Grand Rounds Recap 12/16/15
/"IN JEOPARDY", AN ACS REVIEW - DR. FERMANN
Dr. Greg Fermann, Executive Vice Chairman, led us in a thought-provoking game of Jeopardy based on ED interventions and evidence based management of acute coronary syndrome. A few of the learning points (and links to the literature) are here.
EKG Changes
- According to the AHA, there are no diagnostic EKG changes for NSTEMI
- ST elevations in II, III and aVF with depression in V2 represents and inferior-posterior STEMI
- ST depressions in the precordial leads may represent posterior MI
- Continuous ST segment trend monitoring may pick up very dynamic ischemic changes (though this is almost never done anymore)
ACS Risk
- The comorbidities associated with atypical ACS presentations are female sex, advanced age, heart failure and prior CABG/PCI
- The simplest validated quantitative risk model in NSTEMI is the TIMI Risk Score
- Level of troponin elevation is the greatest predictor of 6 month mortality in NSTEMI
Medications
- There are three main delivery routes for nitroglycerin: sublingual, transcutaneous and IV
- Two reasons not to give nitroglycerin are hypo-tension and phosphodiesterase use. Inferior MI is a reason to use caution but can be done safely if patient closely monitored and can easily give IV fluids to prevent hypotension
- The three proposed beneficial effects of morphine in managing ACS symptoms are analgesia, anxiolysis and pulmonary ventilation. However, there is an increased mortality risk with morphine use in NSTEMI (http://www.ncbi.nlm.nih.gov/pubmed/15976786)
- The preferred route of beta-blocker administration in ACS is oral. The COMMIT trial showed metoprolol should be given after the patient is stabilized to decrease risk of worsening cardiogenic shock
- The preferred anticoagulant for STEMI patients who are going to undergo thrombolysis is enoxaparin (ExTRACT-TIMI25) though the study did show an increase in nonfatal ICH
- The most common anticoagulant used in the ED in the United Stated for managing ACS is unfractionated heparin
- There is no oral anticoagulant approved by the FDA for managing ACS
- The ACCOAST trial showed upstream (use in the ED as opposed to at the time of PCI) use of prasugrel should be avoided in NSTE-ACS
- The most common site of bleeding in ACS patients who underwent catheterization with anti-platelets on board is the groin (seen less commonly with the radial artery site)
- Major bleeding is such a problem in ACS care because of hypotension, need for transfusion and discontinuation of beneficial antithrombotic therapy
- The factor that drove the magnitude of the bleeding risk with clopidogrel in the CURE trial was the dose of ASA
- The best therapy for patients with acute major bleeding while taking anti-platelets is administration of platelets
- The current accepted pathophysiology for ACS is platelet aggregation and thrombus formation
- The mechanism of action of clopidogrel, prasugrel and ticagrelor is to prevent platelet activation through the ADP receptor
- The mechanism of action of abciximab, eptifibitide and tirofiban is to prevent platelet aggregation
- The most recent ACC/AHA Guidelines specifically recommend the use of ticagrelor as an anti-platelet in upstream (in the ED) care
THE CRASHING PATIENT WITH CONGENITAL HEART DISEASE - DR. RICHARDSON
Congenital heart disease is common, and with advances in pediatric surgical care, many patients are surviving to adulthood and transitioning out of dedicated pediatric centers to receive care in general Emergency Department settings.
The range of possible conditions is broad, but most patients with congenital heart disease have essentially normal physiology. They are still at early risk for heart failure, pulmonary hypertension, dysrhythmias (especially atrial tachycardias and sinus node dysfunction), and valvular stenosis or insufficiency – but, you can manage these problems much like you would a patient without CHD history, at least until specialist backup is available.
However, there are two conditions that produce very different physiologies, especially in a true emergency or resuscitation situation:
- Mixing physiology: this occurs when there is a large shunt that allows either L to R or R to L flow.
- The prototypical lesion is a large ventricular septal defect, but it can also occur in younger patients who have had palliative procedures (like a Blalock-Taussig shunt or Norwood).
- In these circulations, part of the cardiac output of one or both ventricles can be directed to either the pulmonary circulation or systemic circulation, and any change to pulmonary or systemic vascular resistance can affect the direction and volume of the shunt
- Hypoxia can be a normal finding. Find out what the patient’s normal oxygen saturation is and keep them there.
- Interventions (like supplementary oxygen) that decrease PVR may cause pulmonary over-circulation, decreasing systemic cardiac output
- Factors that raise PVR or lower SVR may worsen a R to L shunt and cause worsening hypoxia.
