Air Care Series: Drowning
/Introduction
Despite what colloquial terms would have people believe there is only one type of drowning - drowning. Specifically, experts define drowning as “a process resulting in primary respiratory impairment from submersion/immersion in a liquid medium. Implicit in this definition is that a liquid/air interface is present at the entrance of the victim’s airway, preventing the victim from breathing air. The victim may live or die after this process, but whatever the outcome, he or she has been involved in a drowning incident.” Terms like “near-drowning” or “dry drowning” are ambiguous and have fallen out of favor with drowning experts and the medical community in general. [1,2] If the patient has no respiratory impairment this is considered a water rescue and not a drowning.
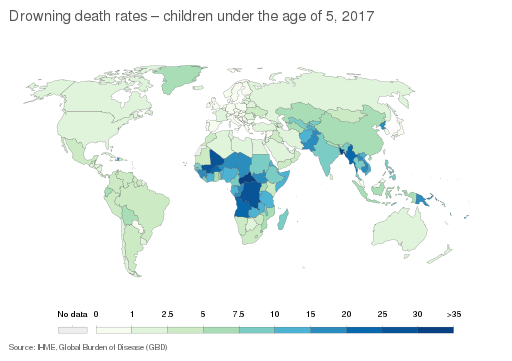
Drowning is responsible for at least half a million deaths annually worldwide with a disproportionate representation of low to middle income countries, which, when combined, account for >90% of all drowning fatalities. [3-5] Demographic risk factors for drowning incidents in the United States include male gender and white race, with younger age and lower socioeconomic status associated with a higher risk of mortality. [6,7]
Generally, there is a bimodal age distribution of deaths. First are the children under 5 years old where drowning occurs when they are unsupervised in tubs or pools. Then again at ages 15-30 years old we see patients who were recreationally swimming at the time of drowning, including those at beaches, lakes, and rivers. As may be expected, >50% of adult drowning deaths involve alcohol consumption. You will often also see these patients have hypothermia, concomitant trauma, and even seizures. [4] It is important to note that less than 10% of pediatric cases are related to child abuse or neglect. [8]
Pathophysiology
When we think of drowning the first thought is often how it affects the lungs, specifically oxygen exchange during respiration. Importantly, in addition to this, detrimental effects on the brain, heart, and metabolic system are important to understanding how to manage these emergencies. Understanding how not only the characteristics of the patient but qualities of the water itself can have a role in drowning pathophysiology and how the patient presents, specifically pertaining to the type (fresh or salt) and temperature.
The amount of water aspirated also plays a role. During a drowning episode, the initial panicking behavior of the patient causes a loss of normal breathing patterns and a physical struggle by the patient to stay above water. Once the patient is either submerged (under the water’s surface) or immersed (water splashed on the face) they often aspirate fluid. The involuntary inspiratory effort of fluid causes hypoxemia, quickly progressing to loss of consciousness and apnea. Reflex laryngospasm occurs when water hits the lower respiratory tract but is terminated with onset of significant cerebral hypoxia. This whole process usually happens in a matter of seconds to minutes. [4,9,10]
In the past, the theoretical pathophysiological differences between salt and freshwater drowning were stressed: hypertonic salt water was thought to cause more pulmonary edema and hypertonicity in serum as it drew plasma in to the pulmonary interstitium and alveoli whereas fresh water would easily pass through the lungs into the vasculature causing volume overload and electrolyte dilution. Now we know that this is more relevant to the pathologist for drowning victim autopsy cases. Instead, the most important factor in patients who survive to time of rescue is that both salt and freshwater drowning destroy surfactant with similar efficacy; the resultant fluid shifts of this causing noncardiogenic pulmonary edema and ARDS. [11] Although hyponatremia and hypernatremia have been reported in deaths following the ingestion of large amounts (≥22ml/kg) of fresh or salt water respectively, there should be no major electrolyte abnormalities unless significant hypothermia is present, or these disturbances were pre-existing. [12]
The initial cardiac rhythms in drowning patients can range from sinus tachy/bradycardia, atrial fibrillation, and ventricular tachycardias. Arrhythmias and/or ischemia also occur depending on the degree of hypoxemia and any concomitant hypothermia.
A major cause in morbidity and mortality from drowning is the aforementioned cerebral hypoxia. This causes cerebral edema and elevated intracranial pressures. Approximately 20% of downing victims sustain an initial neurologic insult, which can go on to limit full recovery. [13] In some cases, especially in prolonged immersion, the co-occurring hypothermia before asphyxiation may actually be neuroprotective for this reason.
