Caustic Skin Injuries
/WHY DO WE CARE ABOUT CAUSTIC SKIN INJURIES?
Chemical burns come with complications that thermal burns do not. Specifically:
Chemical burns are more likely to involve prolonged exposure, both before ED arrival and throughout hospital stay (1).
The human body protects against continued protein denaturation in thermal burns through immediate and irreversible protein coagulation. In chemical burns, protein denaturation does not halt, but instead continues through hydrolysis (1).
Chemical burns cause systemic effects, including distant organ damage and electrolyte abnormalities, which can in turn cause fatal cardiac arrhythmias.
Almost all chemical burn patients require hospitalization. Das (2015) reports that 0.13% of the chemical burn patients studied were treated as outpatients, compared to over 50% of thermal burn patients.
Even when chemical burns and thermal burns are of similar size, hospitalization for chemical burns is 30% longer (2).
Close to 55% of chemical burns go on to require surgery (1).
Chemical burns produce more hypertrophic scarring than thermal burns; this can in turn lead to decreased quality of life and mental health decline (3).
Chemical burns are also an evolving pathology, with thousands of new chemicals added to the market each year (4). Since 2000, both assault and warfare with chemical weapons have increased, although these pathologies vary based on practice location (1). For instance, chemical burns can comprise up to 14% of burns in the developing world, compared to 3% in the US and Europe (2, 5). It is therefore important to understand your local chemical burn patterns, in much the same way providers learn local patterns of antibiotic resistance.
HOW DO THESE INJURIES OCCUR?
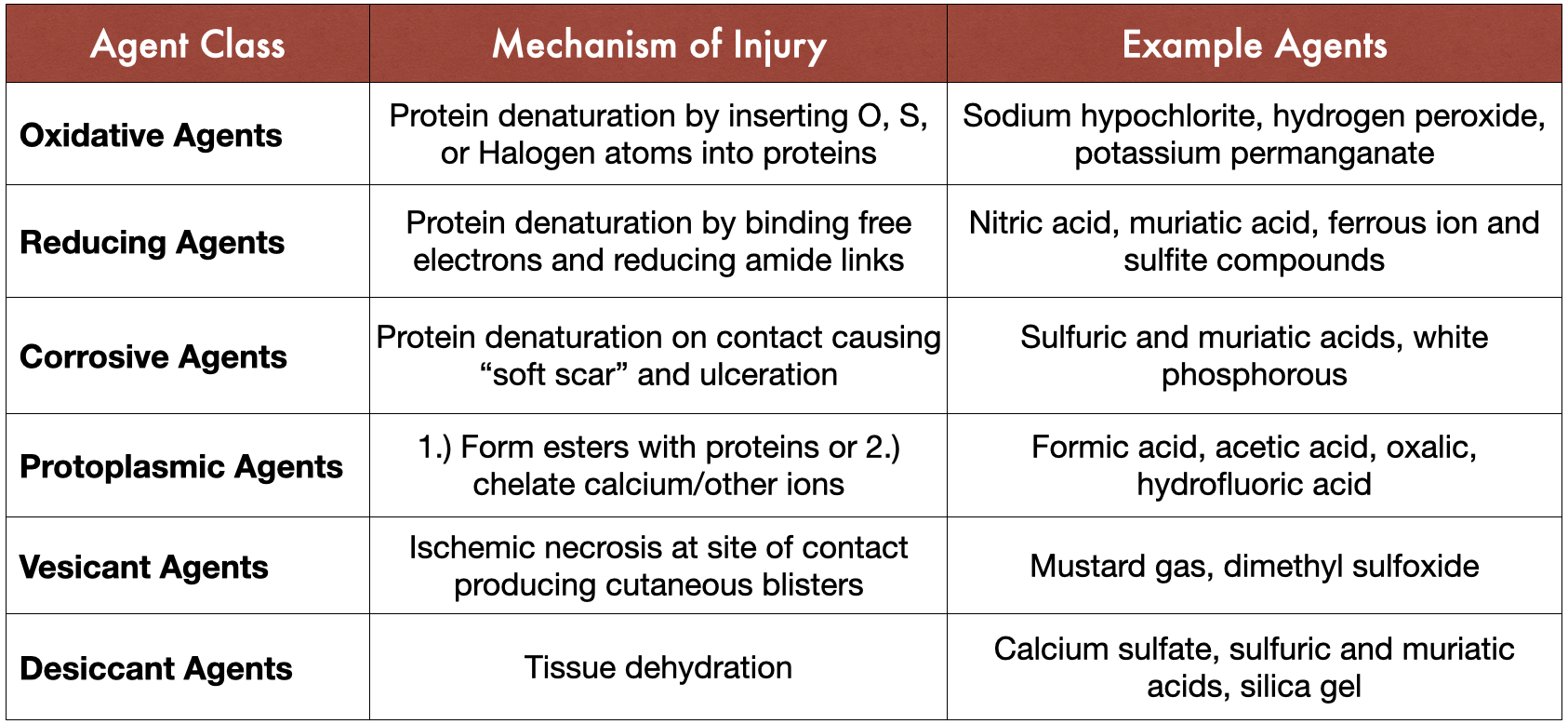
Not all chemicals are created equal, and the pathology behind chemical burns varies substantially. Dinis-Oliviera (2015) provides a thorough but concise summary which has been adapted into the table below:
Table 1: A classification of chemical agents leading to caustic skin injuries. Adapted from Dinis-Oliviera (2015).
Additional factors that contribute to the severity of the burn include the physical state of the chemical (solid, liquid, or gas), the concentration, the amount, and local skin characteristics. Skin already damaged by dermatitis, for example, is more susceptible to burn damage, whereas warts provide some protection. The single most important factor in determining burn severity is the duration of exposure (13).