- Fontan physiology: this occurs in patients with functionally uni-ventricular hearts (hypoplastic left or right heart syndrome; tricuspid or pulmonary atresia) who have had surgical palliation.
- e Fontan operation is done in stages over the first 1-2 years of life
- A complete Fontan involves connecting the SVC and IVC to the pulmonary artery and disconnecting this from the heart, meaning pulmonary blood flow is entirely passive.
- These patients are very sensitive to changes in venous return. Dehydration or interventions that impair venous return (high PEEP, sedative drugs like propofol) dramatically lower pulmonary blood flow and ultimately cardiac output.
- A dry Fontan is a dead Fontan!
R2 CASE FOLLOW-UP - DR. TITONE
18 y/o previously healthy female with 2 week history of sore throat, left sided neck pain, fevers and rigors presents with shortness of breath and pleuritic chest pain. CXR shows multifocal pneumonia and CT of the neck with IV contrast shows thrombus of left IJ with extension of clot in facial vein.
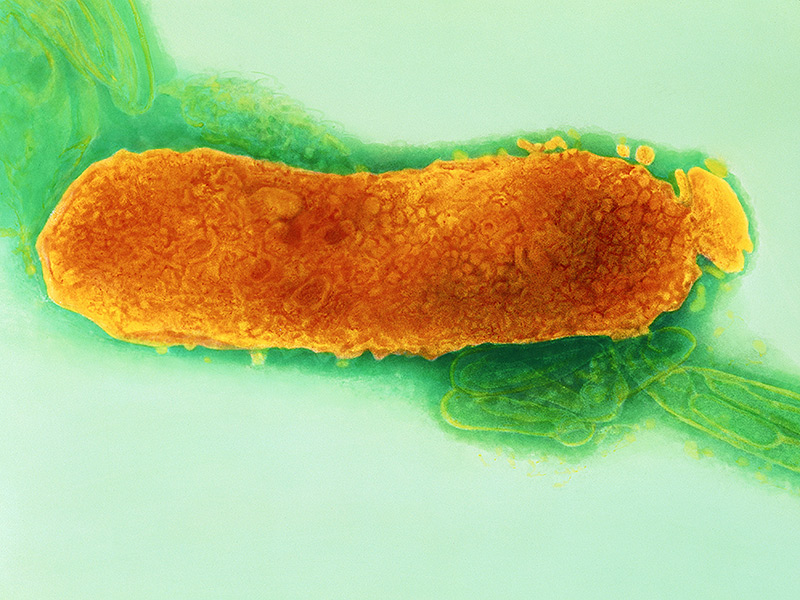
Diagnosis: Lemierre's Syndrome
- Lemierre's Syndrome: Thrombophlebitis of the internal jugular vein caused by direct spread of bacteria from tonsilar veins. Can also be secondary to dental infection or central line placement.
- Most often caused by the gram negative anaerobeFusobacterium necrophorum.
- The most common presentation is a healthy 18-22 year old with 1 week of sore throat and neck pain who develop septic emboli. to the lungs (97%), heart or joints.
- Gold standard diagnostic test is CT Neck with IV contrast. Jugular vein ultrasound is sensitive but not specific.
- Initial treatment is with beta-lactamase resistant beta-lactams with addition of vancomycin if infection is catheter related.
- Anticoagulation is controversial and should not be started in the ED.
- We can avoid this complication is we consider bacterial pharyngitis and antibiotics in patients with >3 days of sore throat, high fevers, rigors and lack of coryzal symptoms
R1 CLINICAL KNOWLEDGE: SPONTANEOUS BACTERIAL PERITONITIS - DR. MERRIAM
Your patient has a protuberant belly, spider angiomas, and palmar erythema. He has a fever and is complaining of abdominal pain. Spontaneous bacterial peritonitis has many presentations, from blaringly obvious to completely subtle, and it is up to us to make the diagnosis. Here are some important points to remember:
SBP: ascitic fluid neutrophil count ≥250 or positive culture
Risk Factors: previous SBP, history of variceal bleed, TBili >1.5, malnutrition, PPI us
Indications for Paracentesis in the ED: patient with ascites who has abdominal pain, fevers, altered mental status, or leukocytosis; any patient with ascites who is being admitted
Mortality increases with each hour of delay to paracentesis
Treatment of SBP: 3rd generation cephalosporin
R4 CAPSTONE - DR. LOFTUS
Dr. Loftus regailed us with advice gleaned over his four years here. He summed it up with the following poetic tribute:
“With the air still fresh with the educational stylings of Dr. Merriam covering SBP,
Dr. Loftus stepped to the front, quickly making allusions to the illustrious “Steu-ie.”