On Scene Management
Initial management should include immediate removal of the patient from the water. Even doing a pulse check while the patient is in the water is wasted time as effective compressions cannot take place until the patient is on a firm and stable surface. When removing the patient from the water, rescuers should try to maintain the patient in a position that keeps the airway open and prevents emesis and further aspiration.
The method of removal has been discussed as potentially impacting patient outcomes. Many organizations advocate for Horizontal Extraction. One reason this is advised with a victim immersed in body-temperature water; cardiac output will be increased due to the pressure of the surrounding water. If the patient is removed from the water in a vertical position, this additional peripheral resistance is suddenly lost, leading to venous pooling and circulatory collapse. There are other theories of why this “circum-rescue collapse” can occur, but all theories eventually lead to circulatory collapse though a loss of cardiac filling. This is why it is most often suggested to remove the patient from the water in a horizontal position if prolonged immersion is known or suspected.[14,15] Once on land, the patient can be laid supine with the head and chest at the same level, parallel to the ground. If the patient is breathing but unconscious, they can be placed in the recovery position, lateral decubitus. [16]
Bystander intervention and early breaths significantly improves survival.[17] During on scene management, rather than focusing on CAB (circulation, airway, breathing), start with ABC (airway, breathing, circulation) as rescue breathing needs to start as soon as safely possible. This is because in drowning this is likely a respiratory (hypoxic) arrest. If the patient does not respond to two to five well-delivered rescue breaths, immediately begin CPR following BLS/ACLS pathways, including applying an AED to the patient. Remember, an AED is a contained electrical system, but water will conduct the electrical output - if the patient is in a puddle, do not shock them with you or anyone else in that puddle as well.[10]
Importantly, management does not include things often seen in popular entertainment or that were done historically. The Heimlich maneuver and other postural draining techniques to remove water have no role in management and just increase risk to the patient of further aspiration. All drowning victims are treated as trauma patients. Unless there is evidence on your clinical exam of relevant trauma (or the patient had a witnessed dive into shallow water) c-spine immobilization is not indicated and will only interfere with airway management.[18]
At first opportunity apply 100% FiO2 supplemental oxygen to all drowning victims while your assessment and initial resuscitation takes place. This can always be titrated down later to treat hypoxemia while avoiding hyperoxia. As with most resuscitations, intubation should be emergently performed in anyone who cannot protect their airway, is apneic, and/or cannot maintain PaO2>90% despite high flow oxygen device. If there is no need to emergently intubate, titrate supplemental O2 to maintain SpO2>94%. When considering NIPPV, remember that victims of drowning tend to swallow high volumes of water increasing their risk for emesis, either spontaneous or triggered by resuscitation efforts.[9]
