Diagnostics: Flex your D Dimer
/Few diagnostic tests draw the ire that D dimer does. From ubiquitous to demonic, for most of this test’s existence it has been a dichotomous marker of clot, either a positive led to diagnostic testing and a negative was a clean pass. In this post, we will walk through why we should broaden our view of D dimer and adapt it to a variety of patients to properly risk stratify them.
Background
D dimer is a natural fibrin degradation by product that occurs when a clot is being formed and lysed. D dimer was first discovered in 1973 in both human and bovine models, and appeared to be present when coagulation cascade was being activated. Initially used to detect and trend disseminated intravascular coagulation (DIC), D dimer levels were deemed important with the detection of possible thrombus formation and breakdown, specifically demonstrated in venous thromboembolism (VTE). Since its utilization in detecting thrombotic disorders, a D dimer test has shown to have a high negative predictive value and sensitivity, while consistently having a low specificity. Hence, when the test is negative, no further testing or exploration for VTE is indicated. To better utilize the D dimer diagnostic ability, clinicians began to risk stratify patients based on their likelihood of having a VTE, and whether a D dimer was indicated, immediate imaging or no testing at all.
In general medicine, and especially the emergency setting, pulmonary embolism is one of the six scary chest pain diagnosis that can be mascaraed by various other, potentially more benign diagnoses. But on the other side of the coin, making a definitive diagnosis of pulmonary embolism comes with its own price to pay such as unnecessary radiation exposure and expensive imaging/testing. Therefore, utilizing risk stratification algorithms and D dimer test has real impact on our patient’s care and cost.
Wells Score
Wells Score was initially derived with the intent to risk stratify patients based on their likelihood of having a VTE. By using the Wells criteria, the intention is for patients to undergo less imaging while maintaining satisfactory outcomes. Further discussion of the Wells criteria in general, as well as the argument for the two-tier versus three-tier model can be found here.
YEARS
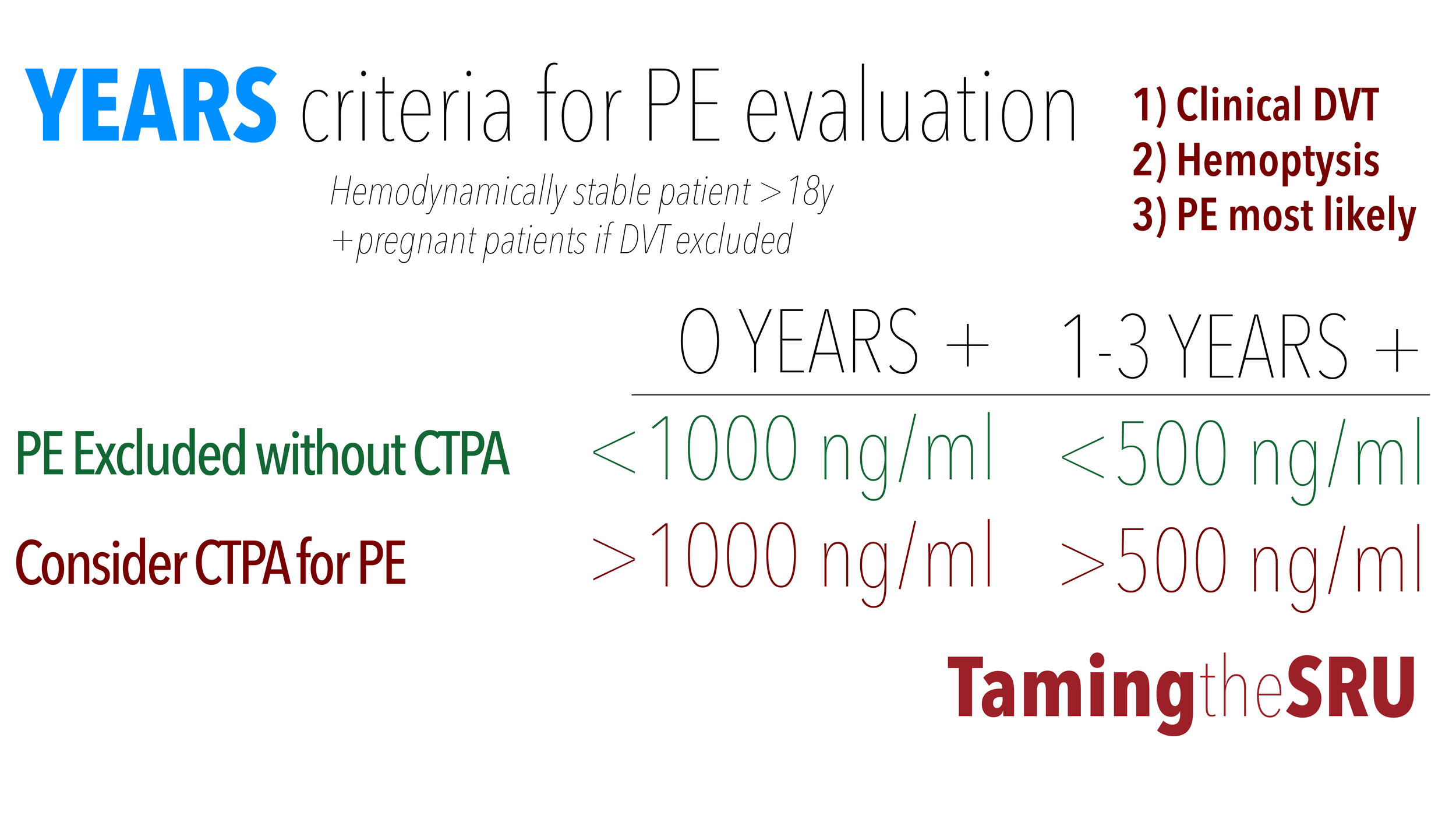
Derived from the Wells criteria, utilizing the three most predictive criteria of DVT, hemoptysis and PE as the most likely diagnosis.
