AORTIC ULTRASOUND
INDICATIONS:
Evaluate for abdominal aortic aneurysm
Abnormal:
>3cm diameter for abdominal aorta
>1.5cm diameter for common iliac arteries
REQUIRED IMAGES:
Anatomy:
The abdominal aorta travels retroperitoneally just anterior and left of the spine. It enters the abdomen at the level of the xiphoid, tapering in diameter distally until it branches into the iliac arteries just inferior to the level of the umbilicus. On its path it gives off several branches at predictable levels:
Aneurysms will appear as areas of dilatation along the aorta itself. These are most commonly fusiform, as below, but can be saccular as well. Fusiform aneurysms are focal areas of circumferential widening, while saccular aneurysms are an outpouching of the aortic wall. A third type of aneurysm, a pseudoaneurysm, can occur in conjunction with aortic dissection. This can form an outpouching of the aorta as the damage to the vessel allows blood to collect between the two outer layers of the aortic wall
This is why it is important to image the aorta in two planes, as each of these can be easily missed if only viewed in one plane.
Our goal in aortic ultrasound is to visualize the entirity of the abdominal aorta, beginning at the level of the celiac artery, all the way to its bifurcation into the common iliac arteries. We will measure the diameter of the aorta at 3 different levels to assess for any areas of dilatation.
A diameter of the abdominal aorta >3cm or diameter of iliac artery >1.5cm indicates presence of an aneurysm.
An adequate exam should contain:
Transverse views of the proximal, mid, distal aorta, as well as the bifurcation into iliac arteries
Longitudinal view of aorta at proximal, mid, and distal levels
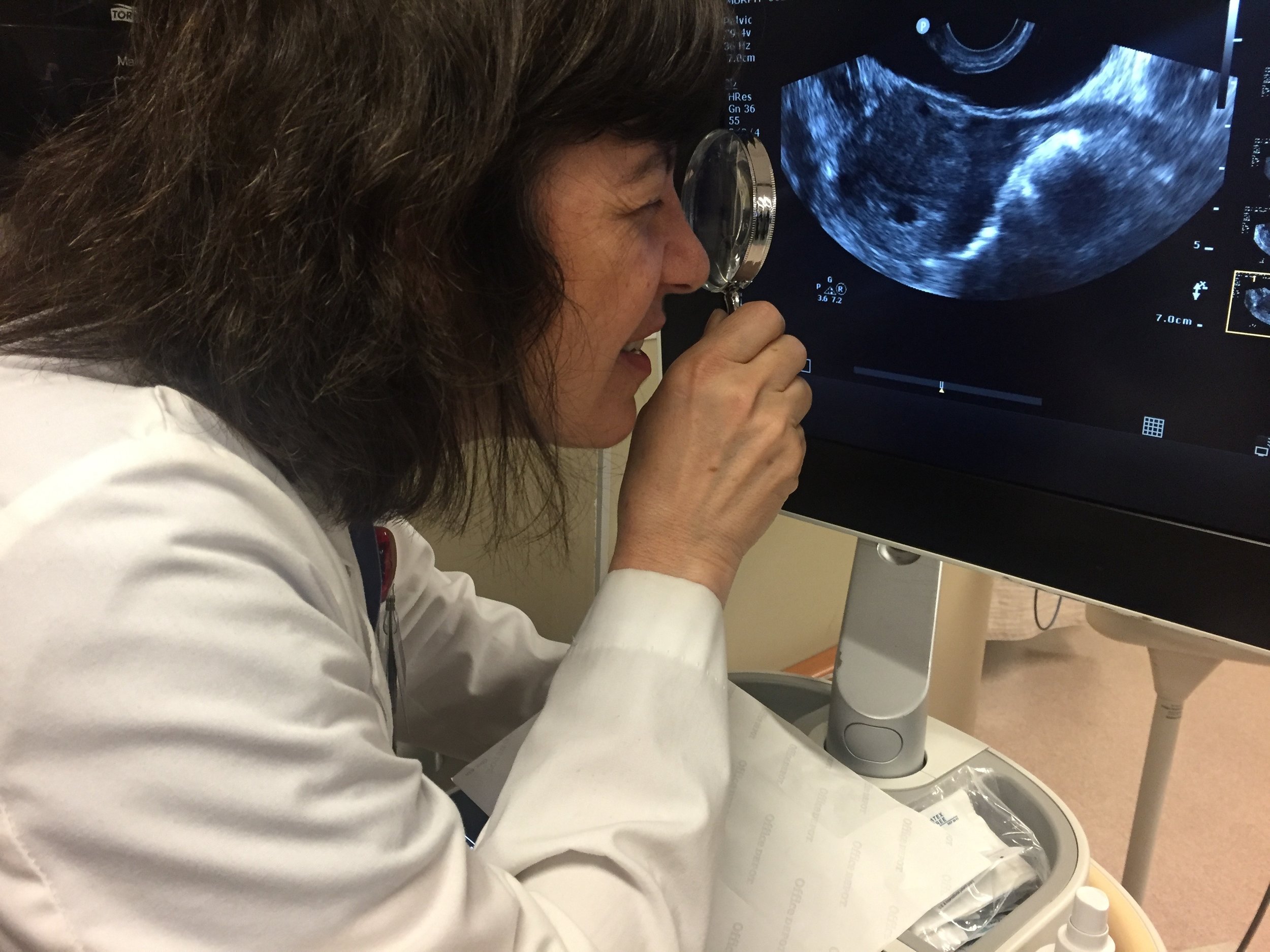
HOW TO SCAN AORTA:
Probe selection
The probe of choice is the curvilinear probe as it has lower frequency and can penetrate deeply. Alternatively, one can also use a phased array probe if available.