HOW DO WE TREAT CHEMICAL BURNS?
There are 33,000 – 63,000 distinct chemical compounds classified as hazardous by the US government (4). Many of these chemicals are capable of causing caustic skin injuries. This is an intimidating problem. How can one person remember all the antidotes? How can one ED even STOCK the antidotes?
Fortunately, most caustic skin injuries can be treated by following a simple protocol, adapted from Herbert (1989) and Palao (2010):
SAFETY
STRIP
SHOWER
SIZE
SEDATE
STABILIZE
Systemic toxicity
Side effects
Special considerations
Silver sulfadiazine
Let’s take a closer look at each step:
1. SAFETY – The first step is making sure the scene is safe for you to enter. This includes any scene of a chemical accident, but also the ED itself. It is possible for patients to be transported without adequate decontamination. Once it is safe to assess the patient, all personnel should don gloves, eye shields, and plastic aprons (14).
2. STRIP – Remove all patient clothes. Chemical burns don’t care about modesty, and neither should you.
3. SHOWER – Recommendations for irrigation time range from 15 minutes to 12 hours. A reasonable compromise suggested by Cartotto et al. is 45-60 minutes in a hydrotherapy tank. Immediate irrigation leads to shorter hospital stays (6.2 days vs. 22 days) and decreased incidence in full-thickness burns, compared to delayed irrigation (15).
Of note, you should NOT immerse the patient in a bathtub or tank for irrigation. This is insufficient chemical dilution and can spread the chemical to previously uninjured parts of the patient’s body. It can also lead to nosocomial bacterial infection and electrolyte imbalances (1, 14).
4. SIZE – You should attempt to estimate burn size and depth, in order to calculate medication doses and to communicate with other providers. This is easier said than done, particularly in chemical burns, where the burn depth is often much deeper than estimated. Always err on the side of overhydration, using urine output as your guide (14).
5. SEDATE – Like thermal burns, caustic skin injuries are excruciatingly painful. Patients should be given IV opioids or sedated for comfort.
6. STABILIZE
Systemic toxicity – several chemicals are associated with systemic toxicity (see Part Four). In these cases, serial electrolyte monitoring and telemetry for 24-48 hours is key. Patients may require dialysis (16).
