Grand Rounds Recap 11.16.16
/M&M with Dr. Grosso
Case #1
The patient is a middle aged male with history of septic arthritis (left knee 2 years ago) who came to ED with ankle pain. Complaining of right ankle pain refractory to ibuprofen. Temperature of 99.9, heart rate of 96, other vitals unremarkable. Normal CBC, ESR normal, CRP elevated to 80. Ankle X-ray with some soft tissue swelling, consistent with images 1 week ago. Synovial fluid analysis shows total nucleated cell count of 803 and calcium pyrophosphate crystals, negative gram stain. Treated for pseudo gout and sent for follow up with orthopedics. Blood cultures return positive, patient called to return to ED, no change in vitals or physical exam on repeat assessment. While patient is in ED, second culture returns positive for same (gram positive cocci and clusters), found to be MSSA and repeat arthrocentesis of ankle by orthopedics returning with significant elevation in WBC count, culture positive for MSSA.
Blood culture contaminants:
- False positive: organisms that are not actually presenting a blood sample are grown in culture
- Target contamination rates nationally are set at ~2-3%
- Clues to help differentiate contamination from bacteremia
- Identify the organism
- Staph aureus, strep pneumo, e. coli, etc consider true positive until proven otherwise
- Coag negative staph often considered false positive
- Paper looking at likelihood of true positive result correlating with first call from the lab
- values range from only 13% positive for coag negative staph, to near 100% for yeast and gram negative rods
- Number of positive culture sets
- Near linear relationship with positivity
- Number of positive bottles within a set
- Time to growth
- More likely contaminant if it takes >3 days to grow
- Quantity of growth
- Clinical and laboratory data correlates as well (vitals, labs, etc)
- Rigors in particular has high PPV
- Identify the organism
- Who should get blood cultures?
- Prospective study to evaluate for possible decision rule
- Major criteria:
- concern for endocarditis
- Temperature >103F
- Indwelling catheter
- Minor criteria:
- Lower fever, chills, and other laboratory/clinical markers classic for infection
- Patient found to be low risk (NPV 99.4%) if 0 major criteria or <2 minor criteria
- Major criteria:
- Prospective study to evaluate for possible decision rule
Case #2
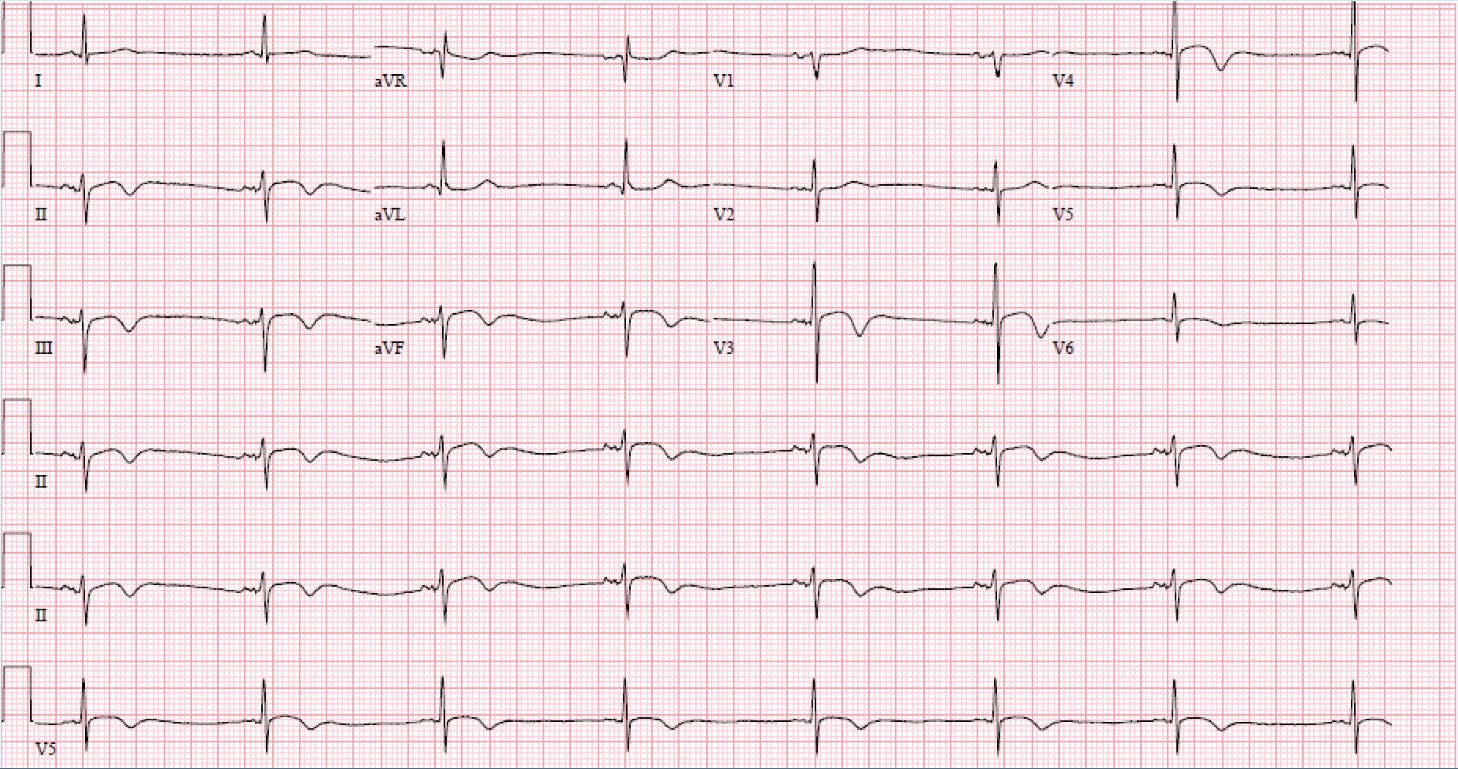