This exam is performed in 3 sections: Proximal, Mid, and Distal/Bifurcating Aorta
Proximal Aorta:
1. Orient the probe in the transverse plane, with the probe marker facing to the patient’s right. Place the probe just inferior to the xiphioid process
2. Adjust the depth such that you can identify the vertebral shadow in the far field of your image. This will appear as a densely hyperechoic, concave down shadow (frowny-face)
3. Identify the Aorta, which will appear as a hypoechoic, pulsatile, thick walled circular structure just anterior to the vertebral shadow. (The aorta will tend to run just slightly right of midline on the screen. The IVC will appear just to its left, and will have compressible walls)
4. Identify the celiac trunk, which will appear as an anterior branch off the aorta. The celiac will then branch into the hepatic and splenic arteries in the “seagull sign”. (You may not always be able to visualize this area, as it is often too proximal. It is useful for orienting yourself to the level of aorta you are imaging, but not necessary for a scan to be 'adequate'.)
5. Fan/Slide the probe inferiorly. Note the branching of the SMA which will appear as a small circular structure with hyperechoic walls, just anterior to the aorta. You may also see the left renal vein passing between aorta and SMA, as well as the splenic vein anterior to SMA'
6. Measure the aorta in its longest diameter at this level (outer wall to outer wall)
Transverse view of proximal aorta.
Note concave down shadow of vertebral body in far field, with pulsatile, thick walled aorta anterior. The IVC is visible just to the left of the aorta on the screen.
Transverse view of proximal aorta with doppler
Note that both IVC and aorta have pulsatile flow. One must rely on anatomical position and ultrasound appearance of the wall to differentiate the two.
Proximal aorta at the level of Celiac Trunk/Superior Mesenteric artery. Image transverses proximal to distal in the transverse plane.
The celiac trunk is visible proximally with initial branch coming from anterior aorta. It gives off the common hepatic and splenic arteries in the 'seagull sign'
The SMA originates just distal to the celiac trunk. It is visible in transverse view just anterior to the aorta. Note the left renal vein communicating with the IVC after it passes horizontally between the aorta and SMA.
Another, clearer example of the 'seagull sign' of the celiac trunk as it gives off common hepatic and splenic arteries
Mid Aorta
Longitudinal view at same level as above
Note Celiac trunk branching off the Aorta proximally
Just below the celiac origin, the SMA is clearly visible as it branches off the aorta and takes a path pointing inferiorly.
Continue sweeping the probe caudally in the transverse plane, keeping the aorta in view the entire time
Ideally, visualize the renal arteries as you slide down the aorta. (This is often difficult)
Obtain a measurement of the mid aorta in its longest dimension at the level of the renal arteries.
Image obtained while sweeping transversely down the aorta. Note lack of clearly visible branches. This lack of clearly identifying landmarks is typical for the midportion of the aorta.
If you look closely, a portion of the L renal artery is visible as it branches off of the aorta!
Note also that the aorta appears much closer to the probe as you approach the inferior aorta. You may need to adjust the depth accordingly!
Distal Aorta
Continue sweeping the probe caudally towards the umbilicus, keeping the aorta in view the entire time
Watch the aorta carefully for its bifurcation into the iliac branches.
Measure the diameter in the transverse plane both before and after its bifurcation into each of the common iliac arteries.
Note: (If you can visualize the renal arteries, care should be taken to obtain measurement infra-renally, as this is the most common location for aneurysms to occur)
Image obtained while sweeping probe inferiorly at the level of the distal aorta, through the bifurcation into the common iliac arteries.
