Lessons in Transport - TXA has Arrived!!
/We bring the world class care of UCMC to the patient through advanced transport medicine..."
-ACMC mission statement
To successfully resuscitate the critically ill trauma patient we must have an understanding of and a respect for the LETHAL TRIAD of TRAUMA...
Bleeding causes acidosis, coagulopathy, and hypothermia...
Acidosis and hypothermia causes more coagulopathy which causes more bleeding... and so begins a deadly cycle
Administration of anti-fibrinolytic agents such as tranexamic acid (TXA) has been shown to reduce blood loss in patients with both normal and exaggerated fibrinolytic responses to surgery. TXA has been used since 1966 to decrease bleeding from a variety of pathologies. Since 2010, two large clinical trials (CRASH-2 and MATTERs) have examined the specific role for TXA in adult trauma patients with evidence of or concern for severe hemorrhage. These studies found significantly favorable reductions in all-cause mortality when victims of trauma received TXA.
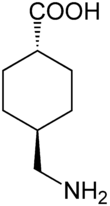
What is TXA?
An anti-fibrinolytic synthetic lysine analogue that inhibits both plasminogen activation and plasmin activity thus preventing clot breakdown and reducing hemorrhage.Other potential beneficial mechanisms of action including decreasing the systemic inflammatory response to trauma are currently being explored.
Who should receive TXA by Air Care & Mobile Care?
Patients who meet ALLof the following criteria should receive TXA:
Evidence of significant blunt or penetrating trauma based on the history of present illness and or physical exam findings. (ex: ejection from automobile, rollover MVC, fall > 20 feet, pedestrian struck, penetrating injury to head, neck, torso, etc.)
Age ≥ 16 years with evidence of severe internal or external hemorrhage. (ex: +FAST, bleeding requiring a tourniquet, unstable pelvic fracture etc.)
Presence of 1 or moremarkers of hemodynamic instability (criteria a-d) orUCMC Massive Transfusion Protocol laboratory Triggers (criteria e-h)
a.) Systolic BP < 90mmHgb.) HR > 100c.) Tachypnea > 24d.) Findings of peripheral vasoconstriction: Cool pale skin, capillary refill > 2 secondse.) INR > 1.5f.) Base deficits < -6mmol/Lg.) Hemoglobin < 11g/dLh.) Platelets < 200,000
Time since the initial injury is KNOWN to be less than 3 hours
Who should NOT recieve TXA by Air Care & Mobile Care?
Patients < 16 years old
Time elapsed from injury is unknown or greater than 3 hours
Evidence of active intravascular thrombotic disease or DIC
Patients who have received or will receive PCCs, factor VIIa or IX complex
Women who are known or suspected to be pregant with fetus of viable gestational age (> 24 weeks)
Previous hypersensitivity reaction to TXA
How do we administer TXA on Air Care & Mobile Care?
Initial bolus of 1 gram of TXA in 100ml of 0.9% normal saline or LR over 10 minutes IV or IO. (If given as an IV push, hypotension may occur)
***Use dedicated IV/IO line if possible and DO NOT administer in the same IV line as blood products, rFVIIa, or Penicillin***
What are the most important key points to remember?
Unstable Trauma Patient + age > 16 + injury less than 3 hours ago = 1 gram of TXA over 10 minutes
If a patient is recieving or will receive pRBCs during transport for treatment of a traumatic injury, they likely qualify for administration of TXA as well
Use dedicated IV/IO for administration of TXA