Grand Rounds Recap 8/24
/Mortality and Morbidity with Dr. Jon McKean
Case#1: Novel oral anticoagulant reversal with PCCs
HPI: Unknown age male on Xeralto for afib with fall from standing height. GCS of 14 initially with a rapid decline to 8 and then 3 in route, intubated in the field and given hypertonic saline. Arrives with stable vital signs, unequal pupils and signs of head trauma only. His GCS is 1T1. Found to have L SDH, given FFP and PCCs. Repeat CT shows worsening of the SDH and patient declared brain dead after multiple imaging studies. Fact: Can’t use CTA as official brain death exam because it is dependent on Left ventricular outflow, which you cannot quantify.
Reversal of Rivaroxaban and Dabigatran by PCCs: Healthy subjects were given the drugs and then labs were drawn, then they were given PCCs and labs were re-checked. Showed PCCs reversed the PT/PTT but not bleeding time after punch biopsy.
Patients on NOACs with bleeding: 18 patients with life threatening bleed given PCCS-- 6 surviving with good neurological recovery. 1 thromboembolic event in those patients that lived. 50% of those that survived did well neurologically.
Time dependent NOAC questions:
- Last dose within past 2 hours? Consider charcoal
- Last dose >12h ago (or 24h if CrCl is <50ml/min)? Drug may not be active anymore, consider not using PCCs as they may not be needed
Nuggets:
- Fear the anticoagulated minor trauma.
- Go to great lengths for history on these patients
- Ask your pharmacists for help, they know these studies well!
Case Series #2: Resuscitative Thoracotomy
Case #2.1: Multiple gunshot wounds to the chest pulses lost in the field, no cardiac activity on bedside US, stopped resuscitation.
Case #2.2: Multiple gunshot wounds, pulses lost in the field, +cardiac activity on bedside US, blood product, re-US and no cardiac activity, stopped resuscitation
Case#2.3: MCC with loss of pulses in the field, finger thoracotomies and bedside US with no cardiac activity, stopped resuscitation
Bedside ECHO as predictor of outcomes after resuscitative thoracotomy. The FAST was considered positive if effusion or cardiac activity. No one that was FAST neg survived to hospital discharge. Four FAST positive patients lived to hospital discharge.
Can cut resuscitative thoracotomy by 59% if you don't do one on patients who have no cardiac activity on bedside ECHO. Can also cut time of resuscitation down: with bedside ultrasound teams performed an average of 13.7mins of resuscitation. Without bedside ultrasound, teams performed an average of 37.9mins of resuscitation.
Case #3: AMA Documentation
Patient is a female in her 60s with a history of idiopathic pericardial effusion comes to the ED with shortness of breath and chest pain. +travel history and leg swelling. Cardiomegaly on CXR, pericardial effusion on bedside US and CT. Patient leaves AMA with good deocumentation.
Patient told to go back to the ED multiple times. Has some mild tachycardia and tachypnea and gets 600cc drained off.
What did physicians actually remember to document for patients who are leaving AMA?
- Capacity: 22%
- Signs/symptoms: 33%
- Extent and limitation of evaluation: 8.1%
- Current treatment plan: 3.8%
- Foregoing treatment: 4.8%
- Alternatives: 5.7%
- Explicit statement about why patient left AMA 50.7%
CURVES
- Communicate: Is the patient able to choose and communicate a choice?
- Understand: Does the patient understand the risks/benefits/and alternatives?
- Reason: Can the patient make a rational choice
- Value: Is the choice consistent with the patient’s values?
- Emergency: Is there impending risk to the patient?
- Surrogate: Are there surrogates or allies available?
Case #4 Rectal Bleeding
A male patient in his 30s with Hemophilia B who presents with rectal bleeding, hemodynamically stable. Guiac positive stool, hemorrhoids, then discharged home. Returns 12h later with similar complaints and presentation. He dropped 1 point of hemoglobin, Factor 9 activity lower than patients baseline. Admitted for factor replacement.
