Whole Blood - More than the Sum of Its Components?
/Q: For a patient in hemorrhagic shock from acute blood loss, what is the best resuscitative fluid?
A: If they've lost blood, give them blood.
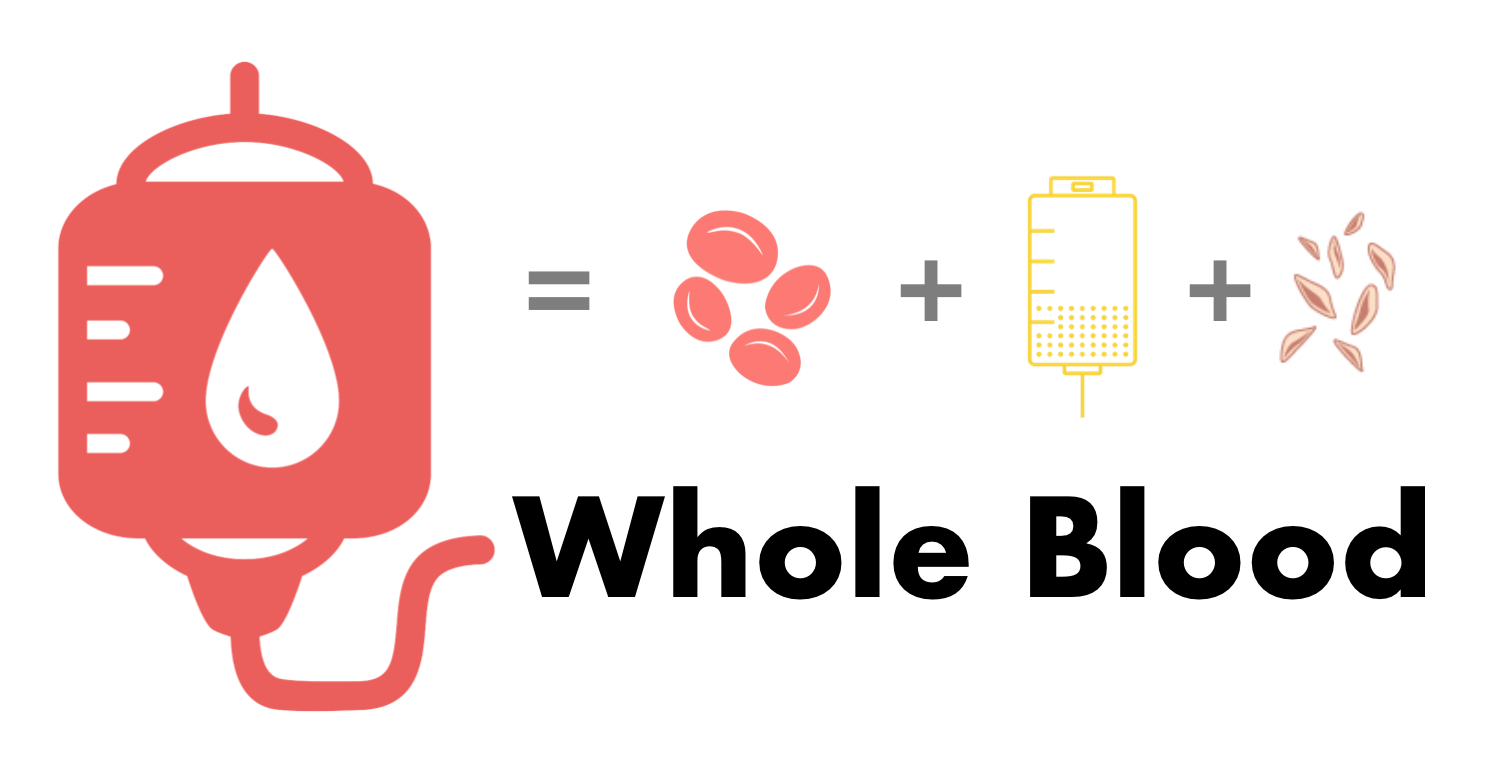
It's never quite that simple though right? For a generation now, we have practiced primarily by transfusing patient's with acute blood loss varying ratios of blood product components. Thanks to the PROPPR trial, we most recently arrived on a generally accepted ratio of 1:1:1 for Plasma, Platelets, and Red Blood Cells for severely injured bleeding trauma patients. Recent military literature however, suggests that there may be another strategy (which is in and of itself a bit of a throwback) that could offer additional benefits over a component transfusion strategy. If were are trying to recreate a whole blood with a 1:1:1 plasma:platelet:PRBC ratio, why not just give whole blood?
