M, Blair K, Gurnani B, et al. Blunt eye trauma. Updated June 11, 2023. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470379/
Neuman M, Bachur R. Orbital fractures. UpToDate. Updated February 25, 2025. Accessed May 26, 2025. https://www.uptodate.com/contents/orbital-fractures
Nguyen M, Blair K. Red reflex. Updated August 28, 2023. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553139/
Riaz A, Shah C, Wei G. Retinal detachment. J Educ Teach Emerg Med. 2018;3(2):V6–V7. doi:10.21980/J8204Q
Wang D, Rizzuti A. Eye trauma imaging. Updated June 26, 2023. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572102/
Weaver CS, Knoop KJ. Ophthalmic trauma. In: Knoop KJ, Stack LB, Storrow AB, Thurman RJ, eds. The Atlas of Emergency Medicine. 4th ed. McGraw-Hill Education; 2016. Accessed May 20, 2025. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=1763§ionid=125433364
Wee JH, Kim DG, Lee JY, Cho MJ, Shim WS, Jung HJ. A case series of surgical outcomes for orbital blowout fracture with extraocular muscle entrapment. Medicine (Baltimore). 2023;102(44):e34879. doi:10.1097/MD.0000000000034879
Zhou Y, DiSclafani M, Jeang L, Shah AA. Open globe injuries: review of evaluation, management, and surgical pearls. Clin Ophthalmol. 2022;16:2545–2559. doi:10.2147/OPTH.S372011