Hemophilia A: lack of factor VIII
Hemophilia B: lack of factor IX
Severity of Disease
- Severe <1%
- Moderate 1-10%
- Mild >10%
Emergent full reversal: ICH, retrobulbar hematoma, epidural hematoma, and hemorrhagic shock
Less emergent: hemarthrosis, muscle hematoma (be concerned for compartment syndrome)
To reverse:
- Hemophilia A: give Factor VIII, cyroprecipitate, DDAVP (mild disease to release more factor VIII from the endothelia)
- Hemophilia B: Factor IX, FFP, K-centra
Patients with Inhibitors: Hemophilia A>Hemophilia B; Severe > Mild/Moderate; Low responder vs high responder
Treatment options: personalized, overpower inhibitors
Nuggets:
- Treat a compartment which is under pressure aggressively
- Phone a friend
- If no specific factor available: Hemophilia A: cryo Hemophilia B: FFP
Case #5 Leukocytosis in an ESRD patient:
Patient is younger male with ESRD, type I DM, and known dry gangrene of the penis who presents initially with penis pain, unchanged from previous. Stable from both a hemodynamic stand point and then found to have a WBC of 21 without change in exam, so was discharged home. Presents 2 days later with DKA, NSTEMI and hyperkalemia, managed in the SRU and then sent to the MICU for management.
Pay attention to lab abnormalities, even if its a not a lab that you wanted in the first place. In your documentation, explain the lab abnormailty, not why it was ordered in the first place.
Case #6 Gangrenous Cholecystitis
Patient is a male with h/o of diabetes, HTN, and HLD presents with LUQ pain and nausea. Pain proceeding nausea. Discharged home after stable labs. Returns with same. Labs show leukocytosis. CT shows acute cholecystitis, OR course shows gangrenous cholecystitis.
N/v, fever more likely with gangrenous cholecystitis—> have a high index of suspicion
Infective endocarditis with Dr. Jeremy Leibman
HPI: Young male with HA, mildly hypotensive and tachycardia, uncomfortable. Sudden onset, 1 week ago, and now waxing and waning. Exam only significant for track markers and slow response/need for re-direction. CT head shows SAH and small infarcts in the L parietal lobe and L cerebellum, LP shows RBCs that do not clear. Gets admitted to neurology and during his work up is show to have a huge vegetation on his aortic valve and a blown aortic valve. Cardiac surgery replaced valve.
Neurological manifestations of infective endocarditis (IE):
- Stroke: 0.5% risk of stroke occurrence/day (80% ischemic, 20% hemorrhagic)
- Mycotic aneurysm: named for the mushroom like appearance of the vessel, bacteria attack from the adventitia. Large number appear in the MCA.
- Meningitis: in patients with neurological findings in IE only 30% have normal CSF. 30% of these patients have meningitis. If there is meningitis it usually indicates pneumococcal IE.
Patient had rothia dentocariosa: gram positive rod, normal oral flora, very rare. Usually affects those who already have valvular damage. Treated with amp for 6 weeks with an aminoglycoside for the first 2 weeks.