Emergency Department Management & Disposition
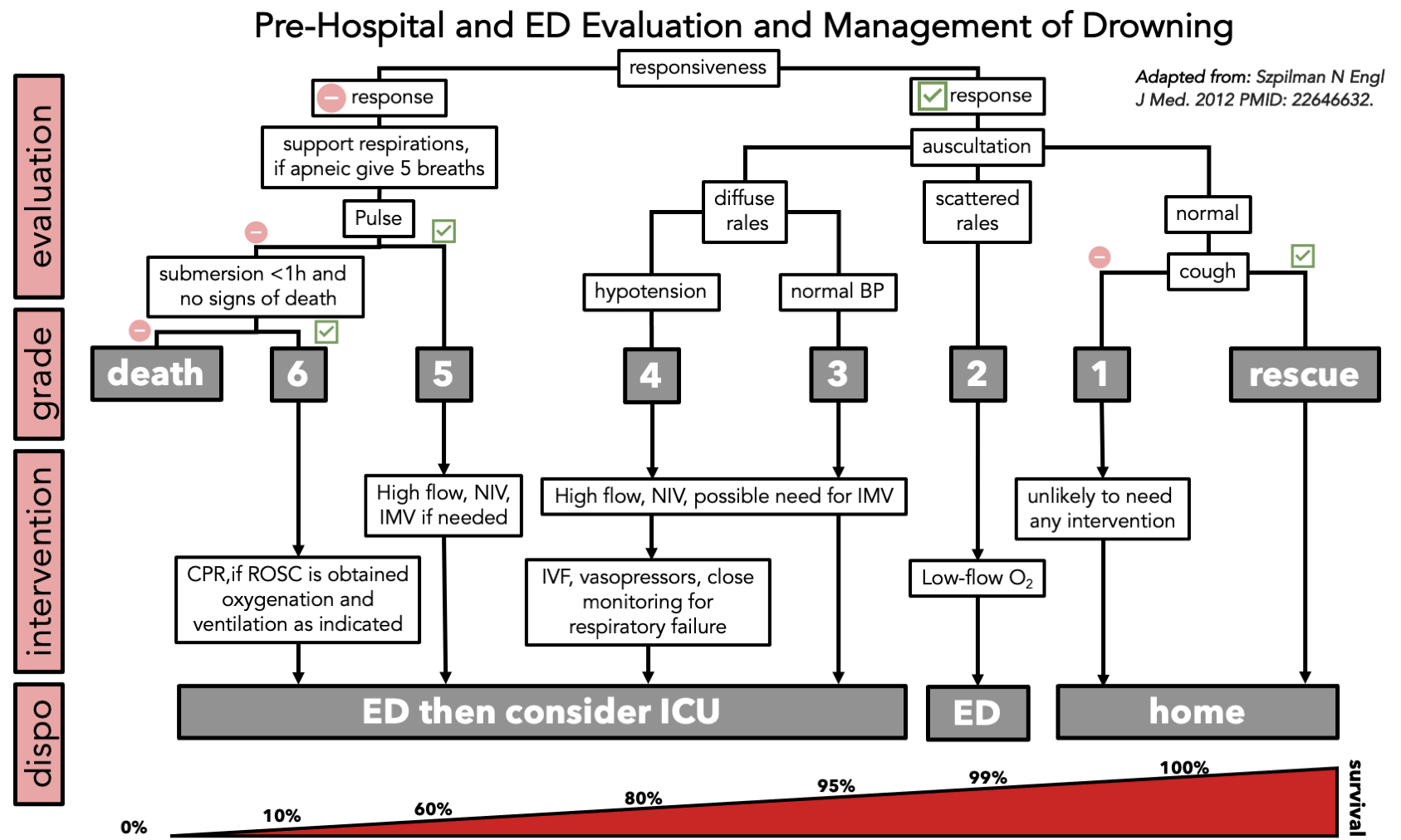
Over 75% of drowning victims make a full recovery, with ~6% suffering any residual neurologic deficits. Red flags on initial assessment in order of increasing concern include cough, rales, hypotension, and pulselessness. Significant factors effecting outcomes are generally the same as for cardiac arrest patients: time to CPR >10min, duration of resuscitation efforts >25min, age >14 years, GCS <5, persistent apnea, pH<7.1. Specific to drowning, duration of submersion is the most important factor for survival outcomes and is linked to considerably increased mortality if this time was greater than 5 minutes. [10,22] The grades of drowning severity and the associated management can be seen in the figure above.
While management of a severe drowning presentation is important to know, in the United States, most commonly it is asymptomatic patients who present alert after a drowning event. Despite lack of symptoms, all of these patients deserve an initial CXR looking for evidence of aspiration, pulmonary edema, or segmental atelectasis that can suggest the presence of a foreign body such as in sand aspiration. Consider repeat CXRs if the patient develops new signs or symptoms, such as a drop in pulse oximetry.
Bronchospasm is a common, late complication of drowning and can be treated with bronchodilators. Steroids have not been found to be beneficial in routine drowning patients [19]. Post-drowning pneumonia is a different phenomenon not to be covered in full here but, in general, prophylactic antibiotics are only indicated to prevent pulmonary infection post-drowning if the patient was submerged in grossly contaminated water (ie: sewage). In both cases of grossly contaminated water and for post-drowning pneumonia, antibiotic coverage should be tailored for waterborne pathogens such as pseudomonas & proteus [20,21].
After at least 6 hours of observation, patients can be safely discharged home if there is a reliable history of a minor event, no evidence of significant traumatic injury, no alterations in mental status, and no evidence of bronchospasm, dyspnea, or inadequate oxygenation. In special more risky populations such as elderly or underlying conditions that increase the risk of hypoxic injury, the observation period can be prolonged, either in the ED or on an inpatient floor. Prolonged observation is also appropriate for those with mild respiratory symptoms without hypoxia that improve while in the ED and no indication of respiratory abnormalities (i.e. normal ABG, O2 saturation, and CXR).
Patients with mild to moderate hypoxemia that is easily corrected with non-positive pressure supplemental oxygen should be admitted to the hospital to monitor for further complications. Finally, any patient who requires supplemental oxygen beyond low-flow and remains symptomatic needs ICU level of care. The goal of ICU care is to prevent secondary neurologic injuries due to ongoing ischemia, cerebral edema, hypoxemia, fluid & electrolyte imbalances, acidosis, and/or seizure.