Younger male with history of bipolar disorder with presentation for concern of “possible PE”. Complaining of right sided chest pains and shortness of breath, presenting from psychiatric facility, near catatonia. Tachycardia to 116, EKG shows sinus tachycardia. CXR shows no acute cardiopulmonary process. Labs are notable for negative troponin, positive D-dimer (0.86). CTPA negative for PE. Tachycardia refractory to 2 L crystalloid. Bedside ultrasound negative for pericardial effusion. Discharged back to facility. Returns 4 days later, troponin values had been followed and had now elevated to 0.3. Patient noted to have fevers over the past several days, had been receiving antibiotics and IVF. Looks clinically more sick on second presentation. EKG shows sinus tachycardia, unchanged from previous. Labs unchanged with the exception of troponin to 0.5. TTE performed which shows EF 45-50%, no regional wall motion abnormality. Repeat EKG shows possible PR depression, considering possible myo-pericarditis. Admitted to cardiology, troponin peaked at 6. Theory of myocarditis secondary to clozapine use. Medication was stopped and patient improved over the next 48 hours.
Inflammatory disease of the myocardium:
- precursor of dilated cardiomyopathy (most common cause of heart transplants worldwide)
- 21% go on to develop dilated cardiomyopathy
- 12% of sudden death in young adults
- Common causes
- Viral infection (Parvovirus B19, HHV 6)
- >50% of patients with HIV had myocarditis on autopsy
- Bacterial infections
- Medication
- antipsychotics (clozapine)
- antibiotics (penicillins)
- Autoimmune disease
- Viral infection (Parvovirus B19, HHV 6)
- Clinical presentation
- chest pain
- arrhythmias
- Heart failure (fulminant or indolent)
- Diagnostics
- Labs
- Troponin (helpful for prognostics)
- CRP and WBC are less helpful
- Viral testing (not helpful, often cleared by time of clinical presentation)
- EKG
- Used as screening tool, low sensitivity
- Echo
- Cardiac MRI
- Biopsy: gold standard (being replaced by MRI)
- Labs
Case #3
Elderly male with history of CAD, thoracic aortic aneurysm, active leukemia on chemotherapy, arrives with altered mental status. Patient began to complain of achy back pain, abdominal pain, right leg numbness. Unresponsive upon EMS arrival, went into cardiac arrest, ROSC achieved in field. Heart rate 111, BP 201/108, diaphoretic, pale, diffuse left sided flank mottling. Moves all four extremities, not responding to commands. FAST adequate and negative. Patient intubated, lactate 8.9, pH 7.04, WBC 169.7 (that’s not a typo). CT shows dilation of thoracic aorta with findings showing dissection and some rupture, distal to arch of aorta. Blood pressure drops in scanner while blood transfusing, goes to OR with vascular surgery from scanner. Patient expired intra-operatively.