Entitled “How We Think, What to Read, and the Act of Doing,” his talk received curious looks,
yet the attentive audience quickly learned it was really all about Books.
Covering Seuss, Gawande, Carnegie, Kahneman, and Gaffigan,
he helped those present learn how to laugh again.
Discussion was held on personal lessons learned as an R1, 2, 3, and 4.
The sincerity, sappiness, and sentimentality left all yearning for more.
From Seuss’ Horton to Juster’s Milo, Loftus alluded to lessons learned the hard way,
Like “There’s no such thing as trolls,” “Don’t be an a-hole,” and “Everyone has a bad day.”
Ultimately, Tim’s message was clear - Be Your Own Critic, Relax, Do Right, and Have Fun.
By doing so, in his view anyway, your journey through this Residency will be won.”
NEONATAL RESUSCITATION - DR. BRADY
Neonatal Resuscitation (NRP) is the standard of the unwell newborn
Next ED shift your colleague calls your into the bay and there is an emergent delivery taking place, time to split tasks - don't worry - he will take the mom.
Let's talk about the management of the full term infant emergent delivery in the ED....
- Initial triage
- Is it a term gestation? How many fetuses?
- Is the baby breathing or crying?'
- Does the baby have good tone?
First things first - warm, dry, stimulate - try for 30 seconds for response
- Primary apnea - will reverse and start breathing with stimulation
- Secondary apnea - a host of other etiologies
Reassess the babies breathing and now assess the HR as > < 100
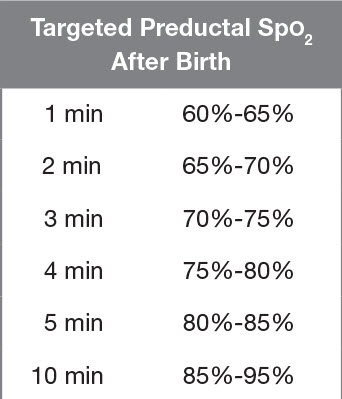
- Attach pulse oximetry (right wrist or hand to get preductal saturation)
- Start PPV (PIP 20 / PEEP 5, RR 40-60) and ensure adequate chest rise with normal chin lift techniques and ensuring a good seal
- FiO2 should titrate to goal pulse ox for age - start with 21% FiO2 for full term, 30% in premie
Reassess - if you have persistent bradycardia - now add on traditional CPR to your airway management, preferably after definitive airway management
- Size 3.5 - 4 ETT for most full term neonate
- Size 0-1 Phillips is the easier blade of choice for almost all neonates
Post-intubation the HR is still low (<60)?
Start compressions at 90 per minute
- In sync with PPV breaths every third compression 30/minute saying one-and -two-and three-and-breaths
- Either 2 finger anterior pressure or thumb method are good methods
Reassess - if the HR is in between (80-100), improve your airway adjuncts and ventilation
At this point we start considering epinephrine if airway techniques are optimized and compressions are ongoing
- 1 ml/kg of 1:10,000 (code dose) epi
- Can be given every 3-5 minutes
- Can be given through ETT while obtaining access
- IV is preferred and worth trying
- UVC (Umbilical Venous Catheter) is the preferred access
- 2 arteries and 1 vein which should be the most open (photo)
- Tie the umbilical cord being starting and cut above that, as close to the neonate as possible
- Prime your line with saline and inset ~3cm for a premie and ~5cm for a full term
- Ideally a sterile procedure (central line)
Continue to reassess every 60 seconds until the cavalry arrives
Caveats
Babies < 1500g
- Do not dry due to increased insensible loses and prone to hypothermia
- Start immediately with PPV
Meconium Recommendations
- No longer recommended to intubate and suction early, the guidelines simplify and by using the above guidelines
VISUAL DIAGNOSIS SMALL GROUPS - DRS. MCKEAN, GROSSO AND BETHAM
More than 95% of African American & 80% of Asian infants are born with Mongolian spots. Often mistaken for signs of NAT, these macular lesions should be uniform in color and do not change over the course of days.
In TCA overdoses, QRS >100ms is predictive of seizures, QRS >160ms is predictive of ventricular arrhythmias.
The diagnosis of PCP pneumonia should trigger an order for a room air ABG. If the patient's A-a gradient is greater than 45mmHg (or PaO2<70mmHg) they should get IV antibiotics plus corticosteroids to decrease incidence of mortality and respiratory failure that accompanies the antibiotic induced-organism death approx 2 days after treatment is initiated.
Perineal desquamation within the first week of a febrile illness in infants & children is an early diagnostic clue for Kawasaki's disease.
TEG with both a low MA & high Lys30 after trauma should prompt treatment with TXA to prevent clot breakdown.