This retrospective analysis was conducted in a US Military population across 6 combat hospitals in Iraq and Afghanistan between January 2004 and October 2007. Patient’s transfused at least 1 unit RBCs met inclusion criteria for the study and were divided into 2 groups; those transfused warm fresh whole blood (WFWB), RBCs, and plasma but no aphaeresis platelets (aPLT) and those transfused component therapy (CT) of RBCs, plasma, and aPLT. Of note, RBCs transfused in this population were not leukoreduced as is standard practice in civilian blood banks. Primary outcomes were mortality at 24 hours and 30 days, and the authors hypothesized that patients transfused WFWB would have improved mortality at both time points.
To evaluate their primary outcomes, authors first compared raw survival between groups. They then performed univariate regression analysis of all patients to determine variables significantly associated with 30-day survival then developed a multivariate regression model to determine which variables had a significant independent effect on survival at 30 days. For the purposes of calculating total units of blood products transfused, 1 unit WFWB = 1 unit RBC + 1 unit plasma + 1 unit platelets. The authors also took into account the volume of anticoagulant/additive transfused with each type of blood product as these volumes are present in grater quantities in stored CT as opposed to WFWB. Additional variables considered included; Glasgow Coma Score (GCS), Injury Severity Score (ISS), temperature, systolic blood pressure, heart rate, hemoglobin, INR, and base deficit all measured at time of admission.
A total of 354 patients met inclusion criteria of which 100 (28%) were included in the WFWB group and 254 (72%) comprised the CT group. Baseline admission labs, vitals, and markers of injury severity were similar between groups, except temperature, which was slightly lower in the WFWB group. WFWB comprised approximately 30% of total blood volume transfused in the WFWB group. Total RBC transfused per group was similar as was plasma:RBC ratio. WFWB group was transfused significantly less anticoagulant/additive volume and total blood product volume as compared to CT. Both raw 24 hour and 30-day mortality were significantly lower in the WFWB group as compared to the CT group. However, renal failure was also more frequent in WFWB group with incidence of DVT and ARDS approaching significance.
Univariate analysis of all patients divided into survivors v non-survivors at 30 days demonstrated increased survival in patients receiving WFWB, higher plasma:RBC ratios, and lower volume anticoagulant/additive. Multivariate regression demonstrated significant positive effect of WFWB group and plasma:RBC ratio on 30-day survival. A second multivariate regression examining effects of administration of specific blood products regardless of treatment group demonstrated significant positive effect of WFWB and plasma on survival with a negative effect of RBC on survival at 30 days.
The authors conclude that transfusion strategies incorporating WFWB and higher plasma:RBC ratio may improve 30-day survival. They also posit that the negative effect on survival seen with RBC use was related to storage lesion as the average unit RBC was stored for 33 days and significant degradation of RBCs is known to occur between 14 and 21 days. While the retrospective nature of this study limits our ability to draw precise conclusions, the evidence provided does support the use of WFWB in traumatic resuscitation of a military population. However, the generalizability of these results to a civilian population remains unclear. Further study is required to determine whether WFWB would prove beneficial in a civilian population as well as whether WFWB administration is even feasible in the civilian setting.
This trial was a first of its kind and sought to investigate the feasibility of using of whole blood early in the resuscitation of severely injured civilian trauma patients. It was a single center, randomized, controlled trial that took place in a level 1 trauma center. The primary outcome of the study was whether or not resuscitation with modified whole blood (mWB) resulted in overall fewer transfusions as compared to resuscitation solely with traditional component therapy. Modified whole blood is a blood product that has undergone a leukoreduction process that also inactivates and/or removes platelets.
They enrolled patients 18 years of age and older who met the highest level of trauma activation and had active bleeding that required emergent transfusion. Patients were excluded if they received more than 4 units of uncrossmatched pRBC prior to randomization, CPR or a thoracotomy prior to randomization, religious objections to transfusions, DNR status, pregnant and incarcerated patients, and those with an “opt-out bracelet.” The authors added on three more exclusion criteria after their initial study approval in order to achieve “a more pragmatic design.” The first additional exclusion was for those patients too unstable to wait an additional 5-10 minutes for the first cooler of blood in order for blood typing to be performed. They also excluded patients with blood types B and AB due to lower resources for these transfusions. Finally, they excluded severe TBI patients during their data collection period.
Out of 1,695 patients screened, they were able to enroll and randomize 107 patients – 55 in the mWB group and 52 in the COMP group. The primary outcome was the quantity of blood product administered over the first 24 hours. Their secondary outcomes measured 24 hour and 30-day mortality, length of stay, transfusion-associated complications, and infections. Ultimately the investigators found no difference between the two groups in either of their primary or secondary outcomes. They then performed a secondary sensitivity analysis which excluded the previously enrolled severe TBI patients from the data set, and among this new study population, they did find that the quantity of product transfused over the first 24 hours was significantly lower among the mWB group as compared with COMP group by approximately 5 units of total transfusion (2u pRBC, 2u plasma, 1 dose of platelets).