Thoracic aortic aneurysm (TAA)
- 10/100,000 people in US develop TAA each year
- Rupture 3.5/100,000 annually
- Dissection 3.5/100,000 annually
- only 41% of ruptured TAA make it to the hospital
- of those that do arrive to hospital, 28% expire
- For our hospital:
- Stanford Classification Type A dissection is a call for cardiac surgery
- Type B involves vascular surgery
- Acute type B aortic dissection
- 10.6% mortality
- Surgical and endovascular repair is reserved for patients in shock or with signs of limb ischemia.
- Demographics
- Only statistically significant for prognosis is that of age >70
- Symptoms
- chest pain, back pain, sudden onset of pain most sensitive
- syncope, hypertension, and hypotension are most predictive of severe disease
- Prediction of in-hospital mortality
- female gender
- age >70
- syncope
- hypotension
- shock
- periaortic hematoma
- ischemia of any distal organ site (mesenteric ischemia, renal failure, etc)
Case #4
Elderly female with history of afib, hyperlipidemia, CHF, CAD, ESRD on dialysis, presenting with altered mental status. Appears acutely ill, tachycardia, hypotension, chronic open wound on posterior right calf. Fingerstick blood sugar of 26. EKG shows atrial fibrillation, low voltage and T wave inversions unchanged from previous EKG. CXR shows unchanged cardiomegaly from previous image. Patient blood pressure drops to 51/17. Patient received phenylephrine IV push, 500 ml crystalloid, 5 mg IV diltiazem. Temperature recorded at 91.4F. Vancomycin and cefepime were ordered. New thrombocytopenia noted and her lactate continues to increase. Despite agressive fluids, pressors and anti-dysrhythmics in the MICU, the patient expires.
Sepsis in ESRD
- Annual % mortality secondary to sepsis is 100-300x higher in ESRD
- In a study of 90 ESRD patients on HD in sepsis
- 39 were bacteremic
- 26% died during that hospital visit (those in septic shock had mortality of 40%)
- 30 day mortality of those that survived was 25%
- on average these patients only received 600 ml of IVF in the first 6 hours of stay
- very under-resuscitated due to concerns of fluid overload
- Do present with SIRS criteria and elevations in lactate
- Temperature less sensitive than in baseline population
- Pathophysiology of sepsis is the same, massive vasodilation does require aggressive fluid resuscitation
- Dialysis can be performed for any excess fluid, intubation for pulmonary edema, etc
- the mortality is too high for sepsis in this population to be slow with your fluids
Atrial fibrillation in Critical illness
- Retrospective study of patients being evaluated for different primary illness but with concomitant atrial fibrillation
- Majority of patients were in either heart failure or sepsis
- Odds of an adverse event was 8.3x higher in patients receiving rate or rhythm control than those who didn’t (just addressed primary pathology)
- The sooner the rate control was attempted the more likely the patient was to have an adverse event
Case #5
Young female with history of lupus, VTE, pacemaker/ICD for previous V tach, presenting for chest pain radiating to jaw, left arm, as well as abdominal pain, nausea, and vomiting. Hemodynamically stable. Labs notable for lipase of 900, troponin and other labs are unremarkable. EKG notable for intermittently paced rhythm, no ST changes, no acute changes from previous EKG. Repeat EKG unchanged in ED. CT scan of abdomen/pelvis performed and shows acute pancreatitis, shows small splenic infarcts which are new. Patient admitted to hospital. Once admitted while in ED patient complains of 10/10 chest pain, PCA ordered by admitting team. TTE performed shows new EF of 35-40% as well as regional hypokinesis. Pain worsening and tachycardia, PCA increased, troponin second value the next day returns at 16. EKG repeated, shows ST segment elevation in lateral precordial and inferior leads. LHC shows 100% occlusion in LAD with no associated plaque. Thrombectomy performed.
SLE and CAD
- women with lupus 35-44 years old were 50x more likely to have an MI compared to women of similar age without SLE.