Side effects – many chemicals that damage the skin also damage the respiratory tract and eyes. Careful physical examination and repeat assessment are a must.
Special considerations – several chemical substances have unique recommended treatments or should not be irrigated with water. See Part Four for more information.
Silver sulfadiazine – this is generally the recommended topical dressing after sufficient irrigation (14).
Neutralize – this doesn’t start with an S. Don’t do it. Neutralization of a chemical exposure (for instance, applying an alkali to neutralize an acid) can cause an exothermic reaction, or secondary tissue damage from the neutralizing agent. There’s also concern that irrigation may be delayed while providers search for antidotes (1, 14).
SPECIFIC CHEMICALS
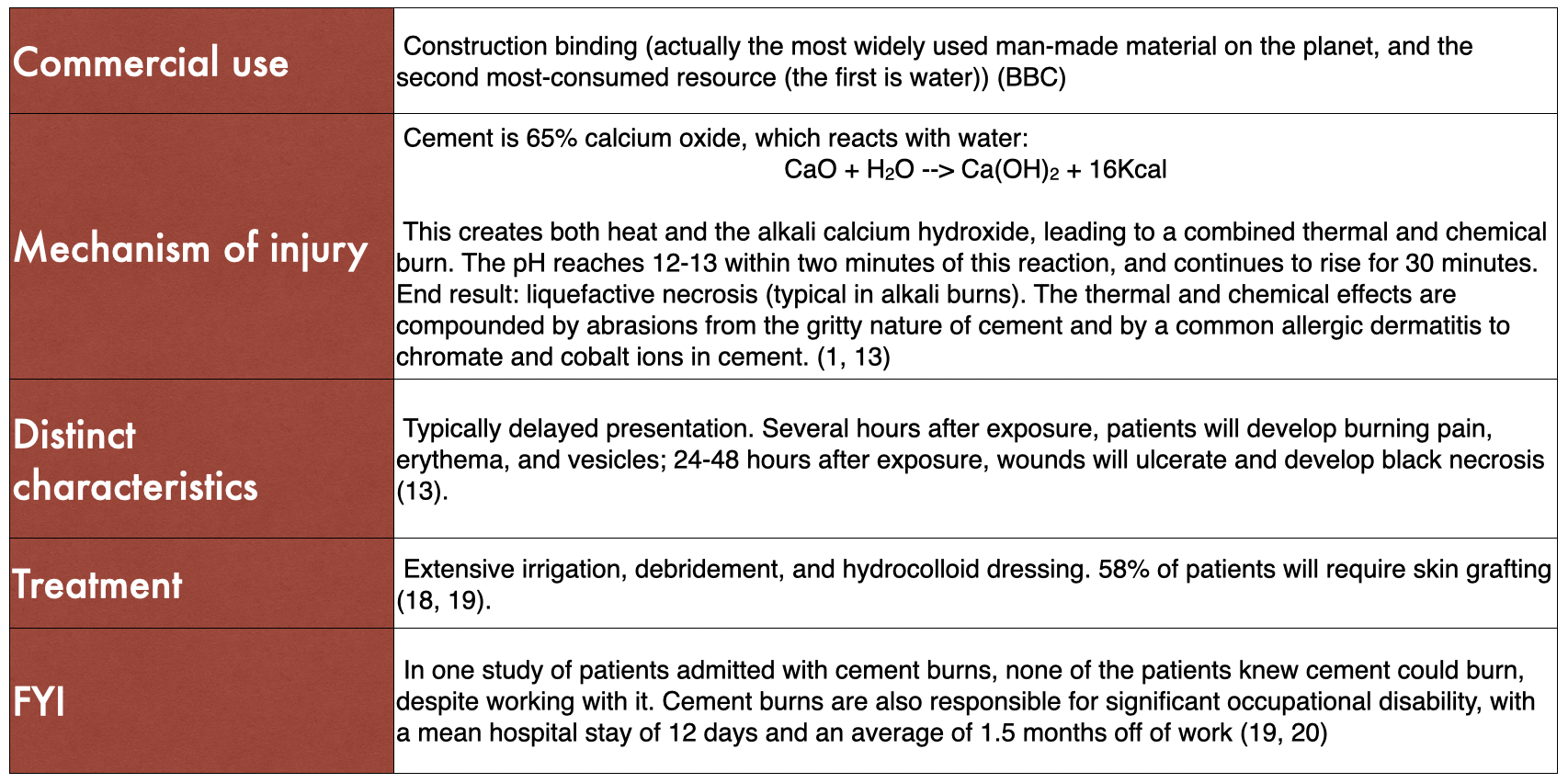
CEMENT
Hydrofluoric Acid
Phenol
White Phosphorous
References
1. Palao, R., Monge, I., Ruiz, M., & Barret, J. P. (2010). Chemical burns: Pathophysiology and treatment. Burns, 36(3), 295–304. https://doi.org/10.1016/j.burns.2009.07.009
2. Eldad, A., Weinberg, A., Breiterman, S., Chaouat, M., Palanker, D., & Ben-Bassat, H. (1998). Early nonsurgical removal of chemically injured tissue enhances wound healing in partial thickness burns. Burns, 24(2), 166–172. https://doi.org/10.1016/S0305-4179(97)00086-7
3. Das, K. K., Olga, L., Peck, M., Morselli, P. G., & Salek, A. J. M. (2015). Management of acid burns: Experience from Bangladesh. Burns, 41(3), 484–492. https://doi.org/10.1016/j.burns.2014.08.003
4. Barillo, D. J., Cancio, L. C., & Goodwin, C. W. (2004). Treatment of white phosphorus and other chemical burn injuries at one burn center over a 51-year period. Burns, 30(5), 448–452. https://doi.org/10.1016/j.burns.2004.01.032
5. Hall, A. H., Mathieu, L., & Maibach, H. I. (2018). Acute chemical skin injuries in the United States: A review. Critical Reviews in Toxicology, 48(7), 540–554. https://doi.org/10.1080/10408444.2018.1493085