This study certainly had some limitations. First, they had the potential for significant selection bias, enrolling only 109 of the original 1,695 patients screened. This makes the data somewhat challenging to apply to an undifferentiated trauma patient. This study also excluded the sickest patients who could not wait for blood typing in order to be enrolled. These unstable patients, perhaps, are the ones who might benefit most from the theoretical hemostatic benefit of the study product over component therapy. Another limitation was the actual study product used, which was a modified whole blood, and therefore not necessarily providing the same hemostatic potential of true whole blood (which retains platelets). This study was performed in 2013. Thanks to advances in technology, we now have platelet sparing leukoreduction filters available. It is possible that this technology will result in a leukoreduced whole blood product with more benefit than this study was able to demonstrate. This study also required a secondary sensitivity analysis with the exclusion of severe TBI patients in order to obtain statistically significant results. While this exclusion criterion is understandable, it further eliminates even more of the original enrollment numbers, leaving a fairly small cohort of 33 in the mWB group and 34 in the COMP group. Ultimately with these low numbers, this study was underpowered to truly detect any advantage in patient-centered outcomes of whole blood as compared to component transfusions. Nevertheless, whole blood does still seem potentially promising in the resuscitation of civilian trauma patients and deserves more research to elucidate its ideal implementation.
This was a single center trial where the researchers implemented a "change in practice" at their institution allowing for administration of up to two units of uncrossmatched, leukoreduced, low-titer, type O, cold whole blood. Their main purpose was to evaluate whether administration of this was feasible and safe in a civilian level 1 trauma center. Specifically, the authors hypothesized that there would be no increased risk of hemolytic transfusion reactions.
In this study, the researchers used low-titer, group O whole blood. They used male O+ blood donors with anti-A and anti-B titers less than 100 based on previous data suggesting increased transfusion reactions with titers above this level. The whole blood units were also leukoreduced in a platelet-sparing method resulting in two units available for use immediately for resuscitation of a trauma patient.
For the methods, eligible patients were male trauma patients with hypotension (defined as a systolic blood pressure less than 90) thought to be due to trauma. They also needed to meet at least two ABC criteria for massive transfusion (ED systolic BP less than or equal to 90, penetrating mechanism, ED heart rate greater than or equal to 120, and/or a positive FAST). If a patient met these criteria, they could be given up to the two units of whole blood and any subsequent blood product administration required according to their needs. The total outcomes measured were total blood products used in the first 24-hours, haptoglobin level (used as a marker of hemolysis), and transfusion reactions. They compared this to a databank of male trauma patients in the preceding two years before the study who had received at least one unit of packed red blood cells. They ultimately found that there was no statistically significant difference in total blood product administration. In general, haptoglobin levels were noted to be on the lower limit of normal in the whole blood group, but no hemolytic transfusion reactions were reported in either group.
While the generalizability of this study is limited because it is a single center cohort looking at only male trauma patients, it is somewhat of a landmark study demonstrating that administration of two units of uncrossmatched, leukoreduced, low titer type O whole blood does appear safe in this specific population of civilian trauma patients. For this to truly translate into everyday practice in the civilian setting, a multi-center randomized control trial is still needed. Nonetheless, the results of this small safety study show a promising future for whole blood use in the civilian world.
References
- Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB. Warm Fresh Whole Blood Is Independently Associated With Improved Survival for Patients With Combat-Related Traumatic Injuries. The Journal of Trauma: Injury, Infection, and Critical Care 2009;66(Supplement):S69–S76.
- Cotton BA, Podbielski J, Camp E, et al. A Randomized Controlled Pilot Trial of Modified Whole Blood Versus Component Therapy in Severely Injured Patients Requiring Large Volume Transfusions. Annals of Surgery 2013;:1–7.
- Yazer MH, Jackson B, Sperry JL, Alarcon L, Triulzi DJ, Murdock AD. Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. Journal of Trauma and Acute Care Surgery 2016;81(1):21–6.
Authorship
- Intro - Jeffery Hill, MD MEd
- Spinella, et al - Brittany Bernardoni, MD PGY-3, University of Cincinnati Department of Emergency Medicine
- Cotton et al - Jimmy Summers, MD PGY-3, University of Cincinnati Department of Emergency Medicine
- Yazer et al - Jessica Baez, MD PGY-3, University of Cincinnati Department of Emergency Medicine
- Peer Review, Editing, and Posting - Jeffery Hill, MD MEd