- the longer patient is on steroid therapy the more likely the patient is to have an MI
ED to Inpatient Hand offs
- Survey of ED and IM providers about ED to inpatient transfers
- 29% reported an adverse event or near miss
- Particular vulnerabilities in handoff
- Flows in communication (highlight your concerns)
- Environment
- Patient Flow (be wary of “the admitted patient” still in the ED)
- Information Technology
- Assignment of Responsibility
- Task assignments should be explicit
- Call medicine senior when an admitted patient in ED is being escalated in care
- Anchoring bias
- people make estimates by starting from an initial value that is adjusted to yield the final answer
- If you don’t know what the diagnosis is, don’t say that you know
- Treat your anchor more like a buoy, we can easily set an inpatient team down a path even if the patient is still undifferentiated if we aren’t careful
R3 Small Groups - Procedural skills with Drs Teuber, plash and Gorder
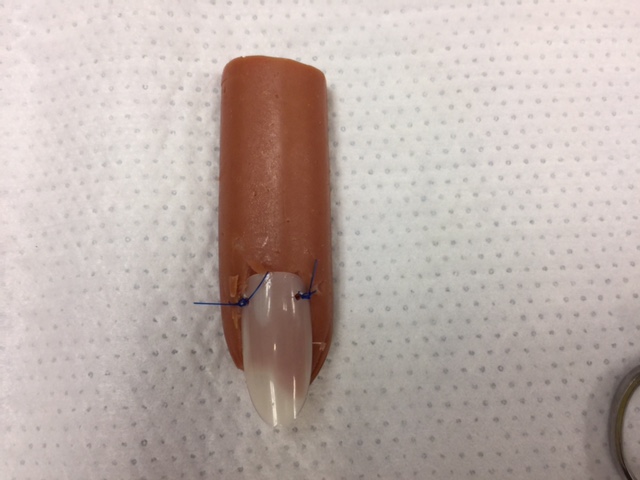
Nail Bed Lacerations
- For nail bed lacs, digital block the finger, and then bluntly dissect the nail off the nail bed.
- For actual lac repair, you can consider 6-0 absorbable sutures vs derma bonding the nail lac, which may save some time.
- To replace the nail, consider puncturing each side near the eponychium with an 18G needle to place a suture through the holes and anchoring the nail into the nail bed.
- If no underlying fracture associated, there is no good evidence to recommend for or against antibiotics.
Auricular Hematoma
- Analgesia can be best obtained via auricular block, consider 1% Lido with epi
- If hematoma is <2cm in diameter, and present <48hrs:
- perform a needle aspiration over the most fluctuant part of the hematoma
- These ears do well with pressure dressings
- If hematoma >2cm in diameter or present 48 hrs - 7 days:
- I&D is recommended with incision along the curvature of auricle
- These ears need mattress sutures or a bolster
- Mattress sutures should be through and through the ear, and may be absorbable or non-absorbable sutures
- Bolsters should be done with non-absorbable sutures
- Bolsters and non-absorbable sutures should be removed at 7 days
- If anti coagulated, consult ENT/Plastics
- All patients need close ENT/Plastics follow up
- Antibiotic prophylaxis with pseudomonas coverage 7-10 days is recommended. Amox/clav is a good first line.
Paronychia/Subungual Hematoma
Subungual Hematoma: Defined as a collection of blood between the nail and nailbed (often from blunt trauma).
- If not painful - no intervention needed!
- If painful, treatment involves trephination over the hematoma
- Apply antiseptic solution over the nail to reduce risk of introducting bacteria into nailbed
- You then have two options (neither requires analgesia):
- Electrocautery with single puncture through the nail
- Blunt trephination with 18g blunt fill using rotational motion
- Take care not to puncture through the nail bed
- No need to remove the nail to inspect the nailbed for simple hematoma
- These generally do not require antibiotics
- Apply a dry dressing over finger after trephination
- No soaking/submission of finger for 2-3 days
Paronychia: an abscess of the nail fold
- Usually from trauma (pulling a hang nail)
- Treatment involves drainage (like any abscess)
- Digital block is most effective for analgesia
- Incision can be made along the cuticle or parallel to nail bed along the fold
- For small infections, you can use a needle to lift skin from cuticle, sometimes without anesthesia
- No evidence for antibx in absence of surrounding cellulitis
- If surrounding cellulitis, consider staph and strep coverage. If extends to hand, consider monitoring with IV antibiotics.
Global Health Grand Rounds with Drs Roche, Teuber and Lagasse
Options for Non Vascular Hydration in Resource-Poor Situations
Dehydration is a leading cause of death in resource poor areas, and is often due to diarrhea.
- ORS (oral rehydration solution) is comprised of salt and sugar. 25-50cc/kg administered over 6-12 hour period.