6. Ye, C., Wang, X., Zhang, Y., Ni, L., Jiang, R., Liu, L., & Han, C. (2016). Ten-year epidemiology of chemical burns in western Zhejiang Province, China. Burns, 42(3), 668–674. https://doi.org/10.1016/j.burns.2015.12.004
7. Agbenorku, P., Akpaloo, J., Chirurgie, F., Aboah, K., Klutsey, E., Hoyte-Williams, P. E., Farhat, B., Turkson, E., Yorke, J., Chirurgie, F., Ametih, R., & Hussey, R. (2015). Chemical Burn Injury in Kumasi: The Trend and Complications following and Their Management. Plastic and Reconstructive Surgery - Global Open, 3(10), e548. https://doi.org/10.1097/GOX.0000000000000519
8. Tan, T., & Wong, D. S. Y. (2015). Chemical burns revisited: What is the most appropriate method of decontamination? Burns, 41(4), 761–763. https://doi.org/10.1016/j.burns.2014.10.004
9. Akhtar, M. S., Ahmad, I., Khurram, Mf., & Kanungo, S. (2015). Epidemiology and outcome of chemical burn patients admitted in burn unit of JNMC hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India: A 5-year experience. Journal of Family Medicine and Primary Care, 4(1), 106. https://doi.org/10.4103/2249-4863.152265
10. Abbasi, H., Dehghani, A., Mohammadi, A. A., Ghadimi, T., & Keshavarzi, A. (2021). The Epidemiology of Chemical Burns Among the Patients Referred to Burn Centers in Shiraz, Southern Iran, 2008–2018. Bulletin of Emergency And Trauma, 9(4). https://doi.org/10.30476/beat.2021.90754.1261
11. Koh, D.-H., Lee, S.-G., & Kim, H.-C. (2017). Incidence and characteristics of chemical burns. Burns, 43(3), 654–664. https://doi.org/10.1016/j.burns.2016.08.037
12. Hardwicke, J., Hunter, T., Staruch, R., & Moiemen, N. (2012). Chemical burns – An historical comparison and review of the literature. Burns, 38(3), 383–387. https://doi.org/10.1016/j.burns.2011.09.014
13. Dinis-Oliveira, R. J., Carvalho, F., Moreira, R., Proença, J. B., Santos, A., Duarte, J. A., Bastos, M. de L., & Magalhães, T. (2015). Clinical and forensic signs related to chemical burns: A mechanistic approach. Burns, 41(4), 658–679. https://doi.org/10.1016/j.burns.2014.09.002
14. Cartotto, R. C., Peters, W. J., Neligan, P. C., Douglas, L. G., & Beeston, J. (1996). Original Article Article original. 39(3).