Brief Resolved Unexplained Events with Dr. Jared Ham
BRUEs were formerly known as ALTE (apparent life threatening event)
Definition of BRUE: In infants under 1 year old who have the following:
- Change in color (has to be central cyanosis, acrocyanosis does not count)
- Change in breathing
- Change in tone
- Change in mental status
AND has to be less than 60 seconds, completely resolved, and back to baseline with no potential cause on found on history and physical exam
Differential:
- GI: GERD
- Respiratory
- NAT
- Congenital heart disease
- Seizures
- Toxic Injestion
Low Risk infants fit all of the following criteria:
- >60 days old
- Born at greater 32 wks
- No CPR by trained medical provider
- 1st event
For every low risk patient you should do the following before sending them home:
- Shared decision making
- CPR training for parents
You could consider doing the following (for those on the conservative side):
- EKG
- Monitor on pulse ox for a few hours
You need not do the following for low risk patients:
- Respiratory viral panels
- Neuroimaging
- Admission for monitoring
You should not do the following for low risk patients:
- Serum labs
- Home Cardio/respiratory monitoring
- Initiating anti-seizure medications
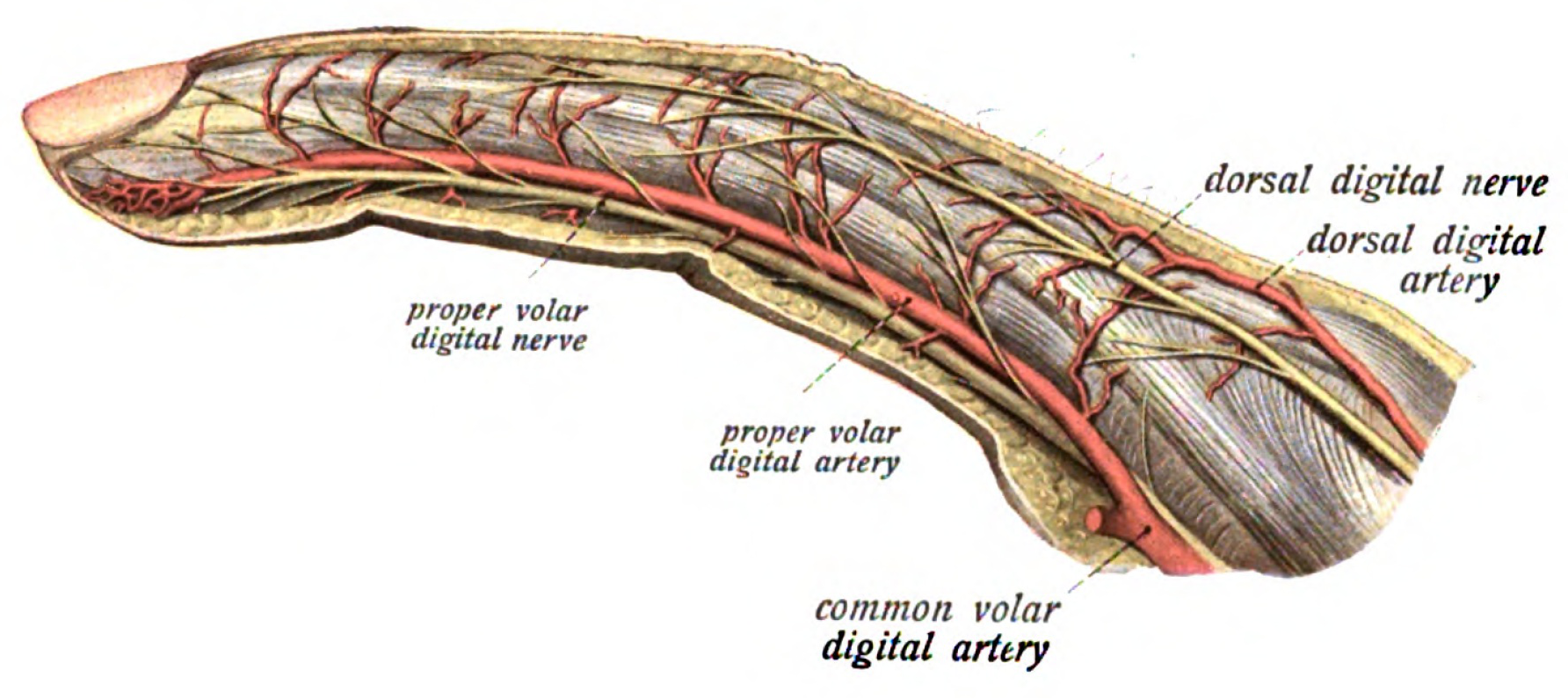
Discharge, Transfer or Admit: Hand Injuries with Dr. Roche
Bottom line:
- Distal tip amputations: consider fixing yourself if there is generous tissue available; minimal bone exposure. Leave it alone if <1cm tissue without bone exposed
- Tendon Lacerations: consider fixing extensor tendon lacerations that are on top of the metacarpals
- Open Fractures (tuft fracture with nail bed laceration): consider fixing if there is minimal contamination; stable reduction
When thinking about repair, consider Complication Reduction v Function Preservation:
- Establish baseline function
- Will the patient be able to work if repair is less than optimal?
