Air Care Series: Burns Management
/History of Present Illness
Air Care 1 is dispatched for a scene flight involving a young male patient with extensive thermal burn injuries. In addition to his severe burns, the patient was reportedly hypoxic on a non-rebreather mask and tachycardic. Emergency Medical Services (EMS) at the scene reports that there are no known traumatic injuries. The patient is only able to vocalize his name, age, and that he has no known drug allergies. EMS has established an 18-gauge IV and administered one liter of normal saline.
Past Medical History:
unknown
Past Surgical History:
unknown
Family History:
unknown
Medications:
unknown
Allergies:
no known
Vitals:
HR 116 BP 118/60 RR 24 SpO2 97% on non-rebreather
Physical Exam:
The patient is an obese male who appeared his stated age, is ill-appearing, and smells of gasoline. He has full thickness burns to his face, head, neck, chest, abdomen, upper back, and upper and lower extremities. He has partial thickness burns of the remaining back and his genitals. He was awake with a Glasgow Coma Scale (GCS) of 15. Pupils were 3 mm bilaterally and reactive. He has carbonaceous material in his oral cavity. He was tachypneic with clear breath sounds bilaterally. He was tachycardic with a normal S1 and S2 without appreciable murmur. His central pulses were bounding. His abdomen is soft and not distended.
Prehospital Intervention:
Given the erythema, edema, and carbonaceous material in the patient’s airway, the air medical crew team was concerned about airway compromise and impending obstruction, and elected to proceed with endotracheal intubation in anticipation of complete airway obstruction. Ketamine and succinylcholine were used to facilitate rapid sequene intubation (RSI). The patient’s airway was secured via direct laryngoscopy on the first attempt sans hypoxia, and was confirmed with end-tidal capnography. The Air Care crew continued IV fluid resuscitation and rapidly transported the patient to the level 1 trauma center..
Hospital Course:
Upon arrival at the level 1 trauma center, the patient lost his only point of IV access during transport. Additional peripheral access was obtained and a femoral central venous line was placed. The patient’s total body surface area burned was estimated at 91%. Fluid resuscitation was initiated per the Parkland formula and the patient was admitted to the burns specialty care unit (BSCU). Escharotomies were performed at the bedside on the anterior torso, and the upper and lower extremities. Burn debridement and allografting was performed several times during the patient’s admission.
Discussion:
Thermal burn injuries are encountered frequently in the prehospital setting. According to the American Burn Association, there are approximately 486,000 patients treated annually for burn injuries. 40,000 patients are admitted annually for inpatient burn management, and 3,275 patients die from exposure to fire, flames, or smoke(1). Pre-hospital critical care providers must quickly gather information and begin appropriate therapeutic interventions while transporting these patients to definitive care.
Obtaining a history from a patient with severe burns is often difficult due to airway compromise or profound shock. Critical care transport providers should obtain collateral information and a pertinent history from ground EMS providers once the patient has been stabilized. Important historical elements include whether the patient was in an enclosed space, if there was any associated traumatic injury, or if there was any chemical component to the burn requiring decontamination. Any patients with burns to the face, hands, soles of the feet, genitals, or greater than 15 percent of total body surface area should be transported to a burn center.
The initial approach to the severely burned patient follows the ATLS algorithm and begins with the primary survey. Providers should place the patient on a continuous cardiac monitor, obtain large-bore IV access, and provide supplemental oxygen if necessary. IV access should be placed in healthy, non-injured skin (2). If IV access can only be obtained through burned skin, it must be well secured. Subcutaneous edema and weeping fluid from burned skin can easily displace the IV cannula. Sutures or staples can be used to prevent loss of access during transport.