The YEARS score adds an additional tier of risk stratification with two D dimer cutoffs, which is dependent on whether the patient meets zero criteria (1,000 ng/mL), or more than 0 criteria (500 ng/mL).
YEARS was initially evaluated in the Netherlands throughout twelve different institutions using hemodynamically stable patients with a high suspicion for pulmonary embolism. All patients had a D dimer test performed with the matching D dimer cutoff depending on the number of YEARS criteria met on presentation. Of note, if any of the patients had a D dimer above their indicated threshold, they underwent computed tomography with pulmonary angiography (CTPA) for definitive diagnosis. If the patient’s D dimer was below the threshold, the patient was deemed low risk and no further investigation was performed. The primary endpoint to this study was the 3 month incidence of VTE after the initial visit, which was significant for only having 0.61% diagnosed during the follow up period.Of the 3465 patients included in the study, a total of 1629 were ruled out without further imaging or testing performed, with only 7 patients having VTE at three months.
When comparing the YEARS criteria to the Wells Score (two-tier model), the patients in the low risk/PE unlikely, 0.43% compared to 0.5% of patients were diagnosed with VTE within the three month follow up period. And of those patients who underwent a CTPA because their D dimer was above the stated threshold using YEARS or they were deemed PE likely via Well Score, 0.84% compared to 1.3% had a VTE within the three month period. Most notable when comparing the two, using the YEARS criteria reduced overall imaging by 14%.
Pregnancy-adjusted YEARS
However useful D dimer testing is, it certainly has its limitations, one of which being pregnancy. During pregnancy, D dimer levels naturally rise with each trimester, along with the risk of possible VTE. However, with the natural rise, the specificity of a positive or negative D dimer test becomes diminished. Therefore, with the YEARS criteria, an additional component is added as to whether or not the patient is pregnant. If pregnant, the YEARS criteria adds compression venous ultrasound of the affected extremities (most likely lower) to the algorithm if the patient meets clinical criteria for possible DVT. If the patient has a positive ultrasound for DVT, then no further investigation is warranted and anticoagulation is initiated. However, if the ultrasound is negative, the patient continues down the YEARS pathway similar to non-pregnant patients.
Overall, with the pregnancy adjustment made to the YEARS criteria, imaging was reduced by 39% of those patients suspicious for VTE. To further break it down, 65% of women in their first trimester avoided imaging, which is especially important due to the increased teratogenicity of radiation seen with CTPA. As well as, 46% and 32% decrease CTPA in the second a third trimester, respectively. Even more impressive, was the 0.21% DVT incidence within the three month follow up time frame, and 0% of patients having a diagnosed PE.
Age-adjusted D dimer
Another known limitation of the D dimer test is age greater than 50 years. This appears to be secondary to the comorbidities associated with older age, such as liver disease or renal dysfunction. As a way to combat the increased false positive rates, the age-adjusted D dimer was established as the patient’s age times ten (age x 10ug/mL). Initially created using a prospective study over three years (2010 to 2013), where the primary outcome was incidence of VTE at three months after initial evaluation. The two-tier wells criteria was used to determine which patients were PE likely (>4 points) or PE unlikely (<4 points). For patients scored to the PE likely category, they underwent definitive imaging, whether that was CTPA or V/Q scan was determine by associated health conditions and availability of resources. If the patient was scored to the PE unlikely subgroup, then the age-adjusted D dimer was applied. D dimer above the adjusted cut off, patients continued to definitive imaging; however, if the patient did not meet their age adjusted D dimer, then no further investigation of VTE was performed.