15. Chai, H., Chaudhari, N., Kornhaber, R., Cuttle, L., Fear, M., Wood, F., & Martin, L. (2022). Chemical burn to the skin: A systematic review of first aid impacts on clinical outcomes. Burns, 48(7), 1527–1543. https://doi.org/10.1016/j.burns.2022.05.006
16. Herbert, K., & Lawrence, J.C. (1989). Chemical burns. Burns, 15(6), 381 – 384. https://doi.org/10.1016/0305-4179(89)90103-4
17. Climate change: The massive CO2 emitter you may not know about—BBC News. (n.d.). Retrieved January 6, 2023, from https://www.bbc.com/news/science-environment-46455844
18. Machovcova, A. (2010). Caustic Ulcers Caused by Cement Aqua: Report of a Case. Industrial Health, 48(2), 215–216. https://doi.org/10.2486/indhealth.48.215
19. Boyce, D. E., & Dickson, W. A. (1993). Wet cement: A poorly recognized cause of full-thickness skin burns. Injury, 24(9), 615–617. https://doi.org/10.1016/0020-1383(93)90126-Q
20. Poupon, M., Caye, N., Duteille, F., & Pannier, M. (2005). Cement burns: Retrospective study of 18 cases and review of the literature. Burns, 31(7), 910–914. https://doi.org/10.1016/j.burns.2005.04.007
21. Sanz-Gallen, P. (2001). Hypocalcaemia and hypomagnesaemia due to hydrofluoric acid. Occupational Medicine, 51(4), 294–295. https://doi.org/10.1093/occmed/51.4.294
22. Caravati, E.M. (1988). Acute hydrofluoric acid exposure. Am J Emerg Med. 6(2):143 – 150. https://doi.org/10.1016/0735-6757(88)90053-8
23. Friedstat, J., Brown, D. A., & Levi, B. (2017). Chemical, Electrical, and Radiation Injuries. Clinics in Plastic Surgery,44(3), 657–669. https://doi.org/10.1016/j.cps.2017.02.021
24. Sheridan, R. L., Ryan, C. M., Quinby, W. C., Blair, J., Tompkins, R. G., & Burke, J. F. (1995). Emergency management of major hydrofluoric acid exposures. Burns, 21(1), 62–64. https://doi.org/10.1016/0305-4179(95)90785-X
25. Wedler, V., Guggenheim, M., Moron, M., Künzj, W., & Meyer, V. E. (2005). Extensive hydrofluoric acid injuries: A serious problem. The Journal of Trauma, 58(4), 852–857. https://doi.org/10.1097/01.ta.0000114528.15627.65
26. Barqouni, L. N. A., Skaik, S. I., Shaban, N. R. A., & Barqouni, N. (2010). White phosphorus burn. The Lancet, 376(9734), 68. https://doi.org/10.1016/S0140-6736(10)60812-4
Authorship
Written by: Ann Wolski, MD, PGY-1 University of Cincinnati Department of Emergency Medicine
Peer Review and Editing by Jeffery Hill, MD MEd, Associate Professor, University of Cincinnati Department of Emergency Medicine
Cite As
Wolski, A Hill, J. (January 11, 2023). Caustic Skin Injuries. TamingtheSRU. https://www.tamingthesru.com/blog/2023/1/11/caustic-skin-injuries