A thorough airway assessment is critical in burned patients. In addition to determining patency, providers must investigate for the following:
Erythema, edema, or blistering of the neck, face, lips, and oropharynx
Carbonaceous material (soot) in the oropharynx
Singeing of facial or nostril hairs
Voice changes (3)
Patients with evidence of airway involvement often have associated inhalation injury. Inhalation injury includes supraglottic thermal injury, subglottic chemical injury, and systemic toxicity from products of combustion (4). Laryngeal edema may progress to complete airway obstruction within minutes of onset (5). Early endotracheal intubation should be performed if supraglottic structures are injured before laryngeal edema develop (4).
It can be difficult for critical care transport providers to determine when endotracheal intubation is indicated. Isolated singeing of facial hair and partial thickness facial burns with no oropharyngeal signs are not definitive indications for endotracheal intubation. It is reasonable to defer definitive airway intervention in these patients if the expected transport time is short. However, providers must remember that these physical exam findings are associated with occult inhalational injuries and these patients should be closely monitored during transit (6). Patients with oropharyngeal edema, vocal changes, severe face or circumferential neck burns should be intubated. In general, critical care transport providers should have a very low threshold to secure the patient’s airway with endotracheal intubation prior to the development of more significant edema and obstruction.
A burned airway should always be considered a difficult airway (6). Providers should have their backup plans and rescue devices immediately available. An endotracheal introducer such as a bougie should be considered early to maximize first past success (7). Video laryngoscopy can help navigate edematous and distorted airway anatomy. A supraglottic device can be used as a rescue device if an endotracheal tube cannot be secured. An “awake look” with topical anesthesia and procedural sedation with ketamine would be an excellent approach to this difficult airway. Unfortunately, this may not be possible given the limited resources in the pre-hospital setting. Surgical cricothyrotomy should be performed if orotracheal intubation is not possible and the patient cannot be oxygenated or ventilated by other means, such as an LMA.
Figure 1: chest wall escharotomy
Once the patient’s airway has been assessed and intervened upon as necessary, providers should move on to the next portion of the primary survey. Two specific findings should be considered during assessment of the patient’s respiration. First, patients that have sustained circumferential full thickness burns of the chest can develop an eschar. An eschar is comprised of leathery, inelastic burned skin (3). Edema forms beneath the eschar due to both the burn itself and crystalloid resuscitation. This will restrict ventilation and manifests clinically as difficult bag-mask ventilation or high peak pressures on the ventilator. When ventilation is inhibited by eschar, an escharotomy is indicated to improve respiratory biomechanics. Escharotomy is a surgical procedure where incisions are made through the eschar to the depth of the subcutaneous fat. Most escharotomies are performed two to six hours after a burn injury. There are multiple methods to perform chest wall escharotomies. The most common method for critical care transport providers begins with incisions from the clavicle to the costal margin in the anterior axillary line bilaterally. These incisions can then be connected by a transverse incision across the costal margin as shown in Figure 1. Full thickness burns are insensate, so no anesthesia is needed. Silver nitrate can be used for hemostasis of the incisions, and the wounds should be loosely packed with saline-soaked sterile gauze (8).
The second important component of respiratory management is to utilize a lung protective ventilation strategy. Approximately half of intubated burned patients admitted to burn centers develop acute respiratory distress syndrome (ARDS) (9). Lung protective ventilation has a proven mortality benefit in ARDS (10). This strategy avoids barotrauma by setting the tidal volume at 6-8 mL/kg of ideal body weight and keeping plateau pressures less than 30 cmH2O. Providers should use a PEEP scale to rapidly titrate PEEP and FiO2 to a goal oxygen saturation of 88-95% (11). The exception to this rule is if there is a suspected carbon monoxide inhalation, in which case the FiO2 should be kept at 100%.
Burned patients have an overwhelming systemic inflammatory response. There is increased secretion of catecholamines, cortisol, glucagon, renin-angiotensin, antidiuretic hormone, and aldosterone. Fluid and proteins are lost in the burned tissue. All of these changes can lead to profound intravascular hypovolemia and vasodilation resulting in hypotension.