Longitudinal
This can be performed along with each segment, or following completion of imaging in the transverse plane. It is usually easier to complete this separately, given the constant, even pressure often needed for adequate imaging of the aorta. Obtaining a transverse image and releasing pressure can allow bowel (and air!) to move and obscure a previously good imaging window.
As such, we recommend that once an adequate image is obtained in the transverse plane, the user sweeps the probe through the entire length of the aorta as directed above, before progressing to longitudinal views.
Return to the proximal aorta, turn probe 90 degrees in the longitudinal plane, such that probe indicator faces patient’s head
Repeat scan in the longitudinal plane, fanning through the aorta, making sure to capture the aorta in its midline (maximal diameter)
Longitudinal view extending from proximal to mid abdominal aorta
When imaging in the longitudinal plane, take special care to ensure that you are imaging the aorta and not the IVC
This image which fans from aorta to IVC as the probe is fanned from patients left to right. It shows that even a slight angle change of the probe can lead to false visualization of the IVC.
Always look for wall pulsatility, thick muscular wall of the aorta, and branching vessels to ensure that you are in the correct plane.
The IVC can also be distinguished as it runs intra-heptically for a segment (note liver present both anterior and posterior to IVC on adjacent image) and empties into the RA if tracked superiorly.
IMAGE INTERPRETATION
Abdominal Aortic Aneurysm (AAA)
Although aortic aneurysms can occur in any portion of the aorta, the most common location is in the abdominal portion. Luckily, this is also the portion that most amenable to evaluation via ultrasound. As such, the above exam is indicated to evaluate for exactly this pathology.
Abdominal aortic aneurysms can occur for various reasons. Risk factors include: male gender, age>50, HTN, smoking history, and history of connective tissue disorder such as marfans or Ehlers- Danlos. They also do tend to run in families for unclear reasons. Patients with AAA often asymptomatic and pain free initially, however can have pain, neurologic or vascular compromise as the aneurysm enlarges. Rupture becomes more likely as size increases and is rapidly fatal when present.
Abdominal aortic aneurysm is defined as:
>3cm diameter for abdominal aorta
>1.5cm diameter for common iliac arteries
Examples of AAA visible in transverse section. Note rim-like mural thrombi which surround the aortic lumen. This exemplifies the importance of the need to measure outside wall to outside wall when measuring aortic diameter.
AAA in the mid abdominal aorta viewed in longitudinal section. Also visible is mixed echogenicity mural thrombus which is most prominent anteriorly (superior aspect of image)
Ruptured AAA in the mid abdominal (infrarenal) aorta. Note large mixed echogenicity fluid collection on the right side of the image which communicates with AAA
Similar ruptured AAA as viewed on axial imaging by CT scan.
Open arrow represents AAA, Closed arrow represents intra abdominal blood collection
While ultrasound alone cannot determine whether a AAA is ruptured, a positive finding on aortic ultrasound should be taken in clinical context. In a patient with unstable vitals and appropriate history, they should be presumed as ruptured until proven otherwise. Assessment for peritoneal fluid may be negative as these patients often hemorrhage in the retroperitoneal space.
AORTIC DISSECTION
Aortic dissection occurs when blood enters the space between the intima and media layers of the arterial wall. This causes the creation of a flap of tissue within the vessel. As the blood enters the media of the vessel at high pressure, it further dissects through this tissue plane, often creating a false lumen.
[A- Aorta, M-Media, I-Intima, FL-False lumen, TL-True Lumen]
Ultrasound is not indicated as a primary modality for the evaluation of aortic dissection given inadequate sensitivity (about 67-80%). However, there is high specificity (99-100%). As such, it is worthwhile to note the appearance of dissection when seen on ultrasound. An ultrasound which does not show a dissection does NOT rule out this disease process, however. Similarly, this exam only focuses on evaluation of the abdominal aorta, and thus we cannot make any determinations about the thoracic aorta.
The Sanford classification separates aortic dissection into two types based on location.
Type A dissection originates from the most proximal aspect of the aorta (proximal to left subclavian artery). It can, however, extend as far as the descending and abdominal aorta.
Type B dissection originates anywhere distal to the left subclavian artery.
The presence of dissection on ultrasound can appear as a free flap visible within the lumen of the aorta. Depending on the plane in which the flap occurs it may be visible on transverse, longitudinal or both views.
Aortic Dissection present in proximal aspect of abdominal aorta. Image alternates from transverse view to longitudinal view. Note hyperechoic line representing dissection flap in most proximal aspect of the aortic lumen.