- Will the patient be able to continue recreation?
Aggressive Repair:
- improved cosmoses and function
- may increase infection risk
- potential for worse outcomes
Thinks you wake a up a hand surgeon for at 2am:
- question of replantation
- highly contaminated open fracture/tendon
- rapidly evolving deep space infection
Things you discuss with a hand surgeon before disposition:
- complete flexor tendon laceration
- distal tip amp that needs revision vs grafting vs flap repair
- irreducible dislocations/fractures
- deep space infections (flexor tenosynovitis, cat bites, deep shooter abscesses)
Things that can wait the weekend until they see a hand surgeon:
- partial (<50%) flexor tendon injury
- extensor tendon injury
- closed tendon rupture (except mallet finger)
- irrigated/splinted open fractures
- fight bite
Fingertip Amputation:
- <1cm without exposed bone heals better with conservative management (4-8 weeks of dressing changes)
- >1cm may benefit from grafting
- Exposed Bone: consider ED closure if adequate tissue
Goals of amputation repair:
- restore a painless digit
- preserve function
- protect sensation
- preserve length
Complications include:
- nail deformity (hook nail)
- painful neuromas
- insensate digits
Replantation:
- Indications for replantation include: young children, single digit proximal to FDS insertion, thumb or multiple digits
- Relative contraindications: crush or avulsion/mangled/multiple levels, prolonger ischemia (>24h), smokers/diabetics/vasculopaths
Tendon Injuries:
- Partial flexor injury: splint and urgently referred
- Consider wound extension for inspection (extensors only)
- Roll stitch for zone 1(2) injuries
Central slip rupture/laceration:
Close the skin, splint wrist to PIP—> Urgent Referral
May need repair if >50% laceration
5.0 non-absorbable sutures, consider fight bite in zone 5, zone 6
Flexor Tendon Injury
- assume injury, high miss rate
- when in doubt, splint and have follow up with hand surgery
Nail Bed Injury
Subungal hematomas with trephination, do not remove the nail unless: nail not adhered to bed, displaced tuft fracture, damage to nail folds
Nail Bed Repair: super frustrating, glue works just as well. Don't glue nail back on, fix underlying nail bed with glue, let dry, and then replace the nail
ImpostOr Phenomenon with Dr. Riley Grosso
Impostor Phenomenon - first identified in 1978 in a study of 150 highly successful women and refers to the the sensation of intellectual phoniness despite high achievements.
Success is attribute to a temporary cause. “I was lucky.”
- Failure is attributed to ability. “I am not very good at this job.”
Dunning-Krueger effect: Those with the least competence are the most confident. (Essentially the opposite of impostor syndrome.)
Patterns of people with impostor syndrome:
- Fear of discovery -> hard work -> excellence -> temporary good feeling -> fear of discovery. Anxiety leads to over preparation or alternatively procrastination.
- Telling your superiors want they want to hear to get positive feedback.
- Using charm and perceptiveness to win over superiors/mentors.
- Teacher’s Pet
“As iron sharpens iron, so one man sharpens another.”: you cannot get better if you are not surrounded by people who are better than you.
Demonstrating confidence and competence increases patient’s trust and the likelihood that they will follow recommendations and discharge instructions.
Techniques to combat impostor phenomenon: Reframe your thinking in terms of success versus failure. Role play scenarios in which you are perceived as competent and intelligent.