Once IV access has been obtained and the patient’s hemodynamics have been addressed, providers should complete a thorough exam for circumferential extremity burns, which can cause compartment syndrome. A significant amount of pressure can develop posterior to a circumferential burn from edema below the inelastic, burned skin. This will result in irreversible nerve and muscle injury if not addressed quickly. Compartment syndrome from a burn is treated with escharotomy as opposed to fasciotomy in traditional compartment syndrome. Limb escharotomy is not routinely performed by critical care transport providers because it is not immediately life-threatening. Compartment syndrome typically develops over the course of hours once the patient has arrived at the burn center.
Providers should then begin a focused neurologic assessment. This is especially important with patients that have sustained additional traumatic injuries from motor vehicle accidents or blast injuries. Confusion and altered mental status may also be secondary to carbon monoxide (CO) or hydrogen cyanide (CN) inhalation.
Carbon monoxide poisoning is a well-known sequelae of smoke inhalation injury. Adult hemoglobin has a much higher affinity for CO than oxygen, causing a relative hypoxemia. Symptoms of CO poisoning include flushing of the skin, headache, vomiting, and altered mental status. All patients with suspected CO exposure should receive 100% oxygen and should be evaluated for hyperbaric oxygen therapy. Indications for hyperbaric oxygen therapy include carboxyhemoglobin levels >25% for adults (>15% in pregnant women), altered mental status, coma, seizure, or other focal neurological deficit (3).
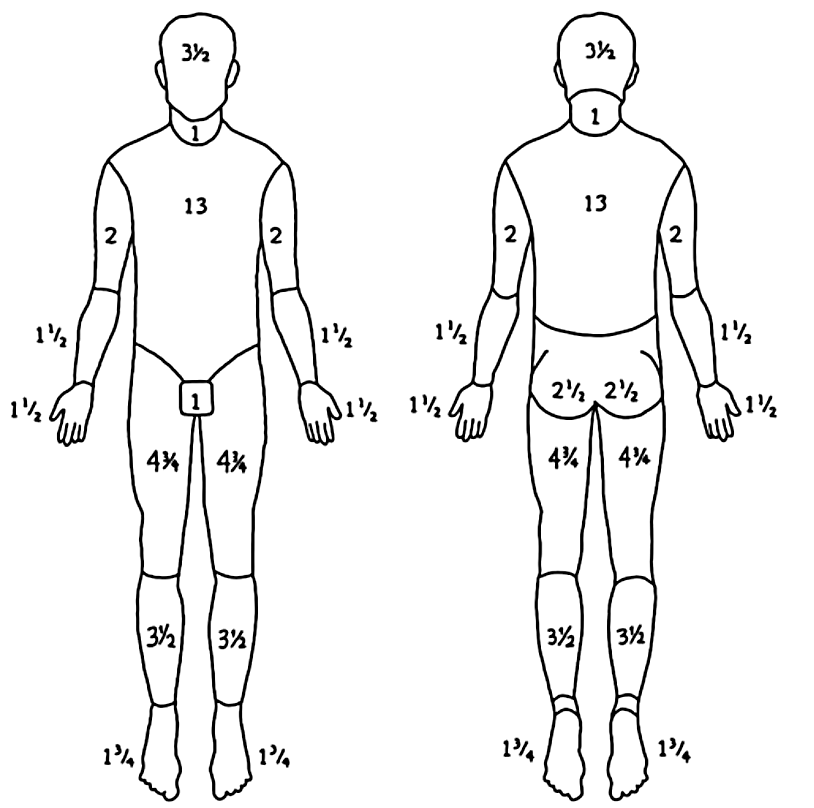
Figure 2: Lund-Browder diagram
Hydrogen cyanide is formed by the combustion of nitrogen-containing polymers found in upholstery and insulation such as wool, silk, polyurethane, and vinyl. CN uncouples mitochondrial oxidative phosphorylation and causes profound tissue hypoxia. CN toxicity presents with dyspnea, loss of consciousness, seizures, altered mental status, and hemodynamic instability (3). Hydroxocobalamin (Cyanokit) is carried by Air Care and is the antidote for cyanide toxicity. It is a natural form of Vitamin B12 and binds CN, forming cyanocobalamin which is excreted renally. Providers should administer this to any patient with an enclosed space inhalational injury and altered mental status, hemodynamic instability, or unexplained lactic acidosis.