In meta-analysis, systemic review performed by Schouten et al (2013), the age-adjusted D dimer was found to have a decreased sensitivity of 1-2% compared to the Wells score, but the overall specificity was increased by 15-20% in patients >50 years old. Sharp et al (2016) also applied the age adjusted D dimer to approximately 31,000 patients >50years old presenting with symptoms suggestive of PE (shortness of breath with/without chest pain), and found that the specificity and sensitivity decreased by 5% and 10%, respectively, compared to the conventional cut off of 500. Historically, D dimer testing has always had a low specificity but high sensitivity, making it a useful test to rule out the diagnosis of DVT/PE. Another incidental finding associated with the use of age-adjusted D dimer, was the relative decreased in contrast induced nephropathy seen with CTPA, with 200 patients being excluded from imaging compared to 43 with the standard cutoff.
PEGeD
More recently, the PEGeD study was performed to further assess risk stratification with D dimer. Kearon et al performed a prospective, multisystem study where they placed patients suspected of having a PE into three categories: 1) low clinical pretest probability (C-PTP), 2) moderate C-PTP and 3) high C-PTP. D dimer cutoffs were assigned as <1,000, <500 and definitive imaging respectively. At three months, both the low and moderate C-PTP had zero patients with reported VTE. Additionally, by using PEGeD algorithm, the study population had a significant decreased in imaging from 51.9% with the standard algorithm to 34.3%.
summary
When comparing the various D dimer adjuncts, they all have their intended uses and targeted populations. The PEGeD study is the newest of the adjuncts but seems promising with its overall reductions in imaging and promising three month follow results. However, when comparing convenience and practicality, the YEARS criteria only asks for the clinician to remember three measures in order to properly use the algorithm, with an added reduction in imaging compared to the standard. Pregnancy-adjusted YEARS does ask for an additional step with the tradeoff of less imaging/radiation exposure to the gravid uterus. With the age-adjusted D dimer, there was also an apparent reduction in imaging and CIN compared to the standard Wells score, even with the reduction in sensitivity. So when asking which is the better algorithm to use, the answer is dependent on which population the clinician is applying it to.
Post by Andrea Comiskey, MD
Peer editing by ryan lafollette, MD
References
Hill, Jeffery. “PERCs of the Wells Score.” Taming the SRU, Taming the SRU, 4 May 2019, www.tamingthesru.com/blog/2019/5/4/percs-of-the-wells-score.
Hulle, Tom Van Der, et al. “Simplified Diagnostic Management of Suspected Pulmonary Embolism (the YEARS Study): a Prospective, Multicentre, Cohort Study.” The Lancet, vol. 390, no. 10091, 2017, pp. 289–297., doi:10.1016/s0140-6736(17)30885-1.
Kabrhel, Christopher, et al. “Factors Associated With Positive D-Dimer Results in Patients Evaluated for Pulmonary Embolism.” Academic Emergency Medicine, vol. 17, no. 6, 2010, pp. 589–597., doi:10.1111/j.1553-2712.2010.00765.x.
Kline, J. A., et al. “Clinical Criteria to Prevent Unnecessary Diagnostic Testing in Emergency Department Patients with Suspected Pulmonary Embolism.”Journal of Thrombosis and Haemostasis, vol. 2, no. 8, 2004, pp. 1247–1255., doi:10.1111/j.1538-7836.2004.00790.x.
Kline, J. A., et al. “Prospective Multicenter Evaluation of the Pulmonary Embolism Rule-out Criteria.” Journal of Thrombosis and Haemostasis, vol. 6, no. 5, 2008, pp. 772–780., doi:10.1111/j.1538-7836.2008.02944.x.
Penaloza, Andrea, et al. “Comparison of the Unstructured Clinician Gestalt, the Wells Score, and the Revised Geneva Score to Estimate Pretest Probability for Suspected Pulmonary Embolism.” Annals of Emergency Medicine, vol. 62, no. 2, 2013, doi:10.1016/j.annemergmed.2012.11.002.
Pol, Liselotte M. Van Der, et al. “Pregnancy-Adapted YEARS Algorithm for Diagnosis of Suspected Pulmonary Embolism.” New England Journal of Medicine, vol. 380, no. 12, 2019, pp. 1139–1149., doi:10.1056/nejmoa1813865.
Righini, Marc, et al. “Age-Adjusted D-Dimer Cutoff Levels to Rule Out Pulmonary Embolism.” Jama, vol. 311, no. 11, 2014, p. 1117., doi:10.1001/jama.2014.2135.
Schouten, H. J., et al. “Diagnostic Accuracy of Conventional or Age Adjusted D-Dimer Cut-off Values in Older Patients with Suspected Venous Thromboembolism: Systematic Review and Meta-Analysis.” Bmj, vol. 346, no. may03 1, 2013, doi:10.1136/bmj.f2492.
Sharp, Adam L., et al. “An Age-Adjusted D-Dimer Threshold for Emergency Department Patients With Suspected Pulmonary Embolus: Accuracy and Clinical Implications.” Annals of Emergency Medicine, vol. 67, no. 2, 2016, pp. 249–257., doi:10.1016/j.annemergmed.2015.07.026.