Aortic dissection noted again in longitudinal view in proximal aorta. Hyperechoic line in aortic lumen can be seen pulsating with heartbeat.
ANY patient with a finding of dissection flap on aortic evaluation should undergo rapid cardiac ultrasonography to rule out proximal dissection with cardiac tamponade.
PATTIES PEARLS
-Too much bowel gas? Try applying more pressure or rolling patient into left lateral decubitus
-You can an attempt to place probe in right anterior axillary line and use the liver as a window (similar to FAST view) but this will only assist in imaging the proximal aorta
- Aneurysms >5cm requires emergent work-up, aneurysms 3-5cm in the right clinical context can likely be referred for outpatient workup.
- Aneurysms most commonly occur infra-renal
- Watch out for intraluminal thrombus which can appear hyperechoic. That's why we measure outer wall to outer wall!
-Don’t mistake the IVC for aorta, especially in the longitudinal plane. Note that the IVC often has pulsatile flow and doppler may not be helpful.
Written by: Aalap Shah, MD
Peer reviewed by: Lori Stolz, MD, RDMS
All images obtained by Aalap Shah, MD and Pattie Smith, RDMS unless otherwise noted
References
Dawson, M., and M. Mallin. Introduction to Bedside Ultrasound: Volume 1. Lexington, KY: Emergency Ultrasound Solutions, 2013. ebook
Kent KC (27 November 2014). "Clinical practice. Abdominal aortic aneurysms.". The New England Journal of Medicine. 371 (22): 2101–8.
LeFevre ML (19 August 2014). "Screening for abdominal aortic aneurysm: U.S. Preventive Services Task Force recommendation statement.". Annals of Internal Medicine. 161 (4): 281–90.
Marie Kuhn, Robert L.L. Bonnin, Michael J. Davey, Jane L. Rowland, Suzanne Le P. Langlois, Emergency Department Ultrasound Scanning for Abdominal Aortic Aneurysm: Accessible, Accurate, and Advantageous, Annals of Emergency Medicine, Volume 36, Issue 3, 2000, Pages 219-223, ISSN 0196-0644,
Noble, Vicki E., and Bret Nelson. Manual of Emergency and Critical Care Ultrasound. Cambridge: Cambridge UP, 2011. Print.
P. Jaakkola, M. Hippeläinen, P. Farin, H. Rytkönen, S. Kainulainen, K. Partanen, Interobserver variability in measuring the dimensions of the abdominal aorta: Comparison of ultrasound and computed tomography, European Journal of Vascular and Endovascular Surgery, Volume 12, Issue 2, 1996, Pages 230-237, ISSN 1078-5884
RAP Scott, The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial, The Lancet, Volume 360, Issue 9345, 2002, Pages 1531-1539, ISSN 0140-6736, http://dx.doi.org/10.1016/S0140-6736(02)11522-4.
(http://www.sciencedirect.com/science/article/pii/S0140673602115224)
Smith, Pattie. Bedside Ultrasound Guide for Emergency Medicine. Cincinnati, OH. Print
Tayal, V. S., Graf, C. D. and Gibbs, M. A. (2003), Prospective Study of Accuracy and Outcome of Emergency Ultrasound for Abdominal Aortic Aneurysm over Two Years. Academic Emergency Medicine, 10: 867–871. doi:10.1197/aemj.10.8.867
Williams J, Heiner JD, Perreault MD, Mcarthur TJ. Aortic dissection diagnosed by ultrasound. West J Emerg Med. 2010;11(1):98-9.
![By Edoarado [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1502907828557-GNLUAR377UWNSPID1TRR/image-asset.png)
![By BruceBlaus (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1502912821121-UHNRKCK5C22GTEBOPSRC/image-asset.png)
![By Bakerstmd (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1502913054080-4CW26FD5ONTJERGSU970/image-asset.jpeg)


![Derivative of work by By BruceBlaus (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1502912088238-8HZZ6ZNYL8CEJM0ISD4W/Proximal+aorta.png)

![Derivative of work by By BruceBlaus (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1508187159014-KLJ0K60U40B1869JPDTT/Mid+aorta.png)
![Derivative of work by By BruceBlaus (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1502912201214-THVQY5HLGKFBQRVMVGCT/Distal+aorta.png)
![By James Heilman, MD (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1504286055919-WCGM26D749LHCPNQURUW/RupturedAAA.png)

![By Npatchett (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1504283645662-U5IITGEOH3V2RZEUKQP3/Aortic_dissection_types.jpg)