Before packaging the patient for transport, providers should remove all burning, hot, or singed clothing. Rings, watches, jewelry, and belts should also be removed to prevent a tourniquet-like effect (3). The extent and degree of the burned skin should also be assessed prior to transport.
Burns are classified based on their depth. Superficial burns affect the epidermis and cause erythema that is painful without blistering, similar to a sunburn. Partial thickness burns affect the dermis. They are split into superficial partial thickness and deep partial thickness burns. Deep partial thickness burns do not blanch as opposed to superficial partial thickness burns. Second degree burns are very painful and cause blistering. Full-thickness burns affect the entire dermis; the skin is insensate and appears charred and leathery. Full thickness burns can affect deeper structures including fat, muscle, and bone (3).
Providers should attempt to estimate the total body surface area affected by second and third degree burns. Various methods exist to help with this calculation. The “rule-of-nines” is the most common in the prehospital environment. This calculation needs to be adjusted in infants and children due to their proportionally larger heads and smaller legs. It is important to remember that the “rule-of-nines” often overestimates the total area of burned skin. Another method is to use the dorsal surface of the patient’s hand as 1% to estimate the total extent of burns on the body. Finally, a Lund-Browder diagram may be filled out and is what is typically used by burn surgeons. This has been shown to be very precise and adjusts for age, and the figure above shows how to calculate this (3).
Burned patients have very high insensible fluid losses and often require significant crystalloid resuscitation. The Parkland formula is the most common method used for calculating fluid requirements in burned patients. The amount of crystalloid required in the first 24 hours can be calculated using the formula below:
Half of this volume is given over the first 8 hours and the second half is given over the subsequent 16 hours. Balanced isotonic solutions, such as lactated ringers or normosol, should be used.
While these patients often require very large volumes of crystalloid, they can easily be over-resuscitated. In the year 2000, Pruitt first described “fluid creep,” which was coined to demonstrate the harmful side effects of over-resuscitation with crystalloid. Burned patients who received too much crystalloid can develop abdominal compartment syndrome and pulmonary edema (1,2). Over resuscitation and “fluid creep” continue to occur as demonstrated by several published retrospective cohort studies (1,3).
The Parkland formula should be used in prehospital burn management to estimate fluid requirements and serve as a starting point. Providers should then use hemodynamic response and urine output as resuscitation guides, and hourly fluid rates can be adjusted as needed. The goal urine output should be 0.5 - 1.0 mL/kg/hr in adults with normal baseline renal function. Critical care transport providers should initiate fluid resuscitation but should be judicious with fluid boluses to prevent complications from over-resuscitation.
Severely burned patients can be intimidating for even the most seasoned critical care transport providers. These patients often require aggressive resuscitation and multiple procedures in a relatively short period of time. It is often easy for providers to become overwhelmed, necessitating an algorithmic approach to the patient, similar to traumatically injured patients. By advancing through the primary survey and stabilizing the patient while starting aggressive but goal directed crystalloid resuscitation, critical care transport providers can bring ICU level care to one of the sickest pre-hospital patient populations.
Article by Shaun Harty, MD
expert review by Steven C. Carleton, MD, PhD
References:
Burn incidence and treatment in the United States: 2016 fact sheet, American Burn Association.
Stapczynski, J. Stephan., and Judith E. Tintinalli. Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 8th Edition. New York: McGraw-Hill Education, n.d. Print.
Roberts, James R, Catherine B. Custalow, Todd W. Thomsen, and Jerris R. Hedges. Roberts and Hedges' Clinical Procedures in Emergency Medicine, 6th Edition. Chapter 38, pages 758-787, 2014. Print.
ARDSNet. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N Engl J Med 2000; 342:1301-1308