Recipes for ORS include:
- 1L clean water; 1 teaspoon salt; 8 teaspoons sugar
- 1L clean water; 1/2 teaspoon salt; 2 tablespoons of honey or sugar +/- 1/2 cup OJ or mashed banana to taste
If patient can not tolerate PO, consider:
- Proctoclysis. Patient is placed lateral decubitus, and buttocks is elevated with towels/sheets. Then infuse 100-200cc/hr of fluid into rectum via 22F lubricated NG or foley catheter, placed 10-40cm deep. Fluids must be warmed, as cold fluids may cause expulsion reaction.
- Hypodermoclysis- A needle is inserted into a subQ space to infuse fluid. Can infuse up to 3L/day via this route into the subQ tissue. NS is fluid of choice as it must be isotonic (or close to it). Can infuse at about 1cc/min at this rate.
Intraperitoneal infusion - Can infuse up to 40-70cc/kg intraperitoneally, and within about 4 hours the body will absorb this fluid. Can also infuse 25-50cc/kg blood products this way.
Wound Management in Resource Limited Settings
Goals of wound management: hemorrhage control with minimized discomfort and maintaining functionality/cosmesis.
Tourniquet on the fly - Will need a rope/belt/cloth, with a windlass (can be a stick, anything strong enough to hold traction)
- Wrap cloth around extremity, tying one knot against the skin
- Then place the windlass over our first knot, tying the cloth in two additional knots over the windlass
- You now can utilize the windlass for torque in your tourniquet
Other options to consider:
- A BP cuff at about 200mmHg should tamponade most bleeding, can use hemostats along the chords if need help clamping off.
- For finger laceration, can apply small glove cutting tip off, then rolling down to the MCP fashioning a finger tourniquet.
Hair apposition technique - for scalp lacerations, tie multiple hair knots along laceration with hair from opposing sides to close scalp lac.
R2 Case Follow Up with Dr. Soria
Call: Young male patient found after electrocution when ladder he was carrying hit a wire, now down.
EMS timeline: V fib-> shock -> asystole -> shock -> v tach -> shock x2 -> ROSC.
- When exposed to alternating current (AC), most outlets and overhead wires people are exposued to, tissue damage is caused when electrical energy is converted to thermal energy. Muscles, nerves, vasculature are most often damaged.
Physical Injuries require:
- 10 mA for muscle tetany
Nervous system effects require:
- 30 mA for respiratory paralysis
- 75 mA for v fib
- 4 amps causes cardiac paralysis
Immediate effects: arrhythmia, respiratory arrest, seizures, compartment syndrome/rhabdo
Subacute effects: cataracts and hearing loss.
Electrocution Workup:
- EKG, CBC, CMP, lactate, trop, CK, u/a
- D/C asymptomatic patient with normal EKG and suffered less than 1000V injury
- Admit high voltage injuries >1000V (even asymptomatic), documented LOC, cardiac disease or CAD
R4 Follow Up with Dr. Riddle
Case: Middle aged male with chest pain
- Vitals: HR 43; RR 22; BP 120s, Afebrile
Pt feels like he got "hit in the chest with hammer” and is also having shortness of breath
- PMHx: HTN, HIV, amphetamine abuse
- Meds: ARV, aspirin, lisinopril
Cardiology was called, and wants a troponin resulted before management decision. It is ordered and returns 8.76.
Cardiology takes patient to cath which demonstrates non obstructive CAD. Apical ballooning c/w takotsubo’s cardiolmyopathy. UDS returns +cocaine
Takotsubo’s Cardiomyopathy
- Named after the “octopus trap”, to reflect the apical ballooning.
- Most commonly in post menopausal women (90% of cases)
Patient's present with CP, dyspnea, syncope, and can develop signs of heart failure. There is an association with stress (both physical - more common in men; and emotional - more common in women). 10% of patients go on to develop cardiogenic shock. Most patients generally recover LV function in 2-8 weeks, but 20% develop chronic CHF.
Dx criteria:
- Transient LV systolic dysfunction
- Absence of obstructive CAD
- New EKG abnormalities (ST segment elevation or TWI) or elevation in troponin
- Absence of pheochromocytoma or myocarditis
A word about cocaine:
- The UDS tests for a metabolite of cocaine (called benzoylecgonine). There are no drugs known to cause false positives for benzoylecgonine, so a +UDS indicates cocaine exposure within 5 days at maximum.
- Cocaine has also been associated with Coronary Artery Aneurysm (30% of patients compared to 1% at baseline!) - so beware chest pain in the patient who uses cocaine!