Overall, the management of these patients focuses on removal from the body of water, cardiopulmonary support as needed, supplemental oxygen, and observation. The vast majority of patients will improve without lasting deficits, but the initial management can significantly impact outcomes especially in the most severe cases.
AUTHORED BY Marlena Wosiski-Kuhn MD PHD
Dr. Wosiski-Kuhn is a PGY-2 Emergency Medicine resident at the University of Cincinnati
Posted BY Christopher Zalesky MD MSc
Dr. Zalesky is a PGY-3 Emergency Medicine resident at the University of Cincinnati
Faculty Editor Conal Roche MD
Dr. Roche is an Assistant Professor of Emergency Medicine at the University of Cincinnati, Fellowship trained in Wilderness Medicine
References
1. 2015 revised Utstein-style recommended guidelines for uniform reporting of data from drowning-related resuscitation: An ILCOR advisory statement. Idris, A H, et al. 7, 2017, Resuscitation, Vol. 20.
2. Recommended guidelines for uniform reporting of data from drowning: the “Utstein style.”. Idris, A H, et al. 2003, Circulation, pp. 2565–257.
3. Systematic review of definitions for drowning incidents. Papa, L, Hoelle, R and Idris, A. 3, 2005, Resuscitation, Vol. 65, pp. 255-64.
4. Drowning: a review of epidemiology, pathophysiology, treatment and prevention. Salomez, F and Vincent, J L. 2004, Resuscitation, pp. 63-261.
5. Peden, M, McGee, K and Sharma, K. The injury chart book: a graphical overview of the global burden of injuries. Geneva : World Health Organization, 2002.
6. Drowning injuries in the United States: Patient characteristics, mortality risk, and associated primary diagnoses. Ryan, K M, et al. 11, 2020, Injury, Vol. 51, pp. 2560-2564.
7. Submersion injuries in the United States: Patients characteristics and predictors of mortality and morbidity. El Sibai, R, Bachir, R and El Sayed, M. 3, 2018, Injury, Vol. 49, pp. 543-548.
8. Submersion injuries in children and adults. DeNicola, L K, et al. 3, 1997, Crit Care Clin, Vol. 13, pp. 477-502.
9. Drowning. Rescue, resuscitation, and reanimation. Orlowski, J P and Szpilman, D. 3, 2001, Pediatr Clin North Am, Vol. 48, pp. 627-46.
10. Drowning. Szpilman, D, et al. 2012, N Engl J Med.
11. Near drowning: consensus and controversies in pulmonary and cerebral resuscitation. Gonzalez-Rothi, R J. 5, 1987, Heart & Lung : the Journal of Critical Care, Vol. 16, pp. 474-482.
12. Electrolyte changes in human drowning victims. Modell, J H and Davis, J H. 4, 1969, Anesthesiology, Vol. 30, p. 414.
13. Drowning. Modell, J H. 1993, N Engl J Med, pp. 253-6.
14. Rescue lifting system (RLS) might help to prevent death after rescue from immersion in cold water. Rollnik, J D, et al. 1, Jan 2001, Int J Sports Med, Vol. 22, pp. 17-20.
15. Wilderness Medical Society Clinical Practice Guidelines for the Out-of-Hospital Evaluation and Treatment of Accidental Hypothermia: 2019 Update. Dow, J, et al. 4S, Dec 2019, Wilderness Environ Med, Vol. 30, pp. S47-S69.
16. Szpilman, D and Handley, A J. Positioning of the Drowning Victim. [book auth.] J Bierens. Handbook of Drowning. Berlin : Springer, 2014, pp. 629-633.
17. The role of bystanders during rescue and resuscitation of drowning victims. Venema, A M, Groothoff , J W and Bierens, J J.4, 2010, Resuscitation, Vol. 81, pp. 434-9.
18. Cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Vanden Hoek, T L, et al. 2010, Circulation, pp. S829–S861.
19. Submersion and asphyxial injury. Ibsen, L M and Koch, T. 2002, Crit Care Med, pp. S402-S408.
20. Incidence and Consequences of Near-Drowning-Related Pneumonia-A Descriptive Series from Martinique, French West Indies. Cerland, L, et al. 11, 2017, Int J Environ Res Public Health, Vol. 14, p. 1402.
21. Pneumonia associated with near-drowning. Ender, P T and Dolan, M J. 1997, Clin Infect Dis, Vol. 25, pp. 896-907.
22. Long-Term Survival After Drowning-Related Cardiac Arrest. Reynolds, J C, et al. 2019, J Emerg Med, pp. 129-139.